Abstract
Single-nucleotide polymorphisms (SNPs) in the TNFSF4, TNFAIP3 and FAM167A-BLK genes have been associated with several autoimmune diseases. Associations of TNFSF4 and FAM167A-BLK with primary Sjogren’s syndrome (pSS) have also been described in a Caucasian population. However, it remains unknown whether polymorphisms of TNFSF4, TNFAIP3 and FAM167A-BLK are associated with pSS in Han Chinese. This study aimed to determine whether SNPs in TNFSF4, TNFAIP3 or FAM167A-BLK genetically predispose a Chinese Han population to pSS. Ten SNPs in the TNFSF4 region (rs1234315, rs2205960, rs844648 and rs704840), the TNFAIP3 gene (rs5029939 and rs2230926) and the FAM167A-BLK region (rs7812879, rs2254546, rs2618479 and rs2248932) were genotyped in a cohort of 555 pSS patients and 597 healthy controls, by using the Sequenom MassArray system. Weak associations were observed when the SNPs in TNFSF4 (rs2205960, rs844648 and rs704840) and FAM167A-BLK (rs7812879, rs2254546 and rs2618479) were directly analyzed or analyzed under dominant model between pSS and controls (all P<0.05). However, when Bonferroni correction was applied to the multiple comparisons, all of the associations vanished, except for rs7812879 (Pa=0.045). The frequencies of alleles, genotypes and haplotypes of TNFAIP3 SNPs and rs2248932 of FAM167A-BLK were not significantly different between the pSS patients and controls. No epistatic interactions were found to exist between the SNPs examined. Unlike the SNPs in TNFAIP3 and TNFSF4, rs7812879 in FAM167A-BLK imparts susceptibility to pSS in a Han Chinese population. The differential genetic risk profiles from other autoimmune diseases may indicate differential molecular mechanisms underlying pSS pathogenesis in this group.
Similar content being viewed by others
Introduction
Primary Sjogren’s syndrome (pSS) is an autoimmune inflammatory condition that primarily affects middle-aged women. In China, incidence estimates range from 0.33 to 0.77%.1 pSS manifests as lymphocytic infiltration into the exocrine glands and is characterized by the production of the anti-SSA and anti-SSB antibodies. Although pSS is generally considered a multi-factorial complex disease, the etiology of pSS remains largely unknown. However, based on knowledge of autoimmune diseases, it is believed that pSS development may be a result of interactions between immunological, hormonal, environmental and/or genetic factors.2 Despite the prevalence of pSS being higher than any of the other autoimmune diseases, it remains one of the most understudied rheumatic disorders.3 No genome-wide association studies of pSS are present in the publicly available literature databases. Likewise, studies of pSS candidate genes are relatively limited.4 It is possible, however, to utilize the extensive knowledge of other autoimmune disorders that share pathogenic features with pSS to gain insight into the potential genetic complexity of pSS.
