Abstract
Cytochrome-c oxidase (COX) deficiency is one of the common childhood mitochondrial disorders. Mutations in genes for the assembly factors SURF1 and SCO2 are prevalent in children with COX deficiency in the Slavonic population. Molecular diagnosis is difficult because of the number of genes involved in COX biogenesis and assembly. The aim of this study was to screen for mutations in 15 nuclear genes that encode the 10 structural subunits, their isoforms and two assembly factors of COX in 60 unrelated Czech children with COX deficiency. Nine novel variants were identified in exons and adjacent intronic regions of COX4I2, COX6A1, COX6A2, COX7A1, COX7A2 and COX10 using high-resolution melting (HRM) analysis. Online bioinformatics servers were used to predict the importance of the newly identified amino-acid substitutions. The newly characterized variants updated the contemporary spectrum of known genetic sequence variations that are present in the Czech population, which will be important for further targeted mutation screening in Czech COX-deficient children. HRM and predictive bioinformatics methodologies are advantageous because they are low-cost screening tools that complement large-scale genomic studies and reduce the required time and effort.
Similar content being viewed by others
Introduction
Cytochrome-c oxidase (COX) deficiency is a clinically heterogeneous group of disorders that range from isolated myopathy to severe multisystem disease that can develop at any age.1 This defect is either biochemically isolated or combined with disruption of other components of the respiratory chain and can arise from mutations located either in mitochondrial genes or in nuclear genes encoding the structural subunits or corresponding assembly factors of the enzyme complex. The incidence of COX deficiency has been estimated to be 1:35000 births in the Slavonic population. The majority of the detected mutations are located in the SCO2 and SURF1 genes,2 which may be accompanied with secondary impairment of the other respiratory chain complexes.3, 4, 5 In several cases of primary COX defects, the normal borderline activity values of the other respiratory complexes were documented in COX15, c2orf64, SCO2 and SURF1 and SCO1 patients.4, 6, 7, 8 To top it all, the secondary complex IV deficiency was observed in patients with primary complex I or complex III deficiency.9, 10
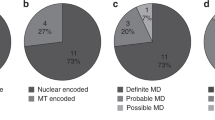
Despite of the advances in the identification of an increasing number of mutations and genes involved in the disease (SURF1, SCO1, SCO2, COX10, COX15, TACO1, LRPPRC, C2orf64, C20orf7, COX4I2 and COX6B1),7, 11, 12, 13, 14 the molecular basis of COX deficiency is unknown for many patients, which makes genetic counselling difficult. Over the last 20 years, we collected samples from a cohort of 106 Czech children with COX deficiency. In total, 51 of these patients have an isolated enzyme defect and 55 have a combined enzyme defect. COX deficiency was confirmed by biochemical and histochemical analyses. Sequencing of the SURF1, SCO2 and SCO1 genes was performed for all of the clinically relevant cases, and 25 patients were diagnosed with an isolated COX defect. By sequencing the mitochondrial DNA (mtDNA), the causative mutations were found in another seven patients with combined COX deficiency.15 Because only an extremely limited amount of DNA samples was available, subsequent genetic analysis was not performed for 14 patients. Therefore, a total of 60 unrelated children without a known genetic cause of COX deficiency were included in this study. In all, 17 of these patients were diagnosed with an isolated defect and 43 were diagnosed with a combined defect.
High-resolution melting (HRM) analysis is a simple, sensitive and cost-effective method that is based on the measurement of changes in the stability of homoduplexes and/or heteroduplexes in the presence of a fluorescent dye while the temperature of the amplified PCR products is increasing.16 Irrespective of the position of the base-pair variant within the PCR product, any type of homozygous or heterozygous sequence variant can be distinguished using this method.17, 18 The sensitivity and specificity of HRM analysis are better than many conventional methods used to detect mutations.19 Because of these unique properties, we used HRM to screen for mutations in genes assumed to be a cause of COX defects in our group of patients.
The aim of this work was to find or exclude the presence of pathological mutations in all the exons of the nuclear genes encoding the 10 structural subunits (COX4I1, COX4I2, COX5A, COX5B, COX6A1, COX6A2, COX6B1, COX6C, COX7A1, COX7A2, COX7B, COX7C and COX8A) and two assembly factors (COX10 and COX15) of COX using HRM analysis in a group of 60 unrelated Czech patients with biochemically confirmed COX deficiency. All new missense amino-acid substitutions identified in the exons of the studied genes were then analyzed using computational tools that can predict the effect of the mutation on protein function.
