Abstract
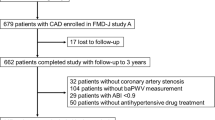
The impact of target organ damage (TOD) clustering in hypertensive patients with established cardiovascular disease has not been clearly defined. Multicentre, observational and prospective study of 1054 consecutive patients with acute coronary syndromes (ACSs). The objective was describing the impact of TOD on first-year mortality. Ankle–brachial index (ABI), left ventricular hypertrophy and renal dysfunction were assessed during hospital stay. Hypertensive patients accounted for 80% of the cohort and had slightly higher mean age, higher prevalence of risk factors, previous cardiovascular disease and TOD. During follow-up, mean time 387.9 (7.2) days and median 382 (364.0–430.0) days, mortality rate tended to be higher in hypertensive patients (6.1 versus 3.5%; P=0.16). Cox regression survival analysis identified pathological ABI as the only TOD independently associated with mortality. When assessed globally, the presence of at least one TOD predicted mortality only in patients with hypertension and differences in mortality rate appeared very early in the follow-up. A linear increase in mortality rate was observed with the clustering of TOD: 2.0%, if no TOD was present, 7.6% in one TOD, 11.1% in two TODs and 20.0%, if three TODs were present. An increased risk in the combined end point of ischaemic events was observed in hypertensive patients without TOD (odds ratio (OR): 3.18; 95% confidence interval (CI): 1.31–7.70; P=0.01) and was still higher in patients with hypertension and TOD (OR: 4.61; 95% CI: 1.90–11.80; P<0.01). TOD predicts mortality and ischaemic events of hypertensive patients after ACS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Egan BM, Zhao Y, Axon RN . US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303: 2043–2050.
Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006; 295: 180–189.
Kotseva K, Wood D, De BG, De BD, Pyorala K, Keil U . Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009; 373: 929–940.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Gonzalez-Juanatey JR, Cea-Calvo L, Bertomeu V, Aznar J . Electrocardiographic criteria for left ventricular hypertrophy and cardiovascular risk in hypertensives. VIIDA study. Rev Esp Cardiol 2007; 60: 148–156.
Verdecchia P, Sleight P, Mancia G, Fagard R, Trimarco B, Schmieder RE et al. Effects of telmisartan, ramipril, and their combination on left ventricular hypertrophy in individuals at high vascular risk in the Ongoing Telmisartan Alone and in Combination With Ramipril Global End Point Trial and the Telmisartan Randomized Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease. Circulation 2009; 120: 1380–1389.
Liao Y, Cooper RS, McGee DL, Mensah GA, Ghali JK . The relative effects of left ventricular hypertrophy, coronary artery disease, and ventricular dysfunction on survival among black adults. JAMA 1995; 273: 1592–1597.
Hawkins NM, Wang D, McMurray JJ, Pfeffer MA, Swedberg K, Granger CB et al. Prevalence and prognostic implications of electrocardiographic left ventricular hypertrophy in heart failure: evidence from the CHARM programme. Heart 2007; 93: 59–64.
Verdecchia P, Angeli F, Borgioni C, Gattobigio R, de SG, Devereux RB et al. Changes in cardiovascular risk by reduction of left ventricular mass in hypertension: a meta-analysis. Am J Hypertens 2003; 16: 895–899.
Verdecchia P, Reboldi G, Angeli F, Avanzini F, de SG, Pede S et al. Prognostic value of serial electrocardiographic voltage and repolarization changes in essential hypertension: the HEART Survey Study. Am J Hypertens 2007; 20: 997–1004.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY . Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004; 351: 1296–1305.
Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med 2004; 351: 1285–1295.
Matsushita K, Van DV, Astor BC, Woodward M, Levey AS, de Jong PE et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 2073–2081.
Luo YY, Li J, Xin Y, Zheng LQ, Yu JM, Hu DY . Risk factors of peripheral arterial disease and relationship between low ankle brachial index and mortality from all-cause and cardiovascular disease in Chinese patients with hypertension. J Hum Hypertens 2007; 21: 461–466.
Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE et al. Ankle brachial index combined with Framingham risk score to predict cardiovascular events and mortality: a meta-analysis. JAMA 2008; 300: 197–208.