Several features of pSS are common to the well-studied systemic lupus erythematosus (SLE) autoimmune disease. Both diseases are characterized by female predominance, high titers of immunoglobulin (Ig) G, presence of rheumatoid factor, production of anti-SSA/SSB, activation of interferon pathways and lymphoid hyperplasia in target organs with large numbers of auto-reactive B cells producing antibodies locally.5, 6 Like many of the autoimmune diseases, including SLE and rheumatoid arthritis, pSS epidemiological studies have shown that first-degree relatives of pSS patients have a higher incidence of the disease than unrelated individuals.7 Furthermore, recent evidence strongly indicates that pSS is a polygenic disorder and likely shares common genetic determinants with related autoimmune diseases, such as SLE.4 For example, the autoimmune disease-associated polymorphisms of STAT4 and IRF5 were found to be correlated with pSS.8, 9
Two recent genome-wide association studies involving Chinese populations identified three single-nucleotide polymorphisms (SNPs) in the tumor necrosis factor ligand TNFSF4 (also known as OX40 ligand, OX40L and CD252) gene as risk factors of SLE; all three (rs1234315, rs2205960 and rs704840) lie upstream of the TNFSF4-coding region.10, 11 Intriguingly, Nordmark et al.12 found the rs1234315 SNP to be associated with pSS in a European population. The rs844648 SNP, which lies in the 5′ untranslated region (UTR) of the TNFSF4 gene, was associated with SLE in Hong Kong Chinese13 and with systemic sclerosis in European populations.14, 15 Other studies of SLE and rheumatoid arthritis patients in multiple populations have revealed associations of both diseases with a nonsynonymous coding SNP, rs2230926, in the tumor necrosis factor-alpha-induced protein 3 (TNFAIP3), which is believed to mediate expression or activity of the A20 anti-inflammatory protein.11, 16, 17, 18 Located in intron 2 of TNFAIP3, rs5029939 is correlated with SLE and some forms of systemic sclerosis.19, 20 The FAM167A-B lymphoid tyrosine kinase (BLK) gene region has also been associated with SLE,10, 11, 21 rheumatoid arthritis,22, 23 systemic sclerosis24, 25 and the anti-phospholipid syndrome.26 Moreover, four SNPs in FAM167A-BLK (rs7812879, rs2254546, rs2618479 and rs2248932) were confirmed as risk factors for SLE by genome-wide association studies, including Chinese populations.10, 11 Rs7812879 and rs2254546 are located in the intergenic region between the FAM167A-coding sequence and the BLK-coding sequence, whereas rs2618479 and rs2248932 lie in the intron region of BLK. The polymorphisms of FAM167A-BLK have also been confirmed as associated with pSS in a European population.12
Considering the genetic overlap in the autoimmune diseases and the associations of these genes with pSS in other populations, we hypothesized that some of the related polymorphisms of TNFSF4, TNFAIP3 and/or FAM167A-BLK may also contribute to genetic susceptibility to pSS in a Chinese Han population.
Materials and methods
Patients and controls
This study was designed as a case–control, and all subjects (pSS, n=555; control, n=597) were unrelated and self-reported as Han Chinese. The study was approved by the Ethics Committee of the Peking Union Medical College Hospital before recruitment of study participants, which occurred between October 2008 and December 2011. All cases fulfilled the American-European consensus group classification criteria for pSS;27 patients were denied study enrollment if other autoimmune diseases were present, suspected or previously diagnosed. As labial salivary gland biopsies are not routine in clinical practice, only patients testing positive for the antibodies (anti-SSA or anti-SSB, or both) by enzyme-linked immuno sorbent assay (ELISA) (Euroimmun AG, Lübeck, Germany) were enrolled. The healthy control subjects were recruited from healthy participants attending the same hospital for routine physical examination. Anti-SSA and anti-SSB screening confirmed that all healthy control group participants were negative for both antibodies. All study participants provided informed consent.
DNA extraction and genotyping
A 2-ml peripheral blood sample was collected from each study participant, and DNA was extracted from the harvested white blood cells (Bioteke, Beijing, China). The DNA of each participant was genotyped using Sequenom Technology (San Diego, CA, USA) of MassArray analysis with matrix-assisted laser desorption ionization–time-of-flight mass spectrometry. Primers for the multiplex PCR and for locus-specific extension were designed with the accompanying MassArray Assay Design 3.0 software (https://www.mysequenom.com). The multiplex PCR was performed in a 384 plate, and the amplicons were subsequently applied as template for the locus-specific extension reaction. The final products were desalted and spotted onto the 384-SpectroCHIP array (Sequenom Technology). Allele detection was carried out using matrix-assisted laser desorption ionization–time-of-flight mass spectrometry, and the resultant mass spectrograms and genotype data were analyzed by the accompanying MassArray Typer software.