Materials and methods
Clinical information on the patients
Altogether, 60 unrelated children without a known genetic cause of COX deficiency were included in this study. Both patients with isolated COX deficiency and combined deficiency of COX with other respiratory chain complexes were involved in the study group.
The onset of mitochondriopathy was noticed at birth in 35 patients, during the first year of life in 14 patients, at the age of 1–5 years in six patients, at the age of 5–10 years in two patients and at the age of 10–15 years in three patients. The 60 patients included in this study presented with the following signs of mitochondrial disorders: failure to thrive (30/60), delay of psychomotor development (29/60), encephalopathy (28/60), hypotonia (26/60), visual impairment (25/60), myopathy (19/60), dysmorphia (15/60), cardiomyopathy (14/60), hepatomegaly (14/60), intrauterine growth retardation (12/60), spasticity (10/60), defects in motor skills (9/60), hearing impairment (9/60), epilepsy (7/60), dystrophy (7/60), microcephaly (7/60), nephropathy (6/60) and diabetes mellitus (2/60). Routine metabolic workup showed lactate acidosis (23/60), anemia (23/60) and hepatopathy (22/60). A total of 30 patients died prior to the beginning of this study; their survival ranged from 4 days to 13 years with a median of 1.1 years.
Patient consent
This study was approved by the Ethics Committee of the General University Hospital in Prague. All the samples were analyzed with the informed consent of the patients or their parents.
mtDNA analysis
Prior to the start of HRM mutation screening, mtDNA of all the 60 patients was sequenced. Briefly, whole-mtDNA molecule was amplified from muscle or fibroblast total DNA using PCR in 34 overlapping fragments. All the fragments were sequenced in both direction on ABI PRISM 3100/3100-Avant Genetic Analyser (Applied Biosystems, Carlsbad, CA, USA) and obtained sequences were compared with revised Cambridge Reference Sequence (rCRS) of the human mtDNA (NC_012920, http://www.mitomap.org/bin/view.pl/MITOMAP/HumanMitoSeq).
PCR design
As we did not know the exact occurrence and distribution of common single-nucleotide polymorphisms (SNPs) in the examined Czech population, the mutation screening was performed with probe-free HRM. This approach is especially suitable for large-scale genetic studies.20, 21, 22 Primers were designed, using the software Primer3Plus (http://www.bioinformatics.nl/cgi-bin/primer3plus/primer3plus.cgi), to amplify the coding regions of COX4I1, COX4I2, COX5A, COX5B, COX6A1, COX6A2, COX6B1, COX6C, COX7A1, COX7A2, COX7B, COX7C, COX8A, COX10 and COX15. Genomic DNA was amplified using PCR in the presence of LCGreen Plus Melting Dye (Idaho Technology Inc., Salt Lake City, UT, USA). Primer sequences and specific PCR conditions are listed in Supplementary Table 1. Genomic DNA was extracted from peripheral blood using the standard procedures with protease digestion, phenol-chloroform extraction and ethanol precipitation. For genetic and subsequent HRM analyses, a total of 15–50 ng of genomic DNA was amplified (NanoDrop ND-1000 UV-Vis Spectrophotometer, Nano-Drop Technologies Inc., Wilmington, DE, USA).
HRM analysis
The size of the scanned amplicons ranged from 191–565 bp. The HRM analysis was performed using a LightScanner instrument (Idaho Technology Inc.) according to the instructions in the LightScanner’s manual. A total of 70 amplicons covering 65 coding regions were analyzed. The melting profiles of 60 patient samples were analyzed blindly along with 14 reference control samples. Provided a new sequence variant was found by HRM analysis, all the remaining exons of the suspected gene were then sequenced (ABI PRISM 3100/3100-Avant Genetic Analyser, Applied Biosystems). Variants of both COX4I2 (rs6088855) and COX10 (c.1291C>T, rs113058506) were clearly distinguishable from the wild type when the DNA was mixed at a 1:1 ratio. The use of High Sensitivity Master Mix (Idaho Technology Inc.) allowed superior resolution of all genotypes for exon 5 of the COX10 gene and exon 9 of the COX15 gene. All the other common variants were readily identified by HRM during the first experiment.
