Abstract
We investigated the relationship between gonadotropin-releasing hormone receptor (GnRHR) gene polymorphisms and outcome of patients with polycystic ovary syndrome (PCOS) undergoing in vitro fertilization and embryo transfer (IVF-ET). PCOS patients undergoing IVF-ET were selected, and infertile patients due to dysfunctional oviducts served as controls. GnRHR gene polymorphisms were detected using the polymerase chain reaction-restriction fragment length polymorphism assay. Gene–gene interaction and linkage disequilibrium tests were performed using the SHEsis software. Logistic regression analysis was performed to evaluate factors affecting outcome of patients undergoing IVF-ET. The PCOS group showed more patients with CC+CT genotypes rs12644822, rs3756159 and rs13138607 than the control group, and CC+CT genotypes and C alleles from three positions enhanced risk of PCOS. Patients with CC+CT genotypes from three positions exhibited increased serum luteinizing hormone (LH), LH/follicle-stimulating hormone (FSH), testosterone (T) and follicles than those with TT genotypes. The haplotype analysis indicated that CCC, CCT and TCC haplotypes increased the risk of PCOS, while TCT, TTC and TTT haplotypes lowered the risk. After IVF-ET treatment, patients with CC+CT genotypes of three positions in the GnRHR gene had a lower pregnancy rate than patients with TT genotypes. Logistic regression analysis indicated that CC+CT genotypes rs12644822, rs3756159 and rs13138607 were risk factor for patients undergoing IVF-ET. In conclusion, these findings demonstrate that CC+CT genotypes rs12644822C>T, rs3756159C>T and rs13138607C>T in the GnRHR gene may contribute to a decreased pregnancy rate for PCOS patients after IVF-ET.
Similar content being viewed by others
Introduction
Polycystic ovary syndrome (PCOS) is often characterized by hyperandrogenism, hyperinsulinemia, insulin resistance, ovulatory dysfunction and polycystic ovaries. It is a complex and heterogeneous disorder that occurs in reproductive aged women. It can lead to defects in reproduction and metabolism.1, 2 The prevalence of PCOS is estimated to be as high as 15–20% according to the European Society for Human Reproduction and Embryology and American Society for Reproductive Medicine.3 PCOS has a complex and unclear pathogenesis and risk factors, including obesity, genetics and early childhood growth patterns.1, 4, 5 According to a prior meta-analysis, women with PCOS face an elevated risk of developing serious pregnancy complications such as preeclampsia and pregnancy-induced hypertension.2, 6 Furthermore, PCOS is reported to be the most common factor for anovulatory infertility and is responsible for women pursuing fertility treatment.7 PCOS also leads to long-term metabolic complications such as obesity, diabetes and cardiovascular disease.1 Studies show that women with PCOS are more likely to have increased coronary artery calcium scores and increased carotid intima–media thickness.8, 9 It is believed that proper diagnosis and treatment of PCOS is essential in preventing future endocrine, metabolic and cardiovascular complications.3
Gonadotropin (Gn)-releasing hormone receptor (GnRHR) is a member of the G-protein-coupled receptors (GPCRs) and is mainly expressed in the gonadotrope membrane of the anterior pituitary.10, 11 The binding of GnRH, GnRHR-associated G proteins, can activate several signaling cascades downstream including the inositol 1,4,5-triphosphate, mitogen-activated protein kinases, diacylglycerol and adenylyl cyclase pathways.12 The expression of GnRH and its receptor has been clearly observed in numerous extrapituitary tissues such as cancer cell lines, ovary, placenta, breast and so on.13 However, the effects of GnRHR on extrapituitary tissues, particularly the ovary, remain ambiguous. The high prevalence of PCOS was found in family lines suggesting a genetic etiology.14 Furthermore, PCOS has a complicated and uncertain pathogenesis and is inherently difficult to study genetically.4 In the present study, we discuss the relationship between GnRHR gene polymorphisms, steroid hormones and the outcome of IVF-ET in patients with PCOS. Finally, we hypothesized a molecular basis for the therapeutic function of IVF-ET.
Materials and methods
Ethics statement
This study was approved by the Ethics Committee of Linyi Cancer Hospital. All patients signed informed consent forms.