Statistical analysis
The 10 SNPs were tested for Hardy–Weinberg equilibrium (HWE) in control populations using χ2-test. Any SNPs that deviated from HWE (P<0.05) were excluded from further analysis. Genotype and allele frequencies of cases and controls were evaluated with χ2-test using the PLINK v1.07 whole-genome data analysis toolset (http://pngu.mgh.harvard.edu/~purcell/plink/). The odds ratios of associations were calculated with 95% confidence intervals. Genotype frequencies were further analyzed by three genetic models: additive, dominant and recessive. Epistasis among the SNPs was assessed by logistic regression using PLINK v1.07. Haplotype analysis was carried out with Haploview software v4.2 (http://www.broadinstitute.org/haploview). Power analysis was performed using Quanto version 1.2 (http://hydra.usc.edu/GxE/). The Bonferroni correction was applied for multiple testing. P-values (corrected for multiple testing by Bonferroni correction) <0.05 were considered statistically significant.
Results
The characteristics of all the subjects are shown in Table 1. There were no significant differences between the pSS patients and controls with regard to the mean age or sex distribution. With the detected minor allele frequency of the participants in our study and the prevalence of pSS set at 0.33%, power calculations indicated that our sample size had >80% power (α=0.05) to detect associations with odds ratio ⩾1.4 for the SNPs in TNFSF4 and FAM167-BLK, and odds ratio ⩾1.6 for the SNPs in TNFAIP3 (Supplementary Table 1). The rs1234315 SNP in the TNFSF4 gene region deviated from HWE in the control group (P<0.05) and was excluded from subsequent analysis. The remaining nine SNPs from the three genes were in HWE and produced genotyping rates >93%. The accuracy was 100% as 50 samples were duplicate genotyped and the results were consistent.
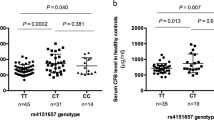
For the TNFSF4 region, only rs2205960 showed a suggestive association with pSS (P=0.026; Table 2) when genotype frequencies were analyzed. For the TNFAIP3 gene, neither of the two SNPs (rs5029939 and rs2230926) showed significant differences in allele or genotype frequencies between cases and controls (all, P>0.05; Table 2). For the FAM167A-BLK gene region, the genotype frequencies of rs7812879 and rs2254546 SNPs showed associations with pSS (P=0.005 and 0.010, respectively; Table 2). In addition, the rs2618479 SNP showed a trend for association with pSS (P=0.072; Table 2). No association with pSS was found for the fourth FAM167A-BLK SNP, rs2248932 (all, P>0.05). However, none of the observed associations for any of the SNPs, with the exception of FAM167A-BLK rs7812879 (Pa=0.045), retained statistical significance after Bonferroni correction.
All three of the SNPs (rs2205960, rs844648 and rs704840) in TNFSF4 showed differences in genotype frequency between cases and controls under the dominant model (all, P<0.05; Table 3). None of the three genetic models showed any significant differences for the SNPs of TNFAIP3 (all, P>0.05; Table 3). For SNPs (rs7812879, rs2254546 and rs2618479) in FAM167A-BLK, weak associations were also observed under the dominant model (all, P<0.05; Table 3). However, none of the P-values remains <0.05 after applying the Bonferroni correction.
Considering that most pSS patients are female, we removed all of the data for the male patients in the cases and controls and re-performed the analyses on the female patients only, but the results were similar (data not shown). Furthermore, the haplotype formed by the SNPs showed no statistically significant associations with pSS (all, P>0.05; Table 4). Finally, we investigated epistasis among the nine SNPs from TNFSF4, TNFAIP3 and FAM167A-BLK (Table 5) according to the recent evidence for potential functional interaction among disease-susceptibility genes.28, 29 However, no evidence of intermolecular epistatic interactions was found (all, P>0.05; Table 5).