In silico analysis
The web servers SIFT, SNAP, PolyPhen-2, MutPred, PMut and PANTHER were used to evaluate the possible pathogenicity of the identified missense substitutions as described elsewhere.23, 24, 25, 26, 27, 28
Molecular genetic analysis
The frequency of rare sequence variants in the Czech population was ascertained by PCR-restriction fragment length polymorphism and/or HRM analysis. RNA was isolated from human cell fibroblasts and transcribed to cDNA as described previously.29 cDNA and promoter analysis of the COX4I2, COX5A, COX7A1 and COX10 genes were performed in patients P8, P12, P17 and P29 (Expand Long Template PCR System, Roche Diagnostics GmbH, Mannheim, Germany). The nuclear DNA of these patients was analyzed using a Genome-Wide Human SNP 6.0 microarray chip (Affymetrix, Santa Clara, CA, USA).
Results
Mutation analysis of mtDNA in the investigated group of patients
In 59 of the patients, sequencing of the mtDNA revealed only known common polymorphisms listed in Mitomap (http://www.mitomap.org/MITOMAP) or mtDB—Human Mitochondrial Genome Database (http://www.mtdb.igp.uu.se/index.html). However, in patient P25, a homoplasmic variant, m.15866A>G (p.N374D), in MT-CYB gene was detected that has not been yet reported. It was found to be homoplasmic in a patient skeletal muscle, blood and cultivated fibroblasts and was not present among the 200 healthy controls, which was confirmed by BbsI-restriction fragment length polymorphism analysis. Because we lost the contact with the patient family, the presence of m.15866A>G (p.N374D) in MT-CYB gene could not be tested in maternal relatives. The protein alignment showed that the Asp374 of cytochrome-b is not evolutionary conserved. Because the western blot assembly profile and the activity of complex III performed on patient fibroblast were within the physiological range, we assumed that this base-pair exchange was a polymorphic variant. Considering the highly polymorphic nature of mitochondrial genome and the strict application of postulated pathogenicity criteria,30, 31 we assessed the m.15866G variant as polymorphic. These data suggested a nuclear genetic origin of the COX deficiency in the patient. However, subtle modification in the rate of complex III biogenesis might occur, as documented by others.32, 33 With the exception of the new homoplasmic m.15866G variant, the patient P25 carried only common SNPs in her mtDNA.
HRM analysis
Our findings expanded the known spectrum of mutations and SNPs in the COX genes. We documented nine new sequence variants; two were located in exons of COX7A1 (c.91_93delAAG, p.K31del) and COX6A2 (c.34T>G, p.L12V), whereas the remaining seven were located in introns of COX-related genes (Table 1). All the newly identified nucleotide sequence data are available in the EMBL database under the WEBIN ID accession numbers HE647854–HE647864. Furthermore, the HRM technique directly detected 52 known homozygous and/or heterozygous sequence variants located in COX-related genes (Supplementary Table 2). In all, 33 amplicons had a wild-type profile and did not have any heterozygous sequence variants. The 175 homozygous and/or heterozygous genetic variants, which when combined resulted in 152 distinct genotypes, were correctly detected.
In silico analysis
Seven sequence variants leading to missense amino-acid substitutions were identified in a total of eight patients (P4, P8, P12, P17, P25, P29, P33 and P39) located in four of the nuclear-encoded subunits, COX4I2, COX5A, COX6A2 and COX7A1, in an assembly factor COX10 (Figure 1, Table 2) and in mtDNA. In the 52 remaining patients, common SNPs were merely found (Supplementary Table 2). The onset of disease, symptoms and biochemical findings of four patients P8, P12, P17 and P29 harboring the four potentially pathogenic heterozygous mutations in nuclear DNA and of one patient P25 carrying the new homoplasmic variant in mtDNA are listed in Table 3.
Melting curve plots for the amplicons covering three exons of COX4I2, COX5A and COX7A1. Melting curves detected for exon 4 of COX4I2. The grey line depicts the wild type and the red line depicts the heterozygous variant c.253C>T (p.R85W) (a). Melting curves detected for exon 2 of COX5A. The grey line depicts the wild type, the red line depicts the heterozygous variant c.101–63G>A and the blue line depicts the heterozygous variant c.212G>A (p.R71H) (b). Melting curves detected for exon 2 of COX7A1. Seven distinct sequence genotypes were detected in these amplicons, which demonstrates the efficiency of the HRM assay. The orange line depicts rs68159832 (G), rs2285599 (G) and rs2285598 (G/C). The dark-blue line depicts rs68159832 (G), rs2285599 (G) and rs2285598 (G). The middle blue line depicts rs68159832 (G), rs2285599 (T/G) and rs2285598 (G/C). The light-blue line depicts heterozygous c.91_93delAAG (p.K31del), rs68159832 (G), rs2285599 (G) and rs2285598 (G). The grey line depicts rs68159832 (delG/G), rs2285599 (T) and rs2285598 (G). The rose line depicts rs68159832 (delG), rs2285599 (T), rs2285598 (G) and c.102+16 G>C. The red line depicts rs68159832 (delG), rs2285599 (T) and rs2285598 (G) (c).
