Abstract
Sturge–Weber syndrome (SWS) is a neurocutaneous disorder characterized by capillary malformation (port-wine stains), and choroidal and leptomeningeal vascular malformations. Previously, the recurrent somatic mutation c.548G>A (p.R183Q) in the G-α q gene (GNAQ) was identified as causative in SWS and non-syndromic port-wine stain patients using whole-genome sequencing. In this study, we investigated somatic mutations in GNAQ by next-generation sequencing. We first performed targeted amplicon sequencing of 15 blood–brain-paired samples in sporadic SWS and identified the recurrent somatic c.548G>A mutation in 80% of patients (12 of 15). The percentage of mutant alleles in brain tissues of these 12 patients ranged from 3.6 to 8.9%. We found no other somatic mutations in any of the seven GNAQ exons in the remaining three patients without c.548G>A. These findings suggest that the recurrent somatic GNAQ mutation c.548G>A is the major determinant genetic factor for SWS and imply that other mutated candidate gene(s) may exist in SWS.
Similar content being viewed by others
Main
Sturge–Weber syndrome (SWS; MIM no. 185300) is a rare neurocutaneous disorder characterized by facial cutaneous vascular malformations (port-wine stains), and ocular and cerebral vascular malformations result in neurological impairment including seizures and intellectual disability.1, 2 The prevalence is estimated at ~1/20 000–50 000.2 Because the occurrence of SWS is sporadic with no heritability, it is thought to be caused by somatic mutations.3 Previously, a somatic mutation in the gene encoding the q class of guanine nucleotide-binding protein (G-protein)-α subunit (guanine nucleotide-binding protein, Q polypeptide; GNAQ) was identified in both SWS patients and those with non-syndromic port-wine stains.4 Here, we investigated the presence of somatic GNAQ mutations in 15 SWS patients using targeted next-generation sequencing.
Patients and methods
Study population
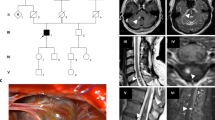
A total of 15 SWS patients were recruited for this study, and complete paired sets of peripheral blood leukocytes and surgically resected brain tissues were obtained from all patients. Patients were diagnosed as having SWS if they had two or more of the following symptoms: (1) craniofacial vascular malformation, (2) early-onset seizure, (3) contralateral hemiplegia or ateliosis, (4) intellectual disability and (5) ocular findings including choroidal vascular malformations, glaucoma, buphthalmia and hemianopia. All of the individuals underwent preoperative neuroimaging with magnetic resonance imaging. Detailed clinical features are shown in Table 1. All the brain specimens were histopathologically examined and confirmed as truly leptomengial angioma. Experimental protocols were approved by the Institutional Review Board of Yokohama City University School of Medicine and Juntendo University Graduate School of Medicine. Written informed consent was obtained from patients or parents of pediatric patients.
Deep sequencing of GNAQ c.548G>A
Genomic DNA of RNAlater (ThermoFisher Scientific, Waltham, MA, USA)-treated brain tissue blocks and peripheral blood leukocytes was extracted using Puregene Core Kit A (Qiagen, Valencia, CA, USA) and PAXgene Blood DNA kit (Qiagen), respectively, according to the manufacturer’s instruction. With genomic DNA obtained from leukocytes and tissues, the 173-bp target region including c.548G>A in GNAQ exon 4 was PCR-amplified using the following primers: forward 5′-ATTGTGTCTTCCCTCCTCTA-3′ and reverse 5′-GGTTTCATGGACTCAGTTAC-3′. A single-indexed sequencing library was prepared using the SureSelect XT Library Prep Kit (Agilent Technologies, Santa Clara, CA, USA) and sequenced on an Illumina HiSeq 2500 (Illumina, San Diego, CA, USA) with 101-bp paired-end reads. Image analysis and base calling were performed by sequence control software real-time analysis and CASAVA software v1.8.2 (Illumina). Quality-filtered reads were mapped to the human reference genome sequence (UCSC hg19, NCBI build 37) and aligned using Novoalign (Novocraft Technologies, Jaya, Malaysia). The aligned read files in the BAM format were sorted and indexed using SAMtools.5 Data analysis including allele counting was performed by Integrative Genomics Viewer software.6, 7 We defined the 1% cutoff line for the presence of mutant alleles out of total reads based on the Shirley’s criteria.4
GNAQ mutation screening
In the remaining subjects without c.548G>A, GNAQ mutation screening was performed using additional brain tissues. Primers were designed for the entire GNAQ (NM_002072.4) gene covering the coding region, intron–exon boundaries, as well as 5′- and 3′-untranslated regions (Table 2). A dual-indexed sequencing library was prepared with the Nextera DNA Sample Preparation Kit (Agilent Technologies) and sequenced on an Illumina MiSeq (Illumina) with 150-bp paired-end reads. Read alignment, sorting and indexing were performed as described above. Somatic single-nucleotide variant calling was performed by MuTect algorithms with the default setting.8 Variants that passed the MuTect filters were annotated using ANNOVAR software.9 Novel somatic single-nucleotide variants were selected based on the following four criteria: (1) mutant alleles observed with ⩾2 reads in the brain and <2 reads in blood leukocytes, (2) variants unregistered in dbSNP 137 except for clinically associated single-nucleotide polymorphisms (flagged),9 (3) variants unregistered in 6500 ESP, 1000 Genomes databases10, 11 or 575 in-house control exomes and (4) non-synonymous variants.
