Abstract
Mucolipidosis (ML) II alpha/beta and III alpha/beta are autosomal recessive diseases caused by a deficiency of α and/or β subunits of the enzyme N-acetylglucosamine-1-phosphotransferase, which is encoded by the GNPTAB gene. We analyzed the GNPTAB gene in 25 ML II and 15 ML III Japanese patients. In most ML II patients, the clinical conditions ‘stand alone’, ‘walk without support’ and ‘speak single words’ were impaired; however, the frequency of ‘heart murmur’, ‘inguinal hernia’ and ‘hepatomegaly and/or splenomegaly’ did not differ between ML II and III patients. We detected mutations in GNPTAB in 73 of 80 alleles. Fourteen new mutations were c.914_915insA, c.2089_2090insC, c.2427delC, c.2544delA, c.2693delA, c.3310delG, c.3388_3389insC+c.3392C>T, c.3428_3429insA, c.3741_3744delAGAA, p.R334L, p.F374L, p.H956Y, p.N1153S and duplication of exon 2. Previously reported mutations were p.Q104X, p.W894X, p.R1189X and c.2715+1G>A causing skipping of exon 13. Homozygotes or compound heterozygotes of nonsense and frameshift mutations contributed to the severe phenotype. p.F374L, p.N1153S and splicing mutations contributed to the attenuated phenotype, although coupled with nonsense mutation. These results show the effective molecular diagnosis of ML II and III and also provide phenotypic prediction. This is the first and comprehensive report of molecular analysis for ML patients of Japanese origin.
Similar content being viewed by others
Introduction
Mucolipidosis (ML) is clinically characterized by developmental delay and dysostosis multiplex, which is partially overlapped with mucopolysaccharidoses. ML II and III are autosomal recessive diseases caused by reduced enzyme activity of N-acetylglucosamine-1-phosphotransferase (GlcNAc-phosphotransferase) (EC 2.7.8.17). Targeting of newly synthesized lysosomal enzymes to lysosomes is mediated mainly by mannose-6-phosphate receptor, which recognizes the phosphate at the end of the sugar chain on lysosomal enzymes. The recognition marker is synthesized in a two-step reaction and GlcNAc-phosphotransferase acts in the first step. In patients, targeting of many lysosomal enzymes to the lysosome is impaired and levels of overflowed lysosomal enzymes are elevated in the serum and body fluids.1
Structural analysis of bovine GlcNAc-phosphotransferase shows that this enzyme is an α2β2γ2 hexameric peptide complex.2 In 2000, Raas-Rothschild et al.3 reported that the γ subunit is encoded by the GNPTG gene and contributes to the pathology of ML III gamma, formerly described as ML IIIC.4 Recent cloning of cDNAs for α/β subunits showed that it is encoded by a single gene GNPTAB.5 GNPTAB is located at chromosome 12q23.3, contains 21 exons and codes 1256 amino acids. The α–β boundary is located within exon 14, but the detailed mechanism of processing the precursor into α and β subunits is not clear.6 A series of genetic-complementation studies have shown heterogeneity in ML III and the genetic relationship between ML II and III.7, 8, 9 Mutations in GNPTAB cause both the severe type of ML (ML II alpha/beta, ML II, I-cell disease (MIM 252500)) and the attenuated type of ML (ML III alpha/beta, ML IIIA, Pseudo-Hurler polydystrophy (MIM 252600)).10, 11, 12 Mutations in GNPTG cause the attenuated type of ML (ML III gamma, ML IIIC, ML III variant (MIM 252605)).
We analyzed the GNPTAB gene in 40 Japanese ML II and III patients who had been diagnosed clinically or biochemically. Because the previously recorded clinical information was ambiguous, we reviewed the clinical records of these patients. In this article, we show the results of mutation analysis of the GNPTAB gene in 40 Japanese ML II alpha/beta and III alpha/beta patients and the comparison of the obtained genotype and phenotypes.