The heterozygous variant of the COX4I2 gene that was identified in patient P8 was predicted to be pathological by SNAP, PolyPhen-2, MutPred and PMut. The SIFT software uses the protein alignment only, which may explain why p.R85W (COX4I2) was scored as tolerable, as opposed to the four other algorithms. Owing to the lack of data, PANTHER could not assign the status of this substitution.
Although SIFT determined the MT-CYB (p.N374D) and COX10 (p.R431W) substitutions to be non-tolerable, both predictions had low confidence scores. Additionally, the latter variant was classified as having low reliability by SNAP. The use of a different data library and algorithm may be the reasons for the neutrality of p.R431W (COX10) that was predicted by MutPred. Contradictorily, PolyPhen-2, which uses the two modus operandi algorithm, indicated that p.R431W (COX10) was probably damaging (HumDiv: score=0.986; sensitivity=0.72; specificity=0.96) and benign (HumVar: score=0.365; sensitivity=0.85; specificity=0.77), which implies that this variation might be pathogenic.
Two variations, p.L12V (COX6A2) and p.V366L (COX10), were each determined to be benign. Therefore, they are most likely to be neutral SNPs. Moreover, both variants occur at sites that are not evolutionary conserved. The pathogenicity classification of the MT-CYB missense substitution is ambiguous. Unfortunately, the prediction methodology, which would be able to infallibly evaluate missense variations located in highly polymorphic vital proteins, such as cytochrome-b, is not available at present. To the best of our knowledge, there are no predictive online servers that would be able to score proteins with deletions, such as the p.K31del (COX7A1).
Frequency of rare missense variants
Three heterozygous missense variations in COX4I2 (c.253C>T, p.Arg85Trp), COX5A (c.212 G>A, p.Arg71His) and COX7A1 (c.91_93delAAG, p.K31del) were found in both the group of 60 patients and a set of 100 healthy control samples, which was confirmed by PCR-restriction fragment length polymorphism analysis. This finding was further confirmed by PCR-restriction fragment length polymorphism analysis. Using HRM, the variant c.1291C>T (p.Arg431Trp, rs113058506) was found to be a heterozygous variant in two patients (2/60) and in two control samples (2/250). No homozygotes for c.1291T of COX10 were detected. Additionally, the protein alignment showed that the affected codons are evolutionary conserved. Even though all the remaining exons and adjacent intronic regions of the suspected genes were sequenced in P8 (COX4I2), P17 (COX5A), P29 (COX10) and P12 (COX7A1 and COX10), only common SNPs were identified. No mutations in the promoter regions and/or alternative cDNA splicing products were detected in COX4I2, COX5A, COX7A1 and COX10 of the patients P8, P12, P17 and P29. Besides, the deletions overlapping COX4I2, COX5A and COX7A1 genes were proved to be absent in all the four investigated patient genomic DNAs by microarray analysis.
Discussion
HRM analysis is capable of detecting homozygous and/or heterozygous sequence variations in amplified PCR products through monitoring differences in their thermal stability and evaluation of the shape and/or shift in their melting curves.34, 35 Although HRM analysis makes it possible to screen the entire amplicon region, sequencing is still needed to determine the precise sequence variation that is present in an amplicon. The accuracy of HRM analysis is dependent on the salt concentration, GC content, length and the primary sequence of the duplex. Additionally, it could be affected by the presence of many melting domains.36, 37, 38 However, several strategies can be used to achieve better resolution: genotyping using small amplicons, unlabelled probes, snapback primers, internal temperature calibrators and/or mixing patient samples with the reference control genotype.39, 40, 41, 42, 43, 44
We used internal calibrators and DNA mixing to improve the resolution of individual genotypes for four amplicons of the COX genes. However, the majority of examined amplicons did not require these adjustments. Our findings expanded the known spectrum of SNPs in COX genes. Using the optimized HRM methodology, we identified two new variants with altered codons, COX6A2 (p.L12V) and COX7A1 (p.K31del), that had not been previously described. Moreover, we discovered seven new non-coding variations in COX4I2, COX6A1, COX7A1, COX7A2 and COX10.