Hackam DG, Sultan NM, Criqui MH . Vascular protection in peripheral artery disease: systematic review and modelling study. Heart 2009; 95: 1098–1102.
Bertomeu V, Morillas P, Gonzalez-Juanatey JR, Quiles J, Guindo J, Soria F et al. Prevalence and prognostic influence of peripheral arterial disease in patients >or=40 years old admitted into hospital following an acute coronary event. Eur J Vasc Endovasc Surg 2008; 36: 189–196.
Morillas P, Cordero A, Bertomeu V, Gonzalez-Juanatey JR, Quiles J, Guindo J et al. Prognostic value of low ankle-brachial index in patients with hypertension and acute coronary syndromes. J Hypertens 2009; 27: 341–347.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39: 1–266.
Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation 2004; 109: 733–739.
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006; 113: e463–e654.
Morillas P, Quiles J, Cordero A, Guindo J, Soria F, Mazon P et al. Impact of clinical and subclinical peripheral arterial disease in mid-term prognosis of patients with acute coronary syndrome. Am J Cardiol 2009; 104: 1494–1498.
Bertomeu V, Facila L, Gonzalez-Juanatey JR, Cea-Calvo L, Aznar J, Mazon P et al. Blood pressure control in hypertensive patients with left ventricular hypertrophy. The VIIDA Study. Rev Esp Cardiol 2007; 60: 1257–1263.
Huelmos A, Jimenez J, Guijarro C, Belinchon JC, Puras E, Sanchez C et al. Underrecognized peripheral arterial disease in patients with acute coronary syndrome: prevalence of traditional and emergent cardiovascular risk factors. Rev Esp Cardiol 2005; 58: 1403–1410.
Agnelli G, Cimminiello C, Meneghetti G, Urbinati S . Low ankle-brachial index predicts an adverse 1-year outcome after acute coronary and cerebrovascular events. J Thromb Haemost 2006; 4: 2599–2606.
Facila L, Bertomeu-Gonzalez V, Bertomeu V, Gonzalez-Juanatey JR, Mazon P, Morillas P . Importance of recognizing occult renal disease in hypertensive patients. Rev Esp Cardiol 2009; 62: 282–287.
de Simone G, Pasanisi F, Contaldo F . Link of nonhemodynamic factors to hemodynamic determinants of left ventricular hypertrophy. Hypertension 2001; 38: 13–18.
Mehta SK, Rame JE, Khera A, Murphy SA, Canham RM, Peshock RM et al. Left ventricular hypertrophy, subclinical atherosclerosis, and inflammation. Hypertension 2007; 49: 1385–1391.
Leenen FH, Yuan B . Mortality after coronary artery occlusion in different models of cardiac hypertrophy in rats. Hypertension 2001; 37: 209–215.
Galderisi M, de Simone G, D'Errico A, Sidiropulos M, Viceconti R, Chinali M et al. Independent association of coronary flow reserve with left ventricular relaxation and filling pressure in arterial hypertension. Am J Hypertens 2008; 21: 1040–1046.
Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F . Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension 2000; 35: 580–586.
Franklin SS, Lopez VA, Wong ND, Mitchell GF, Larson MG, Vasan RS et al. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation 2009; 119: 243–250.
Kennedy M, Solomon C, Manolio TA, Criqui MH, Newman AB, Polak JF et al. Risk factors for declining ankle-brachial index in men and women 65 years or older: the Cardiovascular Health Study. Arch Intern Med 2005; 165: 1896–1902.
Bayturan O, Kapadia S, Nicholls SJ, Tuzcu EM, Shao M, Uno K et al. Clinical predictors of plaque progression despite very low levels of low-density lipoprotein cholesterol. J Am Coll Cardiol 2010; 55: 2736–2742.
Acknowledgements
The PAMISCA Study has an unrestricted grant of Sanofi-Aventis Spain.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cordero, A., Morillas, P., Bertomeu-Gonzalez, V. et al. Clustering of target organ damage increases mortality after acute coronary syndromes in patients with arterial hypertension. J Hum Hypertens 25, 600–607 (2011). https://doi.org/10.1038/jhh.2010.109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2010.109