Abstract
Objective:
To determine if metabolite ratios at near-term age predict outcome in very low birth weight preterm infants at 18 to 24 months adjusted age.
Study Design:
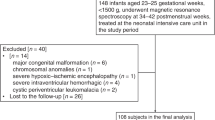
Thirty-six infants (birth weight ⩽1510 g, gestational age ⩽32 weeks) were scanned at a postmenstrual age (PMA) of 35 to 43 weeks from July 2001 to September 2003. Multivoxel proton spectroscopic data were acquired and metabolite ratios were calculated in regions of the thalamus and basal ganglia. Bayley Scales of Infant Development were assessed between 18 and 24 months corrected age.
Result:
Metabolic ratios showed no significant correlation with developmental outcome. A correlation was seen between N-acetylaspartate (NAA)/choline (Ch) and PMA in thalamus and basal ganglia.
Conclusion:
Metabolite ratios from near-term proton magnetic resonance spectroscopy (MRS) were not predictive of Bayley scores at 18 to 24 months adjusted age. There was a positive correlation between NAA/Ch and PMA, which supports previous work by others for the importance of developmental changes in the MRS with age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Andreias L et al. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA 2005; 294: 318–325.
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M . Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 2005; 115: 997–1003.
Vohr BR, Wright LL, Dusick AM, Perritt R, Poole WK, Tyson JE et al. Center differences and outcomes of extremely low birth weight infants. Pediatrics 2004; 113: 781–789.
Hack M, Flannery DJ, Schluchter M, Cartar L, Borawski E, Klein N . Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med 2002; 346: 149–157.
Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. Pediatrics 2001; 107: E1.
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993 to 1994. Pediatrics 2000; 105: 1216–1226.
Ment LR, Bada HS, Barnes P, Grant PE, Hirtz D, Papile LA et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002; 58: 1726–1738.
Mirmiran M, Barnes PD, Keller K, Constantinou JC, Fleisher BE, Hintz SR et al. Neonatal brain magnetic resonance imaging before discharge is better than serial cranial ultrasound in predicting cerebral palsy in very low birth weight preterm infants. Pediatrics 2004; 114: 992–998.
Inder TE, Anderson NJ, Spencer C, Wells S, Volpe JJ . White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term. AJNR Am J Neuroradiol 2003; 24: 805–809.
Miller SP, Cozzio CC, Goldstein RB, Ferriero DM, Patridge JC, Vigneron DB et al. Comparing the diagnosis of white matter injury in premature newborns with serial MR imaging and transfontanel ultrasonography findings. AJNR Am J Neuroradiol 2003; 24: 1661–1669.
Cecil KM, Jones BV . Magnetic resonance spectroscopy of the pediatric brain. Topics Magn Reson Imaging 2001; 12 (6): 435–452.
Scarabino T, Popolizio T, Bertolino A, Salvolini U . Proton magnetic resonance spectroscopy of the brain in pediatric patients. European J Radiol 1999; 30: 142–153.
Babikian T, Freier MC, Ashwal S, Riggs ML, Burley T, Holshouser BA . MR spectroscopy: predicting long-term neuropsychological outcome following pediatric TBI. J Magn Reson Imaging 2006; 24: 801–811.
Filippi CG, Ulug AM, Deck MDF, Zimmerman RD, Heier LA . Developmental delay in children: assessment with proton MR spectroscopy. Am J Neuroradiol 2002; 23: 882–888.
Moore GJ . Proton magnetic resonance spectroscopy in pediatric neuroradiology. Pediatr Radiol 1998; 28: 805–814.
Kreis R, Hofmann L, Kuhlmann B, Boesch C, Bossi E, Hüppi PS . Brain metabolite composition during early human brain development as measured by quantitative in vivo 1H magnetic resonance spectroscopy. Magn Reson Med 2002; 48: 949–958.
Roelants-van Rijn AM, van der Grond J, Stigter RH, de Vries LS, Groenendaal F . Cerebral structure and metabolism and long-term outcome in small-for-gestational-age preterm neonates. Pediatr Res 2004; 56: 285–290.
Heerschap A, Kok RD, van den Berg PP . Antenatal proton MR spectroscopy of the human brain in vivo. Childs Nerv Syst 2003; 19: 418–421.
Khong PL, Tse C, Wong IY, Lam BC, Cheung PT, Goh WH et al. Diffusion-weighted imaging and proton magnetic resonance spectroscopy in perinatal hypoxic-ischemic encephalopathy: association with neuromotor outcome at 18 months of age. J Child Neurol 2004; 19: 872–881.
Kadri M, Shu S, Holshouser B, Deming D, Hopper A, Peverini R et al. Proton magnetic resonance spectroscopy improves outcome prediction in perinatal CNS insults. J Perinatol 2003; 23: 181–185.
Miller SP, Newton N, Ferriero DM, Partridge JC, Glidden DV, Barnwell A et al. Predictors of 30-month outcome after perinatal depression: role of proton MRS and socioeconomic factors. Pediatr Res 2002; 52: 71–77.
Barkovich AJ, Baranski K, Vigneron D, Partridge JC, Hallam DK, Hajnal BL et al. Proton MR spectroscopy for the evaluation of brain injury in asphyxiated, term neonates. Am J Neuroradiol 1999; 20: 1399–1405.
Shu SK, Ashwal S, Holshouser BA, Nystrom G, Hinshaw DBJ . Prognostic value of 1H-MRS in perinatal CNS insults. Pediatr Neurol 1997; 17: 309–318.
