Abstract
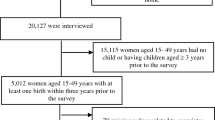
Inability to reduce neonatal and maternal mortality in poor countries is sometimes blamed on a lack of contextual knowledge about care practices and care-seeking behavior. There is a lack of knowledge about how to translate formative research into effective interventions to improve maternal and newborn health. We describe the findings of formative research and how they were used to inform the development of such an intervention in rural Nepal. Formative research was carried out in four parts. Part 1 involved familiarization with the study area and literature review, and parts 2, 3 and 4 involved community mapping, audit of health services, and qualitative and quantitative studies of perinatal care behaviors. Participatory approaches have been successful at reducing neonatal mortality and may be suitable in our context. Community mapping and profiling helped to describe the community context, and we found that community-based organizations often sought to involve the Female Community Health Volunteer in community mobilization. She was not routinely conducting monthly meetings and found them difficult to sustain without support and supervision. In health facilities, most primary care staff were in post, but doctors and staff nurses were absent from referral centers. Mortality estimates reflected under-reporting of deaths and hygiene and infection control strategies had low coverage. The majority of women give birth at home with their mother-in-law, friends and neighbors. Care during perinatal illness was usually sought from traditional healers. Cultural issues of shyness, fear and normalcy restricted women's behavior during pregnancy, birth and the postpartum period, and decisions about her health were usually made after communications with the family and community. The formative research indicated the type of intervention that could be successful. It should be community-based and should not be exclusively for pregnant women. It should address negotiations within families, and should tailor information to the needs of local groups and particular stakeholders such as mothers-in-law and traditional healers. The intervention should not only accept cultural constructs but also be a forum in which to discuss ideas of pollution, shame and seclusion. We used these guidelines to develop a participatory, community-based women's group intervention, facilitated through a community action cycle. The success of our intervention may be because of its acceptability at the community level and its sensitivity to the needs and beliefs of families and communities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Save the Children USA. State of the world's mothers 2006. Saving the lives of mothers and newborns. Save the Children: Westport Connecticut. www.savethechildren.org/publications/SOWM_2006_final.pdf 2006.
Knippenberg R, Lawn J, Darmstadt G, Begkoyian G, Fogstad H, Walelign N et al. Neonatal survival 3. Systematic scaling up of neonatal care in countries. Lancet 2005; 365: 1087–1098.
United Nations. Millennium Development Goals. www.un.org/millenniumgoalsAccessed 10/07/2004: United nations, 2004.
Bhutta Z, Darmstadt G, Hasan B, Haws R . Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics 2005; 115: 519–617.
Winch P, Alam M, Akther A, Afroz D, Ali NA, Ellis AA et al. Local understandings of vulnerability and protection during the neonatal period in Sylhet district, Bangladesh: a qualitative study. Lancet 2005; 366: 478–485.
Goodburn E, Rukhsana G, Chowdhury M . Beliefs and practices regarding delivery and postpartum maternal morbidity in rural Bangladesh. Stud Fam Plan 1995; 26: 22–32.
Essien E, Ifenne D, Sabitu K, Musa A, Alti-Mu’azu M, Adidu V et al. Community loan funds and transport services for obstetric emergencies in northern Nigeria. Int J Gynaecol Obstet 1997; 59 (Suppl 2): S237–S244.
Olaniran N, Offiong S, Ottong J, Asuquo E, Duke F . Mobilizing the community to utilize obstetric servicess, Cross River State, Nigeria. The Calabar PMM Team. Int J Gynaecol Obstet 1997; 59 (Suppl 2): S181–S189.
Howard-Grabman L, Snetro G . How to mobilize communities for health and social change. Health Communication Partnership, Johns Hopkins Population Information Program, Media/Materials Clearing House: Baltimore, 2003.
Borghi J, Thapa B, Osrin D, Jan S, Morrison J, Tamang S et al. Economic assessment of a women’s group intervention to improve birth outcomes in rural Nepal. Lancet 2005; 366: 1882–1884.
Manandhar D, Osrin D, Shrestha B, Mesko N, Morrison J, Tumbahangphe KM et al. Effect of a participatory intervention with women′s groups on birth outcomes in Nepal: cluster randomized controlled trial. Lancet 2004; 364: 970–979.
Ministry of Health and Population. Nepal Demographic and Health Survey 2006. Population Division, Ministry of Health and Population, Government of Nepal; New ERA; MEASURE DHS; ORC Macro: Kathmandu and Calverton MA, 2007.
Nepal Research Associates. Makwanpur District Profile: District Development Committee, 1999.
Manandhar M . Makwanpur baseline survey. Unpublished MSc thesis. Institute of Child Health, University College London: London, 1998.
Osrin D, Tumbahangphe K, Shrestha D, Mesko N, Shrestha BP, Manandhar MK et al. Cross sectional, community based study of care of newborn infants in Nepal. Br Med J 2002; 325: 1063–1066.
Tamang S, Mesko N, Shrestha BP, Osrin D, Manandhar MK, Standing H et al. A qualitative description of perinatal care practices in Makwanpur district, Nepal. Contr Nepalese Stud 2001; 28: 10–19.
Mesko N, Osrin D, Tamang S, Shrestha BP, Manandhar DS, Manandhar M et al. Care for perinatal illness in rural Nepal: a descriptive study with cross-sectional and qualitative components. BMC Int Health Hum Rights 2003; 3 (3): 3.