Materials and methods
Patients
The cases were Japanese ML II and III patients diagnosed after the 1970s to date. The diagnosis of ML was based on clinical manifestations and lysosomal enzyme activities in serum, lymphocyte and skin fibroblasts. The number of samples was 40, including 25 samples of ML II and 15 samples of ML III. In this study, all patients were probands and no siblings were included. New patients were informed about the gene test by counselors in each institute and consented. All methods in this study were approved by the ethics committee of Osaka University Graduate School of Medicine.
Clinical information
The clinical information of each patient followed in our outpatients’ clinic was reviewed from the medical records at our institute. To obtain clinical information about patients followed in other institutes, we sent questionnaires to outpatients’ doctors or patients’ families. Many medical records had been discarded because of the long period since their death or the end of follow-up. In some cases (cases 4, 12, 13, 14 and 34), only information, such as ‘ML II patient’ or ‘I-cell disease’, was available.
Cell culture
Skin fibroblasts of patients were stored in liquid nitrogen at −196 °C. Half of each thawed sample was subjected to re-culture with Dulbecco's modified Eagle's medium (GIBCO; Grand Island, NY, USA) with 10% fetal bovine serum and anti-biotic-anti-mycotic (GIBCO). The other half of each frozen sample was directly subjected to RNA and DNA extraction.
Total RNA and genomic DNA extraction
We extracted total RNA and genomic DNA using a standard extraction kit (Isogen; Nippongene, Tokyo, Japan) from patients’ peripheral blood leukocytes and/or cultured skin fibroblasts.
Reverse transcription
The obtained total RNA was subjected to reverse transcription to construct cDNA. Synthesis of cDNA was performed with M-MLV reverse transcriptase (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions.
Amplification of cDNA and genomic DNA
A cDNA fragment covering the whole coding region of GNPTAB was amplified by PCR in two fragments (first PCR) and each fragment was secondarily amplified in two fragments (second PCR). In other words, whole cDNA was amplified in four overlapping fragments. Six pairs of primer sequences for amplification of cDNA are listed in Supplementary 1. For genomic DNA amplification of each exon of GNPTAB by PCR, we used genomic primers described earlier by Kudo et al.10 (primer ID; 1088, 1076, 1077, 1078, 1082, 1118, 1119, 1085, 1086, 1089, 1107, 1092, 1109, 1120, 1121, 1122, 1123, 1163, 1164, 1129, 1134, 1135, 1136, 1215, 1216, 1139, 1140, 1141, 1142, 1219 and 1259) and other newly designed primers (Supplementary 1). For the amplification of each exon of GNPTG, we used primers described earlier by Raas-Rothschild et al.3 and other newly designed primers (Supplementary 1). PCR reactions were conducted in 20 μl reaction volumes with rTaq DNA polymerase (Takara Bio Inc., Otsu, Japan). The basic thermal profile consisted of initial denaturation at 94 °C for 2 min, followed by 35 cycles at 94 °C for 1 min, 56 °C for 2 min and 72 °C for 2 min, with a final extension at 72 °C for 7 min. Annealing temperature was modified within 55 and 60 °C. Three microliters of each PCR mixture were run on agarose gel to ensure that only the specific product was amplified.
DNA sequencing
PCR products were purified using a standard kit (SUPREC-02; Takara Bio Inc.) to remove unnecessary primers and finally dissolved in pure water at a concentration of approximately 2–10 ng μl−1 water as a sequencing reaction template. DNA sequencing was carried out with the same primers as mentioned above (Supplementary 1) using the BigDye Terminator V1.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA) and the Applied Biosystems 3100 genetic analyzer according to the manufacturer’s instructions. First, DNA sequencing was performed for cDNAs of GNPTAB followed by the confirmation by genomic DNA sequencing. We also analyzed the genomic DNA sequence of GNPTG in seven patients in whom only one mutation in GNPTAB was detected.