Study subjects
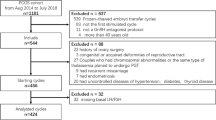
From 2012 to 2014, 634 cases of infertility patients underwent IVF-ET at the Linyi Cancer Hospital. A total of 314 of these cases were recruited as the PCOS group, and the remaining 320 non-PCOS cases who received IVF-ET treatment at the Linyi Cancer Hospital were treated as the control group. The inclusion criteria15 for the PCOS group were: (1) female aged between 21 and 38 years old; (2) infertile patients diagnosed with PCOS or PCOS complicated with tubal factor; (3) patients able to ovulate after follicle-stimulating hormone (FSH) treatment. Inclusion criteria for the control group were: (1) infertility caused by dysfunctional oviducts; (2) patients with regular menstrual cycle and normal endocrine parameters; (3) patients have no clinical manifestation or biological/chemical performance of hyperandrogenism; (4) patients have no manifestation of polycystic ovaries under mode-B ultrasonography. The exclusion criteria for both PCOS and control groups were: (1) patients have abnormality in the reproductive tract; (2) patients have endometriosis or uterine adenomyosis; (3) both husband and wife have known chromosomal abnormality; (4) patients are unable to become pregnant due to male infertility.16 PCOS is often diagnosed with manifestations including oligomenorrhea or amenorrhea, hyperandrogenism or hyperandrogenemia and polycystic ovarian changes (in accordance with the criteria created by experts form the European Society for Human Reproduction and Embryology and the American Society for Reproductive Medicine on the Rotterdam meeting).17 The diagnosis of tubal factor infertility was confirmed through hysterosalpingography or laparoscopy.
IVF-ET therapeutic regimen and serum/follicular fluid collection
In the midluteal phase (patients with oligomenorrhea or irregular menstruation received artificial cycle treatment) of the last menstrual cycle before IVF-ET treatment, PCOS patients were treated with long-acting Gn-releasing hormone agonist and injected with imported leuprorelin acetate microspheres (1.35–1.875 mg) (Takeda Chemical Industries, Osaka, Japan). On the third day of the menstrual cycle, patients were examined to see if they met the pituitary downregulation standard (in the transvaginal ultrasound detection, the endometrium thickness is no more than 5 mm; the diameter of the largest follicle in the bilateral ovaries is <10 mm; the content of serum luteinizing hormone (LH) is no more than 5 IU l−1 and the estrogen (E2) content is <50 pg ml−1). If met the standard, patients were treated with daily intramuscular injection of Gn (75 U), imported FSH (75 U) (IBSA Institut Biochimique SA, Lugano, Switzerland) and FSH (75 U) (Li Min Pharmaceutical Factory of Livzon Pharmaceutical Group, Zhuhai, Guangdong Province, China). Patients underwent regular transvaginal ultrasonography and LH, E2 and progesterone levels were monitored to determine uterus and follicle development. The Gn dose was adjusted over time according to the number of follicles, level of serum E2, growth rate of follicles and ovarian response. If there was a dominant follicle with a diameter of 18 mm, two follicles with a diameter of 17 mm or the serum E2 level reached 200–300 pg ml−1 in a dominant follicle, patients were treated with intramuscular injection (5000–10 000 U) of human chorionic Gn (HCG) (Li Min Pharmaceutical Factory of Livzon Pharmaceutical Group). This injection occurred at 8 p.m. to 10 p.m. on the same day, and 36–38 h after the HCG injection, follicle puncture was performed under the guidance of a transvaginal ultrasonography for oocyte retrieval. After 3–4 h of culturing, the oocyte–cumulus–corona complex was moved to the in vitro fertilization culture liquid and an in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) was performed according to the sperm status. The fertilization status was assessed 16–20 h later. The oocytes were then transferred in oil-capped culture droplets and cultured in an incubator at 37 °C with 5% CO2 and 20% O2. The embryo development was observed on the second and third day. Three days after fertilization, two embryos that had high morphological scores were selected for transplantation and the other transplantable embryos were frozen and reserved. Progesterone (40 mg per day) was intramuscularly injected or orally taken in combination with progesterone tablets (Duphaston; Solvay Pharmaceuticals BV, Weesp, The Netherlands) at a dose of 20–40 mg per day for luteal phase support. This process lasted for 17 days from the day of oocyte retrieval. On the fourteenth day after embryo transfer, the HCG was detected for pregnancy determination. If a positive result was detected, luteal support was prolonged until clinical pregnancy was confirmed by transvaginal ultrasonography 2–3 weeks later when the gestational sac, yolk sac and primitive heart tube pulsation in the uterine cavity was observed. The E2 value, number of eggs, number of fertilized eggs, effective HCG embryos and occurrence rate of ovarian hyperstimulation syndrome (OHSS) was also recorded on that day. The criteria of OHSS were defined as reported previously.18 Intrauterine embryo transfer was performed 48–72 h after oocyte retrieval. Two embryos were conventionally transplanted and then the transplant cancellation rate, clinical pregnancy rate, abortion rate and child birth weight were recorded.