Because it is important to distinguish newly identified neutral variants from those that affect protein function, we applied online computational prediction tools to classify the variants. Nevertheless, proper interpretation of the results that were extracted from the web must take into account the differences in criteria and in the sequence and structural data that was used as the standard for the functional comparison of the analyzed mutant protein.45, 46, 47 The reliability of pathogenicity-prediction methods has been verified by several comparative studies to be approximately 81–92%.48, 49 Despite the mentioned drawbacks, the current predictive tools are an invaluable resource for genetic testing, especially because of their ability to determine when a rare sequence variant may be the cause of a Mendelian disorder. However, the application of only one predictive algorithm could be misleading.
Six rare heterozygous base-pair variations were found in five nuclear-encoded genes that affect codons of COX4I2 (p.R85W), COX5A (p.R71H), COX6A2 (p.L12V), COX7A1 (p.K31del) and COX10 (p.V366L, p.R431W) and were classified by predictive bioinformatics tools. To the best of our knowledge, this is the first time that these missense variants were detected in COX-deficient patients. With regard to the findings of the NHLBI-ESP (https://esp.gs.washington.edu/drupal) and the 1000 Genomes (http://www.1000genomes.org/home) research projects, the homozygous c.253T (COX4I2), c.212A (COX5A) and c.1291T (COX10) variants are extremely rare and could be pathogenic. Because the defects caused by mutations in nuclear-encoded COX-related genes are autosomal recessive, patients P8, P12, P17 and P29 should be considered heterozygous carriers of pathogenic mutations. Thus, it is evident that every human individual is a complex variable mosaic of potential pathogenic variants, which is in accordance with the results from exome sequencing and whole-genome microarray analyses.50, 51, 52 Nevertheless, an additional study of the four non-synonymous variations, p.R85W (COX4I2), p.R71H (COX5A), p.K31del (COX7A1) and p.R431W (COX10), should be performed to evaluate their pathogenicity, significance and severity. Cells with stable downregulated expression of individual subunits may be utilized.53
The clarification of complexity of COX defect is exceptionally challenging, especially because of the phenotype–genotype variability in COX-deficient patients. Because the existence of new uncharacterized assembly factors taking part in biogenesis of individual respiratory complexes are highly probable, a whole-exome sequencing is the optional approach to find the molecular bases of COX defect in our patients.54 As reported, high-throughput next-generation sequencing has enabled to sequence the whole DNA or RNA in a cost-efficient way, which may improve diagnosis and counselling in affected families.55 Hence, next-generation sequencing has opened discovery of disease-causing or disease-associated variants not available before but also new challenges, particularly in processing, analyzing and interpreting data.56
In conclusion, we designed and validated an HRM assay of 15 nuclear-encoded genes of COX that were possible causes of COX deficiency. We demonstrated that HRM and predictive methodologies are suitable low-cost screening tools. In accordance with the results obtained by the employed prediction tools, we documented nine new variants of COX-related genes, which updated the contemporary spectrum of known genetic sequence variations present in the Czech population. These variants will be important for future targeted mutation screening in Czech COX-deficient children.
Accession codes
References
Fernández-Vizarra, E., Tiranti, V., Zeviani, M. Assembly of the oxidative phosphorylation system in humans: What we have learned by studying its defects. Biochim. Biophys. Acta 1793, 200–211 (2009).
Böhm, M., Pronicka, E., Karczmarewicz, E., Pronicki, M., Piekutowska-Abramczuk, D., Sykut-Cegielska, J. et al Retrospective, multicentric study of 180 children with cytochrome c oxidase deficiency. Pediatr. Res. 59, 21–26 (2006).
Coenen, M. J. H., van den Heuvel, L. P., Nijtmans, L. G. J., Morava, E., Marquardt, I., Girschick, H. J. et al SURFEIT-1 gene analysis and two-dimensional blue native gel electrophoresis in cytochrome c oxidase deficiency. Biochem. Biophys. Res. Commun. 265, 339–344 (1999).
Sue, C., Karadimas, C., Checcarelli, N., Tanji, K., Papadopoulou, L., Pallotti, F. et al Differential features of patients with mutations in two COX assembly genes, SURF-1 and SCO2. Ann. Neurol. 47, 589–595 (2000).