Results and Discussion
The recurrent somatic GNAQ c.548G>A mutation was identified in 12 of 15 SWS samples (80%) in the present study. The total read depth ranged from 20 284 × to 2 674 940 × (mean depth, 708 528 × ). Mutant allele frequencies ranged from 3.66 to 8.94% (mean, 5.59%; Table 1). In the remaining three subjects without c.548G>A (patients 3, 4 and 11; Table 1), we performed GNAQ mutation screening. The mean depth of coverage of the coding sequences ranged from 18 080 to 27 967 (average 23 050.6), and 500 or more reads covered 100% of coding sequences. However, no other somatic mutations were found in GNAQ.
Heterotrimeric G-proteins are composed of three subunits, α, β and γ, and act as signal transducers when coupled with seven transmembrane receptors in a diverse range of signaling pathways.12, 13 GNAQ encodes the q class of G-α subunit that activates phospholipase Cβ, thereby leading to the generation of inositol triphosphate and diacylglycerol.14, 15 Somatic mutations in GNAQ were previously reported as oncogenic gain-of-function mutations causing melanocytic neoplasms including melanomas and nevi.16, 17, 18
Van Raamsdonk et al.17 showed that somatic mutations in the Q209 and R183 residues of GNAQ, especially the Q209L substitution located in the Ras-like domain, were likely to be involved in tumorigenesis through upregulation of the MAP kinase pathway. R183 is located in the GTP-binding pocket of the G-α subunit and has an important role in GTP hydrolysis; however, the potential of the R183 mutant to activate signal transmission was markedly lower than that of the Q209 mutant.19, 20 Recently, Shirley et al.4 identified the somatic GNAQ mutation c.548G>A (pR183Q) in 88% of SWS patients (23 of 26) and 92% of patients with non-syndromic port-wine stains (12 of 13). This substitution was suggested to induce moderate activation of the extracellular signal-regulated kinase (ERK) pathway, which may lead to pathologic but not significantly neoplastic growth of capillaries in the skin and brain. In this study, we found the same recurrent somatic c.548G>A (pR183Q) mutation in 80% of patients (12 of 15), which supports the previous findings. However, we could not identify any other causative somatic mutation in GNAQ. Therefore it remains unclear whether mutations in other genes can be causative of SWS, although the recurrent somatic GNAQ mutation c.548G>A (p.R183Q) appears to be the major determinant in this disorder.
References
Sudarsanam, A . & Ardern-Holmes, S. L . Sturge-Weber syndrome: from the past to the present. Eur. J. Paediatr. Neurol. 18, 257–266 (2014).
Comi, A. M . Update on Sturge-Weber syndrome: diagnosis, treatment, quantitative measures, and controversies. Lymphat. Res. Biol. 5, 257–264 (2007).
Huq, A. H ., Chugani, D. C ., Hukku, B . & Serajee, F. J . Evidence of somatic mosaicism in Sturge-Weber syndrome. Neurology 59, 780–782 (2002).
Shirley, M. D ., Tang, H ., Gallione, C. J ., Baugher, J. D ., Frelin, L. P ., Cohen, B . et al. Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. New Engl. J. Med. 368, 1971–1979 (2013).
Li, H ., Handsaker, B ., Wysoker, A ., Fennell, T ., Ruan, J ., Homer, N . et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Robinson, J. T ., Thorvaldsdottir, H ., Winckler, W ., Guttman, M ., Lander, E. S ., Getz, G . et al. Integrative genomics viewer. Nat. Biotechnol. 29, 24–26 (2011).
Thorvaldsdottir, H ., Robinson, J. T . & Mesirov, J. P . Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 14, 178–192 (2013).