On the second or third day of menstruation and on the day of HCG injection, 4 ml of venous blood was obtained from all patients after fasting in the morning. The blood sample was kept at room temperature for 30 min and then centrifuged (2000 r.p.m. min−1) at room temperature for 10 min. The upper serum was transferred into a sterile EP tube, sealed with sealing film and then stored in a refrigerator at −80 °C for the later detection of hormone levels. The Gn treatment was stopped and HCG (r-HCG; Merck Serono, Geneva, Switzerland) was injected when one dominant follicle with a diameter of 18 mm or two follicles with a diameter of 17 mm or three follicles with a diameter of 16 mm appeared. When promoting ovulation, the amount of FSH and human menopausal Gn was adjusted in accordance with the follicular development.
Guided by the transvaginal ultrasonography, the follicular fluid (which contained follicles with a diameter ⩾15 mm) was collected via negative pressure suction. The first tube of follicle liquid without any blood or flushing liquid was immediately centrifuged (3000 r.p.m. min−1) at room temperature for 10 min. The supernatant was placed into a sterile tube, sealed with sealing film, labeled and stored in a refrigerator at −80 °C for further use.
Hormone determination in serum and follicular fluid
Before the experiment, all samples were thoroughly mixed at room temperature (about 25 °C) and assigned into the PCOS or control group. Electrochemical immunoassay (2010 Automation Instrument; Boehringer Mannheim GmbH, Mannheim, Germany) was performed to determine the E2, progesterone and LH levels in the serum. The variation within one group or between any two groups was <10%. The follicular fluid was diluted (1:100 or 1:10 000, respectively) according to the results of the preliminary experiments and FSH, prolactin and testosterone levels in the serum. Follicles were determined using the Enzyme-Linked Immunosorbent Kit (DRG Instruments, Marburg, Germany; DRG International, NJ, USA).
DNA extraction from whole blood
After informed consent was obtained, 4 ml of peripheral venous blood was drawn from all study subjects. It was then reserved in negative pressure non-anticoagulated blood tubes and labeled with the number and name of the patient. After 10 min of centrifugation at 3000 r.p.m. min−1, the whole blood DNA was extracted from the peripheral blood using a DNA Extraction Kit (Takara Bio, Shiga, Japan). Its concentration was detected using a DNA Concentration Detector (NANODROP2000) (Thermo Fisher Scientific, Waltham, MA, USA) and its purity was detected using OD260nm. The concentration was 100±20 ng μl−1 and A260nm/A280nm was between 1.6 and 1.8. The extracted DNA was stored at −20 °C.
Genotyping identification
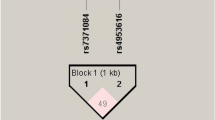
The primers were synthesized by Lejin Biotech (Nanjing, China).19 Detailed primer sequences19 are shown in Table 1. The Polymerase Chain Reaction (PCR) Kit was purchased from Shanghai Univ Biotechnology (Shanghai, China). The total reaction system was 20 μl, made up of 1 μl of extracted DNA, 1 μl of upstream and downstream primers (10 pmol ml−1), 10 μl of PCR mixture and 7 μl of deionized water. The reaction conditions were: predenaturation at 95 °C for 5 min, followed by a total of 40 cycles of denaturation at 95 °C for 30 s, annealing at 65 °C for 40 s and extension at 72 °C for 1 min; and a last extension at 72 °C for 10 min. The samples were added into an even mixture of 3% agarose gel (containing 0.5 μg ml−1 ethidium bromide), 4 μl of amplification products and 1 μl of bromophenol blue buffer. This was followed by electrophoresis (75 V) for 15 min in 0.5 × Tris-boric acid-ethylenediaminetetraacetic acid buffer. Subsequently, the amplified bands were observed under ultraviolet light. The PCR products of rs12644822C>T, rs3756159C>T and rs13138607C>T positions were digested using restriction enzyme Hgal (37 °C), SmlI (37 °C) and HpyCH4IV (37 °C) (purchased from Beijing Kingnor Agtech Corp., Beijing, China) in accordance with the product specifications. Next, electrophoresis was performed for 40 min in 120 V in 3.5% agarose gel and the amplified bands were once again observed under an ultraviolet light. Randomly selected samples (15%) were sent to Sangon Biotech (Shanghai, China) for bidirectional sequence detection to verify the results of the polymerase chain reaction-restriction fragment length polymorphism.