Screening for p.F374L and p.R1189X mutation by restriction fragment length polymorphism
DNA fragments containing the mutation site were amplified by PCR with primer 343/1109 (Supplementary 1) (Kudo et al.10) and 230/232 (Supplementary 1) and digested by restriction enzyme Mbo II or Taq I, respectively. PCR fragments containing p.F374L were recognized by Mbo II and digested from 367 to 33+16+97+221 bp. The same fragments derived from the normal allele were digested from 367 to 33+16+318 bp. With regard to PCR fragments containing p.R1189X, Taq I recognizes only the normal sequence and digests the fragment of 293 bp length into 205+88 bp fragments. If mutations were found by this method, DNA sequences were confirmed by genomic DNA sequencing by the same method as described above.
Results
Mutations in ML II alpha/beta and III alpha/beta patients
We detected 73 mutant alleles of 80 alleles in 40 Japanese patients (Table 1). Bold letters indicate new mutations detected in this study. These include 14 new mutations and four previously detected mutations. All four known mutations were reported by a Korean group11 and one, p.R1189X, was also reported by an Israeli group in a patient of Irish/Scottish origin.13 The most frequent mutation was the nonsense mutation p.R1189X (c.3565C>T) and its allele frequency was 33/80 (=41.25%) in the analyzed alleles of all ML II and III patients. In 90 healthy individuals, this mutation was not found by the restriction fragment length polymorphism method described above. p.F374L was found in 1 of 25 ML II patients and 7 of 15 ML III patients, and total allele frequency was 8/80 (=10.00%). Duplication of exon 2 was found in 1 of 25 ML II patients and 5 of 15 ML III patients, and total allele frequency was 6/80 (=7.50%). No mutation was found in GNPTG in seven patients in whom only one mutation was detected in GNPTAB.
Analysis of the duplication of exon 2
First, we found mutant alleles with the structure of duplicating exon 2 in cDNA analysis (Figure 1c). We constructed forward and reverse primers within exon 2 (primer 336/335) and performed long PCR with an XL PCR Kit (Applied Biosystems). The basic thermal profile consisted of initial denaturation at 94 °C for 1 min, followed by 35 cycles at 94 °C for 15 s, 62 °C for 12 min, with a final extension at 72 °C for 15 min. None was amplified with normal alleles by this method because each primer runs the other way. With a mutant allele, a specific fragment was amplified and the size of the fragment was estimated as approximately 15 kbp by agarose gel electrophoresis (Figure 1d). Sequencing analysis of this fragment was performed by primer walking and the junction between introns 1 and 2 was confirmed (Figure 1b); however, we could not detect any rearrangement between exons 1 and 2 by primer walking (data not shown).
Summary of the duplication exon 2. (a) Overview of rearranged mutant allele. (b) Genomic sequence around the junction. XL PCR product of primer set 336/335 was used as a sequence template. Sequencing analysis of mutant allele showed that IVS 2 jumped and connected to IVS 1 through 7 overlapping bases. The number above indicates the position in reference sequence NT_019546.15. (c) Sequence analysis of cDNA. Forward sequencing showed overlapped signal of exons 2 and 3 next to the end of exon 2. Reverse sequencing also showed overlapped signal of exons 1 and 2 next to the end of exon 2. (d) Agarose gel electrophoresis of PCR products amplified by primer set 336/335 and 365/367. These primers were designed to run the other way, respectively, and only the mutant allele was amplified. Left figure indicates that the amplified fragment by primer set 336/335 was estimated to be about 15 kbp. We then sequenced the fragment by primer walking. The junction was found and primers were designed near the junction. Right figure indicates the PCR fragment amplified by primer set 365/367. Estimated fragment size was 177 bp. M1 is a ladder of λ/Hind III marker and M2 is a ladder of 100 bp marker (Takara Bio Inc.).
Polymorphisms in GNPTAB
The 14 polymorphisms in GNPTAB found in this study are listed in Table 2. Ten polymorphisms were found within the intron and four within the coding region that does not change the amino-acid residue. Not all patients were tested because these polymorphisms were found incidentally in the process of sequencing analysis of mutations. Twelve polymorphisms have been registered in dbSNP (http://www.ncbi.nlm.nih.gov/SNP/). Two polymorphisms have not been reported previously.