Cibulskis, K ., Lawrence, M. S ., Carter, S. L ., Sivachenko, A ., Jaffe, D ., Sougnez, C . et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
Wang, K ., Li, M . & Hakonarson, H . ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Genomes Project C. Genomes Project C., Abecasis, G. R . Genomes Project C., Altshuler, D . Genomes Project C., Auton, A . Genomes Project C., Brooks, L. D . Genomes Project C., Durbin, R. M . et al. A map of human genome variation from population-scale sequencing. Nature 467, 1061–1073 (2010).
Genomes Project C. Genomes Project C., Abecasis, G. R . Genomes Project C., Auton, A . Genomes Project C., Brooks, L. D . Genomes Project C., DePristo, M. A . Genomes Project C., Durbin, R. M . et al. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
Neves, S. R ., Ram, P. T . & Iyengar, R . G protein pathways. Science 296, 1636–1639 (2002).
McCudden, C. R ., Hains, M. D ., Kimple, R. J ., Siderovski, D. P . & Willard, F. S . G-protein signaling: back to the future. Cell Mol. Life Sci. 62, 551–577 (2005).
Dong, Q ., Shenker, A ., Way, J ., Haddad, B. R ., Lin, K ., Hughes, M. R . et al. Molecular cloning of human G alpha q cDNA and chromosomal localization of the G alpha q gene (GNAQ) and a processed pseudogene. Genomics 30, 470–475 (1995).
Mizuno, N . & Itoh, H . Functions and regulatory mechanisms of Gq-signaling pathways. Neurosignals 17, 42–54 (2009).
Van Raamsdonk, C. D ., Bezrookove, V ., Green, G ., Bauer, J ., Gaugler, L ., O'Brien, J. M . et al. Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature 457, 599–602 (2009).
Van Raamsdonk, C. D ., Griewank, K. G ., Crosby, M. B ., Garrido, M. C ., Vemula, S ., Wiesner, T . et al. Mutations in GNA11 in uveal melanoma. New Engl. J. Med. 363, 2191–2199 (2010).
Wu, D ., Katz, A ., Lee, C. H . & Simon, M. I . Activation of phospholipase C by alpha 1-adrenergic receptors is mediated by the alpha subunits of Gq family. J. Biol. Chem. 267, 25798–25802 (1992).
Orth, J. H ., Preuss, I ., Fester, I ., Schlosser, A ., Wilson, B. A . & Aktories, K . Pasteurella multocida toxin activation of heterotrimeric G proteins by deamidation. Proc. Natl Acad. Sci. USA 106, 7179–7184 (2009).
O'Hayre, M ., Vazquez-Prado, J ., Kufareva, I ., Stawiski, E. W ., Handel, T. M ., Seshagiri, S . et al. The emerging mutational landscape of G proteins and G-protein-coupled receptors in cancer. Nat. Rev. Cancer 13, 412–424 (2013).
Acknowledgements
We thank the patients for participating in this work. We also thank Nobuko Watanabe for technical assistance. This study was supported by the Ministry of Health, Labour and Welfare of Japan, a Grant-in-Aid for Scientific Research (A), (B) and (C) from the Japan Society for the Promotion of Science, the Takeda Science Foundation, the fund for Creation of Innovation Centers for Advanced Interdisciplinary Research Areas Program in the Project for Developing Innovation Systems, the Strategic Research Program for Brain Sciences and a Grant-in-Aid for Scientific Research on Innovative Areas (Transcription Cycle) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nakashima, M., Miyajima, M., Sugano, H. et al. The somatic GNAQ mutation c.548G>A (p.R183Q) is consistently found in Sturge–Weber syndrome. J Hum Genet 59, 691–693 (2014). https://doi.org/10.1038/jhg.2014.95
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.95
This article is cited by
-
MRC1 and LYVE1 expressing macrophages in vascular beds of GNAQ p.R183Q driven capillary malformations in Sturge Weber syndrome
Acta Neuropathologica Communications (2024)
-
Somatic mutation spectrum of a Chinese cohort of pediatrics with vascular malformations
Orphanet Journal of Rare Diseases (2023)
-
Clinical and genetic analyses of patients with lateralized overgrowth
BMC Medical Genomics (2022)
-
A novel somatic mutation in GNAQ in a capillary malformation provides insight into molecular pathogenesis
Angiogenesis (2022)
-
Molecular and genetic mechanisms in brain arteriovenous malformations: new insights and future perspectives
Neurosurgical Review (2022)