Statistical analysis
All data were analyzed using the SPSS 20.0 Software (SPSS, Chicago, IL, USA). Quantitative data were expressed as mean±s.d. Measurement data between two groups were validated using the t-test and data comparisons between three groups were detected by one-way analysis of variance. Categorical data were expressed as percentage and were compared using χ2. The genotype distribution and allele frequency of the control and PCOS groups were obtained by direct counting and verified using the Hardy–Weinberg Equilibrium. The Shesis Software (http://analysis.bio-x.cn/myAnalysis.php) was used to analyze haplotypes. Non-conditional logistic regression was used to analyze the risk factors and then the odds ratio and 95% confidence intervals were calculated. A P-value <0.05 is considered statistically significant.
Results
The PCOS group and the control groups are comparable
There was no significant difference in the age, duration of infertility and basal serum FSH, E2 and prolactin levels between the PCOS and control groups (P>0.05). Body mass index, basal serum LH, LH/FSH and testosterone levels and the number of basal follicle were all significantly lower in the control group than those in the PCOS group (all P<0.05) (Table 2).
The PCOS group has higher occurrence rate of OHSS and transplantation cancellation rate than the control group
There was no significant difference in the Gn dosage and stimulation time between the PCOS and control groups (P>0.05). The PCOS group had a significantly higher serum progesterone level before HCG injection, a greater amount of retrieved oocytes and embryos and a lower fertilization rate than the control group (all P<0.05). There was no significant difference in pregnancy or abortion rate between the two groups (both P>0.05). The PCOS group had a significantly higher occurrence rate of OHSS and transplantation cancellation rate than the control group (both P<0.05) (Table 3).
CC+CT genotypes and C alleles from rs12644822C>T, rs3756159C>T and rs13138607C>T enhanced the risk of PCOS
The frequency distribution of rs12644822C>T, rs3756159C>T and rs13138607C>T genotypes in the GnRHR gene was consistent with the results of Hardy–Weinberg equilibrium test (P>0.05). This suggested that the genotype frequency of three positions in the sample was in equilibrium and was a good representation of the population. According to the correlation analysis, the CC+CT genotypes and their alleles in the rs12644822C>T, rs3756159C>T and rs13138607C>T showed a significantly increased risk of PCOS than the TT genotypes and their alleles. This suggested that there was a significant correlation between GnRHR polymorphisms and PCOS (all P<0.05). It also suggested that the C alleles of the three positions were risk factors for PCOS (Table 4).
CT+CC genotypes are associated with the clinicopathological characteristics of PCOS patients
There was no evident difference in average age, body mass index, duration of infertility and basal serum FSH, E2 and prolactin levels between the TT genotypes and (CC+CT) genotypes in rs12644822C>T, rs3756159C>T and rs13138607C>T (all P>0.05). However, the CC+CT genotypes displayed higher basal serum LH, LH/FSH and testosterone levels and a greater number of basal follicle than the TT genotypes (all P<0.05) (Table 5).
CCC, CCT and TCC are risk factors of PCOS, and TCT, TTC and TTT are protective factors of PCOS
The rs12644822C>T, rs3756159C>T and rs13138607C>T haplotypes in the GnRHR gene of both groups were analyzed using the Shesis Software (any haplotype with a frequency <0.03 was excluded). It was found that there were seven common haplotypes and among these haplotypes, there was a significant difference in the frequency distribution of CCC, CCT, TCC, TCT, TTC and TTT between the two groups (all P<0.05). Moreover, it was demonstrated that CCC, CCT and TCC were risk factors for PCOS and that TCT, TTC and TTT were protective factors for PCOS. There was no distinct difference in the frequency of CCT between the two groups (all P>0.05) (Table 6).
CT+CC genotypes are associated with lower pregnancy rate of patients after IVF-ET
Out of the 314 PCOS patients who underwent IVF-ET treatment, there were 115 confirmed to be successful pregnancy cases that were classified into a pregnancy group and 199 to be non-pregnancy cases that were classified into a non-pregnancy group (Table 7). We found that patients with CT+CC genotypes of the three positions had a lower pregnancy rate after IVF-ET treatment than patients with TT genotypes (P<0.05). The results indicated that GnRHR polymorphisms were associated with lower pregnancy rate of patients after IVF-ET.