Clinical phenotypes and genotypes
A summary of the clinical images and types of mutations of patients is shown in Table 3. We chose simple clinical manifestations, such as standing or walking, speaking, heart murmur, inguinal hernia and hepatosplenomegaly, which could be easily retrieved from old medical records or the memory of the doctors who followed them. Only the ML type was recorded in some cases but we could not obtain further information. The frequency of each clinical manifestation in the two groups is shown in Table 4.
In 33 patients, mutation was detected in both alleles. We arranged all cases into eight groups based on the type of mutation, respectively (Table 3).
Nonsense mutation contains p.Q104X, p.W894X and p.R1189X. Frameshift contains a type of mutation caused by the insertion or deletion of 1 or 4 bases, including c.914_915insA, c.2089_2090insC, c.2427delC, c.2544delA, c.2693delA, c.3310delG, c.3388_3389insC+c.3392C>T, c.3428_3429insA and c.3741_3744delAGAA. Each missense mutation, p.R334L, p.F374L, p.H956Y and p.N1153S, is enumerated individually. Duplication of exon 2 and skipping of exon 13 are also enumerated individually, although they finally cause frameshift. Homozygotes or compound heterozygotes of the mutation are indicated by a closed circle and heterozygotes by an open circle.
Discussion
In this study, several frequent mutations were detected. Nonsense mutation c.3565C>T (p.R1189X) was especially frequent in our study and its allele frequency was 41.25%. Eight of 25 ML II patients have this mutation homozygously. According to previous reports, this mutation was only found in two Korean cases11 and in one case of Irish/Scottish origin.13 This mutation seems to be common in eastern Asia, including Japan. It is speculated that it does not occur in a hot spot but by a founder effect, although experimental confirmation is difficult because of the unavailability of samples from the patients’ parents. The secondary frequent mutation is a missense mutation c.1120C>T (p.F374L) found in eight alleles compounded heterozygously with another mutation in this study. Duplication of exon 2 was found in six alleles and this mutation occurred at the genomic level of rearrangement. Sequencing analysis of the fragment from the tail of exon 2 to the head of exon 2 showed the junction between introns 1 and 2; however, there was no junction between exons 1 and 2 by primer walking. We suggest that this rearrangement is not derived from insertion of a region containing exon 2 but from the recombination between introns 1 and 2 (Figure 1a). Skipping of exon 13 is also frequent and is caused by the intronic one-base substitution c.2715+1G>A mutation. This mutation is discussed in detail in the previous article.11
We examined the founder effects of several mutations based on the result of polymorphisms. We show the genotype frequencies of several polymorphisms in patients with/without p.F374L and c.2715+1G>A (Table 5). Reference frequencies are data from HapMap-JPT (Japanese in Tokyo, Japan) in the International HapMap project. Our results indicate that six single-nucleotide polymorphism (SNPs) (rs10778150, rs2108694, rs6539012, rs10778148, rs759935 and rs376475) are coincident with mutation p.F374L and the SNP (rs3751249) with c.2715+1G>A in Japanese ML patients. We suggest that high correspondence between the two mutations and SNPs is most likely explained by a founder effect. With regard to the other mutations, there seemed to be no relationship between the mutations and polymorphisms.
Traditionally, ML patients have been classified into severe type (as type II) and attenuated type (as type III). We examined genotype–phenotype correlation with the obtained mutational information and patient diagnosis, namely ML type. Patients with a combination of homozygotes or compound heterozygotes within nonsense mutation, p.Q104X, p.W894X and p.R1189X, showed clinically severe phenotypes. Frameshift mutations caused by insertion or deletion of 1 or 4 bases (c.914_915insA, c.2089_2090insC, c.2427delC, c.2544delA, c.2693delA, c.3310delG, c.3388_3389insC+c.3392C>T, c.3428_3429insA, c.3741_3744delAGAA) also contribute to the severe phenotype.