Discussion
The current study represents the largest genetic association study performed in pSS to date and the first to test the association of TNFSF4, TNFAIP3 and FAM167A-BLK polymorphisms with pSS in a non-caucasian population. We chose to investigate the genetic contribution of TNFSF4, TNFAIP3 and FAM167A-BLK to pSS based upon the putative roles of each of these genes’ products in aberrant T-/B-cell activation in pSS and their confirmed association with autoimmune diseases. Although frequencies of the risk alleles reported in pSS or other autoimmune diseases also increased in the patients of pSS in our study,11, 12, 13, 14, 17, 18, 19, 20 no evidence of TNFSF4 or TNFAIP3 SNPs were found being closely associated with pSS, and only association with pSS for one of the SNPs of FAM167A-BLK.
The TNFSF4 gene-encoded cytokine is expressed on the surface of antigen-presenting cells. Binding of TNFSF4 to its cognate receptor TNFRSF4 (also known as OX40 and CD134) regulates cytokine production from various immune cells. In addition, the intracellular regions of TNFRSF4 associate with TNF receptor (TNFR)-associated factors that can complex with the inhibitor of nuclear factor-κB (NF-κB), thereby allowing activation of both canonical and non-canonical NF-κB signaling pathways.30 In our study, departure from HWE precluded our ability to perform pSS correlation analyses for the rs1234315 SNP of the TNFSF4 gene region. Given the strong association of TNFSF4 with pSS in a Caucasian population and with other autoimmune diseases, it is possible, if not likely, that TNFSF4 confers risk to pSS in our study population. Analyses of the other three TNFSF4 SNPs (rs2205960, rs844648 and rs704840) indicated a suggestive association with pSS for the genotype frequency of rs2205960, and marginal association for all three under the genetic dominant model. However, these associations did not meet the standard of multiple testing. Therefore, we consider that these three SNPs in TNFSF4, which are known to be associated with other autoimmune diseases, may not be related to the susceptibility for pSS in our population. We presume that differences in genetic background between pSS and other diseases, as well as the potential genetic heterogeneity among different populations, may account for these results.
The TNFAIP3 gene encodes a de-ubiquitination protein known as A20, which can negatively regulate NF-κB signaling in response to multiple stimuli and protect cells against tumor necrosis factor-induced programmed cell death.31 Studies have suggested that TNFAIP3 is a key negative regulator of tumor necrosis factor-induced NF-κB signaling pathways in autoimmune diseases. However, in the Han Chinese population of the current study, TNFAIP3 SNPs did not exhibit significant association with pSS. Although Musone et al.32 reported that rs2230926 was significantly associated with Sjogren’s syndrome, it should be noted that the patients in their study were affected by two or more individual autoimmune diseases. Thus, rs2230926 and rs5029939 may in fact be related to a range of autoimmune diseases but not to pSS in particular. Furthermore, fundamental differences may exist in the TNFAIP3-related genetic pathogeneses of pSS and other autoimmune diseases. It is also important to note that in the current study, the GG genotype frequencies of rs2230926 and rs5029939 were too small to perform analyses based on the dominant and recessive genetic models. Future studies using larger sample sizes should be carried out to confirm this result.
The function of the protein encoded by FAM167A (C8orf13) is unknown. BLK, however, is known to encode a non-receptor tyrosine kinase of the src family that has expression highly restricted to B cells.33 The BLK protein has roles in B-cell receptor signaling and B-cell development.34 B lymphocytes are key contributors to the pathogenesis of pSS, functioning as the major effectors of autoantibody production, hypergammaglobulinemia and mediating an increased risk for development of B-cell lymphomas.35, 36 In our study, the association with pSS was only found when the genotype frequencies of rs7812879, rs2254546 and rs2618479 were directly analyzed or were analyzed under the dominant model. Only the genotype frequency difference of rs7812879 remained significant after Bonferroni correction, which suggests that rs7812879 may indeed be a susceptibility factor of pSS. It should be noted that the SNPs we chose in our study were different from those in the study by Nordmark et al.12 The SNPs in our study are those with the strongest associations with SLE in the Chinese population. Because the SNPs in our study did not show strong associations with pSS, future studies should assess whether other SNPs in FAM167A-BLK are associated.