CT+CC genotypes of rs12644822C>T, rs3756159C>T and rs13138607C>T are risk factors influencing the outcome of PCOS patients after IVF-ET
Using pregnancy outcome and the three positions genotypes as dependent variables, logistic regression analysis was performed to further study the relationship between GnRHR polymorphisms and outcome of PCOS patients after IVF-ET treatment (Table 8). It was found out that rs12644822C>T, rs3756159C>T and rs13138607C>T from the CT+CC genotypes were risk factors influencing the outcome of PCOS patients undergoing IVF-ET.
Discussion
In the present study, we found that the CT+CC genotypes of rs12644822C>T, rs3756159C>T, rs13138607C>T increased the risk of PCOS and were risk factors influencing the outcome of PCOS patients undergoing IVF-ET.
Our study revealed that patients in the PCOS group had higher BMI, basal serum LH, LH/FSH and testosterone levels and a larger number of basal follicle than the control group. PCOS is regularly associated with obesity and being overweight.7 Obese women with PCOS are reported to have less retrieved oocytes, lower clinical pregnancy rates and higher miscarriage rates than non-obese patients with PCOS.20, 21 This result may be explained by the pathogenesis of PCOS as it is regarded as an endocrine disease that can naturally lead to obesity and a hyperstimulated status.22 Studies have shown that obesity can affect the size and quality of oocytes and embryos in PCOS women.23, 24 Huang et al.7 reported that this may be associated with insulin resistance, elevated leptin levels and the alteration of follicle androgen profiles. Increased circulating LH levels are a common biochemical feature of PCOS and a recent study revealed that LH mutation may influence the susceptibility to PCOS.25 Diurnal alternation of LH serum concentration is often high in women with PCOS. Previous data have demonstrated that insulin strengthens the amplitude of serum LH pulse opposed to its frequency in overweight women with PCOS.26 Although testosterone levels in the serum decrease as women with PCOS grow older, they still remain higher than those of the healthy individuals.27
Many factors can potentially affect the outcome IVF-ET treatment such as FSH, progesterone and E2.28 Our results demonstrated that the PCOS group had a higher progesterone level in the serum before HCG injection, more retrieved oocytes and embryos, higher occurrence rates of OHSS and transplantation cancellation, as well as a downregulated fertilization rate compared with the control group. Dai et al.29 reported that the progesterone levels on the day of HCG injection had no association with the clinical pregnancy rate, but the duration of progesterone elevation before HCG injection does have a negative association with the clinical pregnancy rate. According to Li and co-workers,30 an increased progesterone level on the day of HCG injection may affect the outcome of IVF-ET treatment. This hypothesis is based on evidence that patients with an increased progesterone level displayed lower clinical pregnancy and embryo implantation rates compared with patients whose progesterone level did not increase. Implantation is an important step for the successful application of assisted reproduction techniques.31 Three main factors have been reported to affect its effectiveness, namely, embryo quality, endometrial receptivity (ER) and a well-balanced embryo–endometrium interaction.32, 33 Under assisted reproduction techniques cycles, controlled ovarian hyperstimulation has an adverse effect on endometrial receptivity; however, this was mediated by the supraphysiologic levels of E2 and progesterone in the follicular phase. These altered hormone levels can lead to an asynchrony between the endometrium and transferred embryos, thus generating an endometrial environment that may result in implantation failure.34, 35
The most important finding in our study is that CC+CT genotypes of the rs12644822C>T, rs3756159C>T and rs13138607C>T in the GnRHR gene increase the risk of PCOS, and that these three positions are all risk factors that affect the outcome of PCOS patients undergoing IVF-ET. Polymorphisms of the GnRHR gene were detected using polymerase chain reaction-restriction fragment length polymorphism. Most mutations in the GnRHR gene were demonstrated to be responsible for multiple reproductive genetic disorders.36 A study conducted by Wu et al.,37 showed that ducks with the CT or CC genotypes had earlier egg laying ages and laid a greater number of eggs than ducks with the TT genotype of the GnRHR gene. This suggests that GnRHR polymorphisms have an important role in reproduction. Similar reproductive traits were also reported in humans and bovines with GnRHR polymorphisms.38, 39, 40 Based on a study on Holstein bulls, Yang et al.41 reported that GnRHR may serve as a potential marker for improvement in sperm quality, and that bulls with GA or CT genotypes should be selected for breeding. There is a speculation that polymorphism (C177T) existing in the regulatory regions of genes that exert an effect on the potential promoter and transcriptional start sites. This may affect the role of GnRHR in follicle growth and development.37 Moreover, a recent study suggested that GnRHR polymorphisms (rs12644822C>T, rs3756159C>T and rs13138607C>T) have a potential role in the pathogenesis of breast cancer.19 On the basis of such a speculation, we can naturally predict the potential role of these three polymorphisms in PCOS. Previously, researchers observed that one or two copies of the Ser allele are involved in the regulation of hyperandrogenism and carbohydrate metabolism by mildly decreasing testosterone and increasing insulin levels.42 Furthermore, positive links between reproduction outcomes and the GnRHR gene may indicate that IVF-ET is a good treatment option. However, the specific mechanism behind this process remains unclear. A previous study headed by Caburet et al.43 discovered that genetic changes in the hypothalamo-pituitary axis can affect PCOS occurrence. The relationship and relevant mechanism behind GnRHR and PCOS patient endocrine functioning was further evidenced in our study.