Tarnopolsky, M. A., Bourgeois, J. M., Fu, M. H., Kataeva, G., Shah, J., Simon, D. K. et al Novel SCO2 mutation (G1521A) presenting as a spinal muscular atrophy type I phenotype. Am. J. Med. Genet. A 125A, 310–314 (2004).
Alfadhel, M., Lillquist, Y. P., Waters, P. J., Sinclair, G., Struys, E., McFadden, D. et al Infantile cardioencephalopathy due to a COX15 gene defect: Report and review. Am. J. Med. Genet. A 155, 840–844 (2011).
Huigsloot, M., Nijtmans, L. G., Szklarczyk, R., Baars, M. J., van den Brand, M. A., HendriksFranssen, M. G. et al A mutation in C2orf64 causes impaired cytochrome c oxidase assembly and mitochondrial cardiomyopathy. Am. J. Hum. Genet. 88, 488–493 (2011).
Valnot, I., Osmond, S., Gigarel, N., Mehaye, B., Amiel, J., Cormier-Daire, V. et al Mutations of the SCO1 gene in mitochondrial cytochrome c oxidase deficiency with Neonatal-onset hepatic failure and encephalopathy. Am. J. Hum. Genet. 67, 1104–1109 (2000).
Gerards, M., Sluiter, W., van den Bosch, B. J. C., de Wit, L. E. A., Calis, C. M. H., Frentzen, M. et al Defective complex I assembly due to C20orf7 mutations as a new cause of Leigh syndrome. J. Med. Genet. 47, 507–512 (2010).
Gil-Borlado, M. C., González-Hoyuela, M., Blázquez, A., García-Silva, M. T., Gabaldón, T., Manzanares, J. et al Pathogenic mutations in the 5′ untranslated region of BCS1L mRNA in mitochondrial complex III deficiency. Mitochondrion 9, 299–305 (2009).
Ugalde, C., Morán, M., Blázquez, A., Arenas, J., Martín, M. A. in Inherited Neuromuscular Diseases. (eds Espinós C., Felipo V., Francesc P.) 85–116 (Springer: New York, 2009).
Saada, A., Edvardson, S., Shaag, A., Chung, W., Segel, R., Miller, C. et al Combined OXPHOS complex I and IV defect, due to mutated complex I assembly factor C20orf7. J. Inherit. Metab. Dis. 35, 125–131 (2011).
Shteyer, E., Saada, A., Shaag, A., Al-Hijawi, F. A., Kidess, R., Revel-Vilk, S. et al Exocrine pancreatic insufficiency, dyserythropoeitic anemia, and calvarial hyperostosis are caused by a mutation in the COX4I2 gene. Am. J. Hum. Genet. 84, 412–417 (2009).
Massa, V., Fernandez-Vizarra, E., Alshahwan, S., Bakhsh, E., Goffrini, P., Ferrero, I. et al Severe infantile encephalomyopathy caused by a mutation in COX6B1, a nucleus-encoded subunit of cytochrome c oxidase. Am. J. Hum. Genet. 82, 1281–1289 (2008).
Vesela, K., Hansikova, H., Magner, M., Zeman, J. Cytochrome c oxidase deficiency in childhood. Paediatr. Croat 53 (Suppl 1), 122–126 (2009).
Reed, G. H., Kent, J. O., Wittwer, C. T. High-resolution DNA melting analysis for simple and efficient molecular diagnostics. Pharmacogenomics 8, 597–608 (2007).
Liew, M., Pryor, R., Palais,, R., Meadows,, C., Erali,, M., Lyon,, E. et al Genotyping of single-nucleotide polymorphisms by high-resolution melting of small amplicons. Clin. Chem. 50, 1156–1164 (2004).
Erali, M., Wittwer, C. T. High resolution melting analysis for gene scanning. Methods 50, 250–261 (2010).
Taylor, C. Mutation scanning using high-resolution melting. Biochem. Soc. Trans. 37, 433–437 (2009).
Millat, G., Chanavat, V., Julia, S., Crehalet, H., Bouvagnet, P., Rousson, R. Validation of high-resolution DNA melting analysis for mutation scanning of the LMNA gene. Clin. Biochem. 42, 892–898 (2009).
Millat, G., Chanavat, V., Créhalet, H., Rousson, R. Development of a high resolution melting method for the detection of genetic variations in hypertrophic cardiomyopathy. Clin. Chim. Acta 411, 1983–1991 (2010).