Despite the facts that both TNFSF4 and TNFAIP3 interact with the NF-κB signaling pathway and that a recent study has indicated that BLK has an interactive effect with TNFSF4 in Chinese SLE patients,28 no evidence was found of a potential interaction between the examined SNPs of these genes and pSS in this study. This finding may be due to the lack of association between pSS and TNFAIP3 and/or the weak associations between TNFSF4 and FAM167A-BLK and pSS. In addition to differences in the genetic background of diseases and the limited sample size, another possible explanation may account for our results, that is, the SNPs in this study do not represent the general pSS disease but specific phenotypes that we were underpowered to assess, as our previous study have revealed that some SLE SNPs were correlated with certain clinical subtypes of the disease.37
In summary, the strong correlations that have been observed between TNFSF4, TNFAIP3 and FAM167A-BLK and other autoimmune diseases do not exist or are very weak for pSS in the Han Chinese population of our study. Although our study is the largest genetic association study performed to date for pSS, it is still limited and more research is required to understand the associations of TNFSF4, TNFAIP3 and FAM167A-BLK with pSS.
References
Zhang, N. Z., Shi, C. S., Yao, Q. P., Pan, G. X., Wang, L. L., Wen, Z. X. et al. Prevalence of primary Sjogren’s syndrome in China. J. Rheumatol. 22, 659–661 (1995).
Voulgarelis, M. & Tzioufas, A. G. Pathogenetic mechanisms in the initiation and perpetuation of Sjogren’s syndrome. Nat. Rev. Rheumatol. 6, 529–537 (2010).
Gaubitz, M. Epidemiology of connective tissue disorders. Rheumatology (Oxford) 45 (Suppl 3), iii3–iii4 (2006).
Scofield, R. H. Genetics of systemic lupus erythematosus and Sjogren’s syndrome. Curr. Opin. Rheumatol. 21, 448–453 (2009).
Jonsson, R., Bolstad, A. I., Brokstad, K. A. & Brun, J. G. Sjogren’s syndrome—a plethora of clinical and immunological phenotypes with a complex genetic background. Ann. N Y Acad. Sci. 1108, 433–447 (2007).
Meyer, O. Interferons and autoimmune disorders. Joint Bone Spine 76, 464–473 (2009).
Anaya, J. M., Tobon, G. J., Vega, P. & Castiblanco, J. Autoimmune disease aggregation in families with primary Sjogren’s syndrome. J. Rheumatol. 33, 2227–2234 (2006).
Korman, B. D., Alba, M. I., Le, J. M., Alevizos, I., Smith, J. A., Nikolov, N. P. et al. Variant form of STAT4 is associated with primary Sjogren’s syndrome. Genes Immun. 9, 267–270 (2008).
Miceli-Richard, C., Comets, E., Loiseau, P., Puechal, X., Hachulla, E. & Mariette, X. Association of an IRF5 gene functional polymorphism with Sjogren’s syndrome. Arthritis Rheum. 56, 3989–3994 (2007).
Yang, W., Shen, N., Ye, D. Q., Liu, Q., Zhang, Y., Qian, X. X. et al. Genome-wide association study in Asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet. 6, e1000841 (2010).
Han, J. W., Zheng, H. F., Cui, Y., Sun, L. D., Ye, D. Q., Hu, Z. et al. Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat. Genet. 41, 1234–1237 (2009).
Nordmark, G., Kristjansdottir, G., Theander, E., Appel, S., Eriksson, P., Vasaitis, L. et al. Association of EBF1, FAM167A(C8orf13)-BLK and TNFSF4 gene variants with primary Sjogren’s syndrome. Genes Immun. 12, 100–109 (2011).
Chang, Y. K., Yang, W., Zhao, M., Mok, C. C., Chan, T. M., Wong, R. W. et al. Association of BANK1 and TNFSF4 with systemic lupus erythematosus in Hong Kong Chinese. Genes Immun. 10, 414–420 (2009).