The haplotype analysis indicated that CCC, CCT, TCC haplotypes were risk factors for PCOS and that TCT, TTC and TTT were protective factors for PCOS. Haplotype analysis is valued as a reputable method in genetic studies of variant complicated diseases. This consensus may contribute to the finding of more efficient strategies in identifying genetic variants that can increase the risk of human diseases.44 In our study, results of haplotype analysis truly haplotype CCC (all variant) was not superior to other haplotypes with regard to odds ratio (PCOS susceptibility). It potentially can be explained that: (1) relatively small sample size; (2) SNPs of other PCOS-related genes are interacted. A genome-wide association study45 reported on PCOS patients found that multiple gene polymorphisms functionally interacted with each other. Further study is guaranteed to validate whether CCC haplotype is superior to other haplotypes with regard to odds ratio (PCOS susceptibility) in large sample size.
In summary, we found that the CC+CT genotypes of rs12644822C>T, rs3756159C>T and rs13138607C>T positions in the GnRHR gene increased the risk of PCOS and that polymorphisms of the three positions affected the outcome of IVF-ET treatment in PCOS patients. However, the underlying molecular mechanism needs to be further validated based on larger sample sizes.
References
Nandi, A., Chen, Z., Patel, R. & Poretsky, L. Polycystic ovary syndrome. Endocrinol. Metab. Clin. N. Am. 43, 123–147 (2014).
Wang, Y., Zhao, X., Zhao, H., Ding, H., Tan, J., Chen, J. et al. Risks for gestational diabetes mellitus and pregnancy-induced hypertension are increased in polycystic ovary syndrome. Biomed. Res. Int. 2013, 182582 (2013).
Sirmans, S. M. & Pate, K. A. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin. Epidemiol. 6, 1–13 (2013).
Barber, T. M. & Franks, S. Genetics of polycystic ovary syndrome. Front. Horm. Res. 40, 28–39 (2013).
Barber, T. M. & Franks, S. Adipocyte biology in polycystic ovary syndrome. Mol. Cell. Endocrinol. 373, 68–76 (2013).
Boomsma, C. M., Eijkemans, M. J., Hughes, E. G., Visser, G. H., Fauser, B. C. & Macklon, N. S. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum. Reprod. Update 12, 673–683 (2006).
Huang, K., Liao, X., Dong, X. & Zhang, H. Effect of overweight/obesity on IVF-ET outcomes in chinese patients with polycystic ovary syndrome. Int. J. Clin. Exp. Med. 7, 5872–5876 (2014).
Rosen, S. E., Henry, S., Bond, R., Pearte, C. & Mieres, J. H. Sex-specific disparities in risk factors for coronary heart disease. Curr. Atheroscler. Rep. 17, 49 (2015).
Luque-Ramirez, M., Mendieta-Azcona, C., Alvarez-Blasco, F. & Escobar-Morreale, H. F. Androgen excess is associated with the increased carotid intima-media thickness observed in young women with polycystic ovary syndrome. Hum. Reprod. 22, 3197–3203 (2007).
Naor, Z. Signaling by G-protein-coupled receptor (GPCR): studies on the GnRH receptor. Front. Neuroendocrinol. 30, 10–29 (2009).
Torrealday, S., Lalioti, M. D., Guzeloglu-Kayisli, O. & Seli, E. Characterization of the gonadotropin releasing hormone receptor (GnRHR) expression and activity in the female mouse ovary. Endocrinology 154, 3877–3887 (2013).
Cheung, L. W. & Wong, A. S. Gonadotropin-releasing hormone: GnRH receptor signaling in extrapituitary tissues. FEBS J. 275, 5479–5495 (2008).
Aguilar-Rojas, A. & Huerta-Reyes, M. Human gonadotropin-releasing hormone receptor-activated cellular functions and signaling pathways in extra-pituitary tissues and cancer cells (Review). Oncol. Rep. 22, 981–990 (2009).