Groenendaal F, Veenhoven RH, van der Grond J, Jansen GH, Witkamp TD, de Vries LS . Cerebral lactate and N-acetyl-aspartate/choline ratios in asphyxiated full-term neonates demonstrated in vivo using proton magnetic resonance spectroscopy. Pediatr Res 1994; 35: 148–151.
Boichot C, Walker PM, Durand C, Grimaldi M, Chapuis S, Gouyon JB et al. Term neonate prognoses after perinatal asphyxia: contributions of MR imaging, MR spectroscopy, relaxation times, and apparent diffusion coefficients. Radiology 2006; 239: 839–848.
Amiel-Tison C . Neuromotor status. In: Taeusch H, Yogman M (eds). Follow-up management of the high-risk infant. Little, Brown and Company: Boston, 1987, pp 115–126.
Bayley N . The Bayley Scales of Infant Development II. New York Psychological Corporation: New York, 1993.
Zimmerman RA, Wang ZJ . The value of proton MR spectroscopy in pediatric metabolic brain disease. AJNR Am J Neuroradiol 1997; 18: 1872–1879.
Filippi CG, Ulug AM, Deck MD, Zimmerman RD, Heier LA . Developmental delay in children: assessment with proton MR spectroscopy. AJNR Am J Neuroradiol 2002; 23: 882–888.
Baslow MH . N-acetylaspartate in the vertebrate brain: metabolism and function. Neurochem Res 2003; 28: 941–953.
Govindaraju V, Young K, Maudsley AA . Proton NMR chemical shifts and coupling constants for brain metabolites. NMR Biomed 2000; 13: 129–153.
Robertson NJ, Kuint J, Counsell TJ, Rutherford TA, Coutts A, Cox IJ et al. Characterization of cerebral white matter damage in preterm infants using 1H and 31P magnetic resonance spectroscopy. J Cereb Blood Flow Metab 2000; 20: 1446–1456.
Cooke RW, Abernethy LJ . Cranial magnetic resonance imaging and school performance in very low birth weight infants in adolescence. Arch Dis Child Fetal Neonatal Ed 1999; 81: F116–F121.
Kugel H, Roth B, Pillekamp F, Kruger K, Schulte O, von Gontard A et al. Proton spectroscopic metabolite signal relaxation times in preterm infants: a prerequisite for quantitative spectroscopy in infant brain. J Magn Reson Imaging 2003; 17: 634–640.
Cheong JL, Cady EB, Penrice J, Wyatt JS, Cox IJ, Robertson NJ . Proton MR spectroscopy in neonates with perinatal cerebral hypoxic-ischemic injury: metabolite peak-area ratios, relaxation times, and absolute concentrations. Radiology 2006; 239 (3): 839–848.
Posse S, Tedeschi G, Risinger R, Ogg R, Le Bihan D . High speed 1H spectroscopic imaging in human brain by echo planar spatial-spectral encoding. Magn Reson Med 1995; 33: 34–40.
Adalsteinsson E, Irarrazabal P, Topp S, Meyer C, Macovski A, Spielman DM . Volumetric spectroscopic imaging with spiral-based k-space trajectories. Magn Reson Med 1998; 39: 889–898.
Vigneron DB, Barkovich J, Noworolski SM, von dem Bussche M, Henry RG, Lu Y et al. Three-dimensional proton MR spectroscopic imaging of premature and term neonates. Am J Neuroradiol 2001; 22: 1422–1424.
Kim DH, Barkovich AJ, Vigneron DB . Short echo time MR spectroscopic imaging for neonatal pediatric imaging. Am J Neuroradiol 2006; 27: 1370–1372.
Wald LL, Moyher SE, Day MR, Nelson SJ, Vigneron DB . Proton spectroscopic imaging of the human brain using phased array detectors. Magn Reson Med 1995; 34: 440–445.
Barnett A, Mercuri E, Rutherford M, Haataja L, Frisone MF, Henderson S et al. Neurological and perceptual-motor outcome at 5 to 6 years of age in children with neonatal encephalopathy: relationship with neonatal brain MRI. Neuropediatrics 2002; 33: 242–248.
Acknowledgements
EMA was an American Pediatric Society/Society for Pediatric Research Program Awardee and received NIH grant HD007446. EMA also received travel award and presented this work in Poster Session at the 2006 Pediatric Academic Society Meeting. We gratefully acknowledge support from NIH Grant RR 09784 and thank Roger B Baldwin for assistance with data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Augustine, E., Spielman, D., Barnes, P. et al. Can magnetic resonance spectroscopy predict neurodevelopmental outcome in very low birth weight preterm infants?. J Perinatol 28, 611–618 (2008). https://doi.org/10.1038/jp.2008.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.66
Keywords
This article is cited by
-
Neurometabolic changes in neonates with congenital heart defects and their relation to neurodevelopmental outcome
Pediatric Research (2023)
-
Brain proton magnetic resonance spectroscopy and neurodevelopment after preterm birth: a systematic review
Pediatric Research (2022)
-
Altered brain metabolite concentration and delayed neurodevelopment in preterm neonates
Pediatric Research (2022)
-
Magnetic resonance spectroscopy brain metabolites at term and 3-year neurodevelopmental outcomes in very preterm infants
Pediatric Research (2022)
-
The long-term effect of erythropoiesis stimulating agents given to preterm infants: a proton magnetic resonance spectroscopy study on neurometabolites in early childhood
Pediatric Radiology (2018)