Gourh, P., Arnett, F. C., Tan, F. K., Assassi, S., Divecha, D., Paz, G. et al. Association of TNFSF4 (OX40L) polymorphisms with susceptibility to systemic sclerosis. Ann. Rheum. Dis. 69, 550–555 (2010).
Bossini-Castillo, L., Broen, J. C., Simeon, C. P., Beretta, L., Vonk, M. C., Ortego-Centeno, N. et al. A replication study confirms the association of TNFSF4 (OX40L) polymorphisms with systemic sclerosis in a large European cohort. Ann. Rheum. Dis. 70, 638–641 (2011).
Lee, Y. H., Bae, S. C., Choi, S. J., Ji, J. D. & Song, G. G. Associations between TNFAIP3 gene polymorphisms and rheumatoid arthritis: a meta-analysis. Inflamm. Res. 61, 635–641 (2012).
Shimane, K., Kochi, Y., Horita, T., Ikari, K., Amano, H., Hirakata, M. et al. The association of a nonsynonymous single-nucleotide polymorphism in TNFAIP3 with systemic lupus erythematosus and rheumatoid arthritis in the Japanese population. Arthritis Rheum. 62, 574–579 (2010).
Musone, S. L., Taylor, K. E., Lu, T. T., Nititham, J., Ferreira, R. C., Ortmann, W. et al. Multiple polymorphisms in the TNFAIP3 region are independently associated with systemic lupus erythematosus. Nat. Genet. 40, 1062–1064 (2008).
Bates, J. S., Lessard, C. J., Leon, J. M., Nguyen, T., Battiest, L. J., Rodgers, J. et al. Meta-analysis and imputation identifies a 109 kb risk haplotype spanning TNFAIP3 associated with lupus nephritis and hematologic manifestations. Genes Immun. 10, 470–477 (2009).
Dieude, P., Guedj, M., Wipff, J., Ruiz, B., Riemekasten, G., Matucci-Cerinic, M. et al. Association of the TNFAIP3 rs5029939 variant with systemic sclerosis in the European Caucasian population. Ann. Rheum. Dis. 69, 1958–1964 (2010).
Hom, G., Graham, R. R., Modrek, B., Taylor, K. E., Ortmann, W., Garnier, S. et al. Association of systemic lupus erythematosus with C8orf13 CBLK and ITGAM CITGAX. N. Engl. J. Med. 358, 900–909 (2008).
Ito, I., Kawasaki, A., Ito, S., Kondo, Y., Sugihara, M., Horikoshi, M. et al. Replication of association between FAM167A(C8orf13)-BLK region and rheumatoid arthritis in a Japanese population. Ann. Rheum. Dis. 69, 936–937 (2010).
Orozco, G., Eyre, S., Hinks, A., Bowes, J., Morgan, A. W., Wilson, A. G. et al. Study of the common genetic background for rheumatoid arthritis and systemic lupus erythematosus. Ann. Rheum. Dis. 70, 463–468 (2011).
Ito, I., Kawaguchi, Y., Kawasaki, A., Hasegawa, M., Ohashi, J., Kawamoto, M. et al. Association of the FAM167A-BLK region with systemic sclerosis. Arthritis Rheum. 62, 890–895 (2010).
Gourh, P., Agarwal, S. K., Martin, E., Divecha, D., Rueda, B., Bunting, H. et al. Association of the C8orf13-BLK region with systemic sclerosis in North-American and European populations. J. Autoimmun. 34, 155–162 (2010).
Yin, H., Borghi, M. O., Delgado-Vega, A. M., Tincani, A., Meroni, P. L. & Alarcon-Riquelme, M. E. Association of STAT4 and BLK, but not BANK1 or IRF5, with primary antiphospholipid syndrome. Arthritis Rheum. 60, 2468–2471 (2009).
Vitali, C., Bombardieri, S., Jonsson, R., Moutsopoulos, H. M., Alexander, E. L., Carsons, S. E. et al. Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann. Rheum. Dis. 61, 554–558 (2002).