Group ECW Genetic aspects of female reproduction. Hum. Reprod. Update 14, 293–307 (2008).
Goodman, N. F., Cobin, R. H., Futterweit, W., Glueck, J. S., Legro, R. S., Carmina, E. et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society Disease State Clinical Review: Guide to the Best Practices in the Evaluation and Treatment of Polycystic Ovary Syndrome—Part 1. Endocr. Pract. 21, 1291–1300 (2015).
Taylor, T. H., Wright, G., Jones-Colon, S., Mitchell-Leef, D., Kort, H. I. & Nagy, Z. P. Comparison of ICSI and conventional IVF in patients with increased oocyte immaturity. Reprod. Biomed. Online 17, 46–52 (2008).
Jakubowicz, D. J., Iuorno, M. J., Jakubowicz, S., Roberts, K. A. & Nestler, J. E. Effects of metformin on early pregnancy loss in the polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 87, 524–529 (2002).
Sohrabvand, F., Ansaripour, S., Bagheri, M. & Shariat, M. Cabergoline versus coasting in the prevention of ovarian hyperstimulation syndrome and assisted reproductive technologies outcome in high risk patients. Int. J. Fertil. Steril. 3, 35–40 (2009).
Lattrich, C., Muller, A. K., Schuler, S., Haring, J., Ruoff, A., Treeck, O. et al. Single nucleotide polymorphisms in the regulatory region of gonadotropin-releasing hormone receptor gene and breast cancer susceptibility. Oncol. Rep. 28, 1091–1095 (2012).
Jungheim, E. S., Lanzendorf, S. E., Odem, R. R., Moley, K. H., Chang, A. S. & Ratts, V. S. Morbid obesity is associated with lower clinical pregnancy rates after in vitro fertilization in women with polycystic ovary syndrome. Fertil. Steril. 92, 256–261 (2009).
Ozgun, M. T., Uludag, S., Oner, G., Batukan, C., Aygen, E. M. & Sahin, Y. The influence of obesity on ICSI outcomes in women with polycystic ovary syndrome. J. Obstet. Gynaecol. 31, 245–249 (2011).
Barber, T. M., McCarthy, M. I., Franks, S. & Wass, J. A. Metabolic syndrome in polycystic ovary syndrome. Endokrynol. Pol. 58, 34–41 (2007).
Marquard, K. L., Stephens, S. M., Jungheim, E. S., Ratts, V. S., Odem, R. R., Lanzendorf, S. et al. Polycystic ovary syndrome and maternal obesity affect oocyte size in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil. Steril. 95, 2146–2149, 2149 and 2141 e2141 (2011).
Shah, D. K., Missmer, S. A., Berry, K. F., Racowsky, C. & Ginsburg, E. S. Effect of obesity on oocyte and embryo quality in women undergoing in vitro fertilization. Obstet. Gynecol. 118, 63–70 (2011).
Liu, N., Ma, Y., Wang, S., Zhang, X., Zhang, Q., Zhang, X. et al. Association of the genetic variants of luteinizing hormone, luteinizing hormone receptor and polycystic ovary syndrome. Reprod. Biol. Endocrinol. 10, 36 (2012).
Nestler, J. E. & Jakubowicz, D. J. Decreases in ovarian cytochrome P450c17 alpha activity and serum free testosterone after reduction of insulin secretion in polycystic ovary syndrome. N. Engl. J. Med. 335, 617–623 (1996).
Winters, S. J., Talbott, E., Guzick, D. S., Zborowski, J. & McHugh, K. P. Serum testosterone levels decrease in middle age in women with the polycystic ovary syndrome. Fertil. Steril. 73, 724–729 (2000).
Lin, W. Q., Yao, L. N., Zhang, D. X., Zhang, W., Yang, X. J. & Yu, R. The predictive value of anti-Mullerian hormone on embryo quality, blastocyst development, and pregnancy rate following in vitro fertilization-embryo transfer (IVF-ET). J. Assist. Reprod. Genet. 30, 649–655 (2013).
Dai, W., Bu, Z. Q., Wang, L. L. & Sun, Y. P. The relationship between the changes in the level of progesterone and the outcome of in vitro fertilization-embryo transfer. Syst. Biol. Reprod. Med. 61, 388–397 (2015).
Shi, Y., Huang, J., Zhou, J., Liu, Y., Fu, X., Li, Y. et al. MicroRNA-204 inhibits proliferation, migration, invasion and epithelial–mesenchymal transition in osteosarcoma cells via targeting Sirtuin 1. Oncol. Rep. 34, 399–406 (2015).