Dwyer, S., Carroll, L., Mantripragada, K. K., Owen, M. J., O′Donovan, M. C., Williams, N. M. Mutation screening of the DTNBP1 exonic sequence in 669 schizophrenics and 710 controls using high-resolution melting analysis. Am. J. Med. Genet. B Neuropsychiatr. Genet 153B, 766–774 (2010).
Ng, P. C., Henikoff, S. Predicting deleterious amino acid substitutions. Genome Res. 11, 863–874 (2001).
Bromberg, Y., Rost, B. SNAP: predict effect of non-synonymous polymorphisms on function. Nucleic Acids Res. 35, 3823–3835 (2007).
Adzhubei, I., Schmidt, S., Peshkin, L., Ramensky, V., Gerasimova, A., Bork, P. et al A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Li, B., Krishnan, V. G., Mort, M. E., Xin, F., Kamati, K. K., Cooper, D. N. et al Automated inference of molecular mechanisms of disease from amino acid substitutions. Bioinformatics 25, 2744–2750 (2009).
Ferrer-Costa, C., Gelpí, J. L., Zamakola, L., Parraga, I., de la Cruz, X., Orozco, M. PMUT: a web-based tool for the annotation of pathological mutations on proteins. Bioinformatics 21, 3176–3178.
Thomas, P. D., Campbell, M. J., Kejariwal, A., Mi, H., Karlak, B., Daverman, R. et al PANTHER: a library of protein families and subfamilies indexed by function. Genome Res. 13, 2129–2141 (2003).
Pejznochova, M., Tesarova, M., Hansikova, H., Magner, M., Honzik, T., Vinsova, K. et al Mitochondrial DNA content and expression of genes involved in mtDNA transcription, regulation and maintenance during human fetal development. Mitochondrion 10, 321–329 (2010).
DiMauro, S., Schon, E. A. Mitochondrial DNA mutations in human disease. Am. J. Med. Genet. 106, 18–26 (2001).
Mitchell, A. L., Elson, J. L., Howell, N., Taylor, R. W., Turnbull, D. M. Sequence variation in mitochondrial complex I genes: mutation or polymorphism? J. Med. Genet. 43, 175–179 (2006).
Tuppen, H. A. L., Blakely, E. L., Turnbull, D. M., Taylor, R. W. Mitochondrial DNA mutations and human disease. Biochim. Biophys. Acta 1797, 113–128 (2010).
Gil Borlado, M. C., Moreno Lastres, D., Gonzalez Hoyuela, M., Moran, M., Blazquez, A., Pello, R. et al Impact of the mitochondrial genetic background in complex III deficiency. PLoS One 5, e12801 (2010).
Gingeras, T. R., Higuchi, R., Kricka, L. J., Lo, Y. M. D., Wittwer, C. T. Fifty years of molecular (DNA/RNA) diagnostics. Clin. Chem. 51, 661–671 (2005).
Herrmann, M. G., Durtschi, J. D., Bromley, L. K., Wittwer, C. T., Voelkerding, K. V. Amplicon DNA melting analysis for mutation scanning and genotyping: cross-platform comparison of instruments and dyes. Clin. Chem. 52, 494–503 (2006).
Erali, M., Voelkerding, K. V., Wittwer, C. T. High resolution melting applications for clinical laboratory medicine. Exp. Mol. Pathol. 85, 50–58 (2008).
Garritano, S., Gemignani, F., Voegele, C., Nguyen-Dumont, T., Le Calvez-Kelm, F., De Silva, D. et al Determining the effectiveness of high resolution melting analysis for SNP genotyping and mutation scanning at the TP53 locus. BMC Genet. 10, 5 (2009).
Montgomery, J., Wittwer, C. T., Palais, R., Zhou, L. Simultaneous mutation scanning and genotyping by high-resolution DNA melting analysis. Nat. Protoc. 2, 59–66 (2007).
Wittwer, C. T., High-resolution, DNA melting analysis: advancements and limitations. Hum. Mutat. 30, 857–859 (2009).
Norambuena, P. A., Copeland, J. A., Křenková, P., Štambergová, A., Macek, M. Diagnostic method validation: high resolution melting (HRM) of small amplicons genotyping for the most common variants in the MTHFR gene. Clin. Biochem. 42, 1308–1316 (2009).
Liew, M., Seipp, M., Durtschi, J., Margraf, R. L., Dames, S., Erali, M. et al Closed-tube SNP genotyping without labeled probes. Am. J. Clin. Pathol. 127, 341–348 (2007).