Zhou, X. J., Lu, X. L., Nath, S. K., Lv, J. C., Zhu, S. N., Yang, H. Z. et al. Gene-gene interaction of BLK, TNFSF4, TRAF1, TNFAIP3, REL in systemic lupus erythematosus. Arthritis Rheum. 64, 222–231 (2011).
Hughes, T., Adler, A., Kelly, J. A., Kaufman, K. M., Williams, A. H., Langefeld, C. D. et al. Evidence for gene-gene epistatic interactions among susceptibility loci for systemic lupus erythematosus. Arthritis Rheum. 64, 485–492 (2012).
Croft, M. The role of TNF superfamily members in T-cell function and diseases. Nat. Rev. Immunol. 9, 271–285 (2009).
Wertz, I. E., O’Rourke, K. M., Zhou, H., Eby, M., Aravind, L., Seshagiri, S. et al. De-ubiquitination and ubiquitin ligase domains of A20 downregulate NF-kappaB signalling. Nature 430, 694–699 (2004).
Musone, S. L., Taylor, K. E., Nititham, J., Chu, C., Poon, A., Liao, W. et al. Sequencing of TNFAIP3 and association of variants with multiple autoimmune diseases. Genes Immun. 12, 176–182 (2011).
Dymecki, S. M., Zwollo, P., Zeller, K., Kuhajda, F. P. & Desiderio, S. V. Structure and developmental regulation of the B-lymphoid tyrosine kinase gene blk. J. Biol. Chem. 267, 4815–4823 (1992).
Texido, G., Su, I. H., Mecklenbrauker, I., Saijo, K., Malek, S. N., Desiderio, S. et al. The B-cell-specific Src-family kinase Blk is dispensable for B-cell development and activation. Mol. Cell Biol. 20, 1227–1233 (2000).
Youinou, P., Devauchelle-Pensec, V. & Pers, J. O. Significance of B cells and B cell clonality in Sjogren’s syndrome. Arthritis Rheum. 62, 2605–2610 (2010).
Youinou, P., Saraux, A. & Pers, J. O. B-lymphocytes govern the pathogenesis of Sjogren’s syndrome. Curr. Pharm. Biotechnol. 13, 2071–2077 (2012).
Li, P., Cao, C., Luan, H., Li, C., Hu, C., Zhang, S. et al. Association of genetic variations in the STAT4 and IRF7/KIAA1542 regions with systemic lupus erythematosus in a Northern Han Chinese population. Hum. Immunol. 72, 249–255 (2011).
Acknowledgements
This work was supported by funding from the National Science Technology Pillar Program in the 11th Five-year Plan (Grants 2008BAI59B02 and 2008BAI59B03), Research Special Fund for Public Welfare Industry of Health (201202004) and the National Natural Science Foundation of China (Grants 30471617, 30640084, 30872331 and 81072486). We thank Chunwei Cao of the Beijing Institute of Genomics for his help and suggestions in genotyping and data analysis.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Sun, F., Li, P., Chen, H. et al. Association studies of TNFSF4, TNFAIP3 and FAM167A-BLK polymorphisms with primary Sjogren’s syndrome in Han Chinese. J Hum Genet 58, 475–479 (2013). https://doi.org/10.1038/jhg.2013.26
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2013.26
Keywords
This article is cited by
-
SNP variations in IL10, TNFα and TNFAIP3 genes in patients with dry eye syndrome and Sjogren’s syndrome
Journal of Inflammation (2019)
-
TNFAIP3 genetic polymorphisms reduce ankylosing spondylitis risk in Eastern Chinese Han population
Scientific Reports (2019)
-
Association of TNFSF4 Polymorphisms with Neuromyelitis Optica Spectrum Disorders in a Chinese Population
Journal of Molecular Neuroscience (2017)
-
8p22–23-rs2254546 as a Susceptibility Locus for Kawasaki Disease: a Case-control Study and a Meta-analysis
Scientific Reports (2014)