Diaz-Gimeno, P., Horcajadas, J. A., Martinez-Conejero, J. A., Esteban, F. J., Alama, P., Pellicer, A. et al. A genomic diagnostic tool for human endometrial receptivity based on the transcriptomic signature. Fertil. Steril. 95, 50–60 and 60 e51–15 (2011).
Achache, H. & Revel, A. Endometrial receptivity markers, the journey to successful embryo implantation. Hum. Reprod. Update 12, 731–746 (2006).
Roque, M., Lattes, K., Serra, S., Sola, I., Geber, S., Carreras, R. et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil. Steril. 99, 156–162 (2013).
Shapiro, B. S., Daneshmand, S. T., Garner, F. C., Aguirre, M., Hudson, C. & Thomas, S. High ongoing pregnancy rates after deferred transfer through bipronuclear oocyte cryopreservation and post-thaw extended culture. Fertil. Steril. 92, 1594–1599 (2009).
Shapiro, B. S., Daneshmand, S. T., Garner, F. C., Aguirre, M. & Thomas, S. Large blastocyst diameter, early blastulation, and low preovulatory serum progesterone are dominant predictors of clinical pregnancy in fresh autologous cycles. Fertil. Steril. 90, 302–309 (2008).
Kerekoppa, R. Single nucleotide polymorphism identification and characterization of GnRHR gene in Bos taurus and Bos indicus cattle. Turk. J. Vet. Anim. Sci. 39, 10–15 (2015).
Wu, X., Yan, M. J., Wan, X. P., Lian, S. Y. & Li, A. Cloning and tissue expression profiling of the GnRHR gene of the Muscovy duck (Cairina moschata: polymorphism and association with egg-laying performance. Br. Poult. Sci. 56, 164–174 (2015).
Conn, P. M. & Ulloa-Aguirre, A. Trafficking of G-protein-coupled receptors to the plasma membrane: insights for pharmacoperone drugs. Trends Endocrinol. Metab. 21, 190–197 (2010).
Gianetti, E., Hall, J. E., Au, M. G., Kaiser, U. B., Quinton, R., Stewart, J. A. et al. When genetic load does not correlate with phenotypic spectrum: lessons from the GnRH receptor (GNRHR). J. Clin. Endocrinol. Metab. 97, E1798–E1807 (2012).
Liron, J. P., Prando, A., Ripoli, M. V., Rogberg-Munoz, A., Posik, D. M., Baldo, A. et al. Characterization and validation of bovine gonadotripin releasing hormone receptor (GNRHR) polymorphisms. Res. Vet. Sci. 91, 391–396 (2011).
Yang, W. C., Tang, K. Q., Yu, J. N., Zhang, C. Y., Zhang, X. X. & Yang, L. G. Effects of MboII and BspMI polymorphisms in the gonadotropin releasing hormone receptor (GnRHR) gene on sperm quality in Holstein bulls. Mol. Biol. Rep. 38, 3411–3415 (2011).
Valkenburg, O., Uitterlinden, A. G., Piersma, D., Hofman, A., Themmen, A. P., de Jong, F. H. et al. Genetic polymorphisms of GnRH and gonadotrophic hormone receptors affect the phenotype of polycystic ovary syndrome. Hum. Reprod. 24, 2014–2022 (2009).
Caburet, S., Fruchter, R. B., Legois, B., Fellous, M., Shalev, S. & Veitia, R. A. A homozygous mutation of GNRHR in a familial case diagnosed with polycystic ovary syndrome. Eur. J. Endocrinol. 176, K9–K14 (2017).
Zhao, H., Pfeiffer, R. & Gail, M. H. Haplotype analysis in population genetics and association studies. Pharmacogenomics 4, 171–178 (2003).
Chen, Z. J., Zhao, H., He, L., Shi, Y., Qin, Y., Shi, Y. et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat. Genet. 43, 55–59 (2011).
Acknowledgements
We would like to give our sincere appreciation to the reviewers for their helpful comments on this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, WY., Du, YQ., Guan, X. et al. Effect of GnRHR polymorphisms on in vitro fertilization and embryo transfer in patients with polycystic ovary syndrome. J Hum Genet 62, 1065–1071 (2017). https://doi.org/10.1038/jhg.2017.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2017.85
This article is cited by
-
The role of polymorphism in various potential genes on polycystic ovary syndrome susceptibility and pathogenesis
Journal of Ovarian Research (2021)