Zhou, L., Errigo, R. J., Lu, H., Poritz, M. A., Seipp, M. T., Wittwer, C. T. Snapback primer genotyping with saturating DNA dye and melting analysis. Clin. Chem. 54, 1648–1656 (2008).
Gundry, C. N., Dobrowolski, S. F., Martin, Y. R., Robbins, T. C., Nay, L. M., Boyd, N. et al Base-pair neutral homozygotes can be discriminated by calibrated high-resolution melting of small amplicons. Nucleic Acids Res. 36, 3401–3408 (2008).
Margraf, R. L., Mao, R., Wittwer, C. T. Masking selected sequence variation by incorporating mismatches into melting analysis probes. Hum. Mutat. 27, 269–278 (2006).
Ng, P. C., Henikoff, S. Accounting for human polymorphisms predicted to affect protein function. Genome Res. 12, 436–446 (2002).
Kumar, S., Suleski, M. P., Markov, G. J., Lawrence, S., Marco, A., Filipski, A. J. Positional conservation and amino acids shape the correct diagnosis and population frequencies of benign and damaging personal amino acid mutations. Genome Res. 19, 1562–1569 (2009).
Ng, P. C., Henikoff, S. Predicting the effects of amino acid substitutions on protein function. Annu. Rev. Genomics Hum. Genet 7, 61–80 (2006).
Thusberg, J., Olatubosun, A., Vihinen, M. Performance of mutation pathogenicity prediction methods on missense variants. Hum. Mutat. 32, 358–368 (2011).
Hicks, S., Wheeler, D. A., Plon, S. E., Kimmel, M. Prediction of missense mutation functionality depends on both the algorithm and sequence alignment employed. Hum. Mutat. 32, 661–668 (2011).
Majewski, J., Schwartzentruber, J., Lalonde, E., Montpetit, A., Jabado, N. What can exome sequencing do for you? J. Med. Genet. 48, 580–589 (2011).
Sathirapongsasuti, J. F., Lee, H., Horst, B. A. J., Brunner, G., Cochran, A. J., Binder, S. et al Exome sequencing-based copy-number variation and loss of heterozygosity detection: ExomeCNV. Bioinformatics 27, 2648–2654 (2011).
He, Y., Hoskins, J. M., McLeod, H. L. Copy number variants in pharmacogenetic genes. Trends Mol. Med. 17, 244–251 (2011).
Fornuskova, D., Stiburek, L., Wenchich, L., Vinsova, K., Hansikova, H., Zeman, J. Novel insights into the assembly and function of human nuclear-encoded cytochrome c oxidase subunits 4, 5a, 6a, 7a and 7b. Biochem. J. 428, 363–374 (2010).
Calvo, S. E., Compton, A. G., Hershman, S. G., Lim, S. C., Lieber, D. S., Tucker, E. J. et al Molecular diagnosis of infantile mitochondrial disease with targeted next-generation sequencing. Sci. Transl. Med. 4, 118ra110 (2012).
Chen, J. M., Férec, C., Cooper, D. N. Revealing the human mutome. Clin. Genet. 78, 310–320 (2010).
de Magalhães, J. P., Finch, C. E., Janssens, G. Next-generation sequencing in aging research: Emerging applications, problems, pitfalls and possible solutions. Ageing Res. Rev. 9, 315–323 (2010).
Acknowledgements
We thank the patients and their families for participating in the study. This study was supported by the grants GAUK 28410 and SVV264502 from the Charles University in Prague, GAČR 305/08/H037 from the Grant Agency of the Czech Republic, IGA 10581/3 from the Internal Grant Agency of the Ministry of Health of the Czech Republic and by the research project P24/LF1/3 of the Charles University in Prague (program MOLMED).
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Vondrackova, A., Vesela, K., Hansikova, H. et al. High-resolution melting analysis of 15 genes in 60 patients with cytochrome-c oxidase deficiency. J Hum Genet 57, 442–448 (2012). https://doi.org/10.1038/jhg.2012.49
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2012.49
Keywords
This article is cited by
-
Multisystem mitochondrial diseases due to mutations in mtDNA-encoded subunits of complex I
BMC Pediatrics (2020)
-
Regulation of mitochondrial respiration and ATP synthesis via cytochrome c oxidase
Rendiconti Lincei. Scienze Fisiche e Naturali (2018)