Bang A, Bang R, Baitule S, Reddy M, Deshmukh M . Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999; 354: 1955–1961.
West K, Katz J, Khatry S, LeClerq SC, Pradhan EK, Shrestha SR et al. Double blind, cluster randomised trial of low dose supplementation with vitamin A or beta carotene on mortality related to pregnancy in Nepal. BMJ 1999; 318: 570–575.
Howard-Grabman L, Seoane G, Davenport C . Mother Care and Save the Children. The Warmi Project: a participatory approach to improve maternal and neonatal health, an implementor’s manual. Westport: John Snow International, Mothercare Project, Save the Children 2002.
O’Rourke K, Howard Grabman L, Seoane G . Impact of community organization of women on perinatal outcomes in rural Bolivia. Rev Panam Salud Publica/Pan Am Public Health 1998; 3: 9–14.
Bolam A, Manandhar D, Shrestha P, Malla K, Ellis M, Costello A . The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised, controlled trial. Br Med J 1998; 134: 805–810.
Pratt G . Practitioners’ critical reflections on PRA and participation in Nepal. Institute of Development Studies, University of Sussex: Brighton, 2000.
Hobley M . From passive to active participatory forestry. Nepal In: Oakley P (ed). Projects with People: the Practice of Participation in Development. International Labour Organisation: Geneva, 1990, pp 107–118.
Hobley M . Participatory forest management in South Asia: The Process of Change in India and Nepal (Rural Development Forestry Study Guide). Overseas Development Institute (ODI): London, 1996.
Zakus D, Lysack C . Revisiting community participation. Health Policy Plan 1998; 13 (1): 1–12.
Morgan L . Community participation in health: perpetual allure, persistent challenge. Health Policy Plan 2001; 16: 221–230.
Rifkin S . Community Participation in Maternal and Child Health/Family Planning Programmes. World Health Organization: Geneva, 1990.
Chambers R . Whose Reality Counts? Putting the First Last. Intermediate Technology Publications: London, 1997.
Freire P . Pedagogy of Hope: Reliving Pedagogy of the Oppressed. Continuum International Publishing Group: New York, 1995.
De Koning K, Martin M . Participatory research in health: setting the context In: de Koning K, Martin M (eds). Participatory Research in Health: Issues and Experiences. Zed Books: London, 1996, pp 1–18.
Morrison J, Tamang S, Mesko N, Osrin D, Shrestha B, Manandhar M et al. Women’s health groups to improve perinatal care in rural Nepal. BMC Pregnancy Childbirth 2005; 5 (1): 6.
Manandhar M . Birthing Practices Study. Remote Area Basic Needs Project—Bajura. CARE Nepal: Kathmandu, 1999.
Levitt M . A Systematic Study of Birth and Birth Attendants in Nepal. John Snow International: Kathmandu, 1993.
Dawson P . Report on Female Community Health Volunteers’ Knowledge and Activities Related to Diarrhoeal Diseases and Acute Respiratory Infections. John Snow International; Government of Nepal Ministry of Health: Kathmandu, 1998.
Child Health Division. Assessment of the ARI Strengthening Program. Department of Health Services, Government of Nepal Ministry of Health; WHO; USAID; UNICEF: Kathmandu, 1997.
Bennett L . Dangerous Wives and Sacred Sisters. Mandala Book Point: Kathmandu, 1983.
Erickson N . What Health Care When? A Literature Review and Fieldwork Study of Low-caste Women’s Health Care Decision-Making. Save the Children: Kathmandu, 1995.
Pigg S . Here, there and everywhere: place and person in Nepalese explanations of illness. Him Res Bull 1989; 9 (2): 16–24.
Stone L . Concepts of illness and curing in a central Nepal village. Contrib Nepalese Stud 1996; 18: 55–80.
Acknowledgements
We offer particular thanks to all senior field supervisors, Kunta Dahal and Naomi Saville. We also thank the many individuals in Makwanpur District who gave their time generously and without complaint. The study was funded by the British Government Department for International Development, UNICEF Nepal and the Department of Child and Adolescent Health and Development, World Health Organization.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure
The authors have declared no financial interests.
Rights and permissions
About this article
Cite this article
Morrison, J., Osrin, D., Shrestha, B. et al. How did formative research inform the development of a women's group intervention in rural Nepal?. J Perinatol 28 (Suppl 2), S14–S22 (2008). https://doi.org/10.1038/jp.2008.171
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.171
This article is cited by
-
Illness recognition and care seeking for maternal complications of pregnancy and birth in rural Amhara and Oromia Regional States of Ethiopia
BMC Pregnancy and Childbirth (2017)
-
Recognition of and care-seeking for maternal and newborn complications in Jayawijaya district, Papua province, Indonesia: a qualitative study
Journal of Health, Population and Nutrition (2017)
-
Lower mortality is observed among low birth weight young infants who have received home-based care by female community health volunteers in rural Nepal
BMC Pregnancy and Childbirth (2017)
-
Methodology for a mixed-methods multi-country study to assess recognition of and response to maternal and newborn illness
Journal of Health, Population and Nutrition (2017)
-
Re-imagining adherence to treatment from the “other side”: local interpretations of adverse anti-malarial drug reactions in the Peruvian Amazon
Malaria Journal (2016)