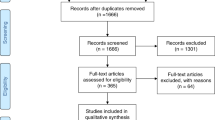
On the other hand, p.F374L is considered to contribute to relatively mild clinical manifestations, except for case 6, which was reported in detail by Kojima et al.14 and also by Okada et al.15 (case 9 in the article). He could stand alone but could not walk and was classified into ML II. We think that this was not a typical ML II case and showed a relatively attenuated phenotype. The other cases of p.F374L, if combined with nonsense or frameshift mutation, clinically showed ML III.
Duplication of exon 2 was found in attenuated cases, except for case 14; however, we cannot discuss case 14 further because limited information was available. We consider that duplication of exon 2 contributes to the attenuated phenotype. c.2715+1G>A causes skipping of exon 13.11 Case 26 has p.R1189X and c.2715+1G>A and shows an attenuated clinical phenotype. We consider that c.2715+1G>A also contributes to the attenuated phenotype.
Exon 2 contains 86 base sequences and exon 13 contains 1103 base sequences. The above two mutations consequently lead to frameshift. The Korean group reported skipping of exon 13 only in ML III patients. Kudo et al. reported a case in which splicing mutation caused an attenuated phenotype with highly suppressed enzyme activity and suggested that splicing was especially disrupted only in these fibroblasts. Our results are consistent, although the detailed mechanisms remain unclear.
Case 33 has compound heterozygosity of p.R1189X and p.N1153S. This case shows one of the most attenuated phenotypes in this study; she could speak and walk when she was 1 year old, without hepatosplenomegaly, and she is now 32 years old and working in a workshop. p.N1153S was found in only one allele; however, it is suggested that this mutation contributes to the attenuated phenotype.
In this study, clinical severity proved to be well correlated with mutational severity. Our result supports the previous report by Bargal et al.13 On the basis of information about known mutations, a patient’s clinical phenotype can be estimated. Even if new mutations are found, some clinical phenotypes can be predicted by the type of mutation.
We investigated the correlation between clinical manifestations and diagnosed ML types (Table 4). ‘Stand alone’, ‘walk without support’ and ‘speak single words’ are considered to well correlate to the ML type. In other words, a patient who cannot stand, walk or speak has a severe phenotype and life expectancy is estimated to be limited, generally called ‘ML II’. Clinical manifestations, such as ‘heart murmur’, ‘inguinal hernia’ and ‘hepatomegaly and/or splenomegaly’, were found in both ML II and III. Unfortunately, other various clinical manifestations, such as ‘age at onset’, ‘bone deformity’ and ‘neurological findings’, could not be examined because of poor information about many cases in this study. If a large-scale prospective investigation about the natural history of ML is carried out in the future, these problems may be solved.
Mucolipidosis II alpha/beta and III alpha/beta are caused by the same gene, GNPTAB, and the clinical phenotype shows a continuum from mild to severe. In both ML II and III, life expectancy is becoming longer owing to improved supportive therapy and care. Previously classified ML II patients can now live for more than 10 years; however, there are undoubtedly differences between typical ML II and III. It is difficult to predict the clinical phenotype from only enzymatic or biochemical characteristics.15 From a clinical standpoint, early prediction of prognosis is necessary. We could clearly classify the former ML types from selected clinical manifestations and these ML types correlated with genotypes. This is useful for predicting prognosis to analyze mutations for treatment, including hematopoietic stem cell transplantation, especially in attenuated cases diagnosed in the early stage by molecular analysis.16
According to the recent report,17 23 different mutations have been reported in the GNPTAB gene causing ML II and III alpha/beta. We detected 14 new mutations in the Japanese population. Three of four other already known mutations detected this time were reported only in Korean patient. This indicates that mutations found in Asian people are restricted to the Asian region and seem not to be derived from hot spots.
This is the first and comprehensive report of molecular analysis for Japanese patients of ML. Our data showed genotype–phenotype correlations in Japanese ML II and III (alpha/beta) in particular mutations. This result provides effective molecular diagnosis and phenotypic prediction of ML II and III (alpha/beta). Additionally, we showed that clinical severity and life expectancy are also predicted by particular clinical manifestations, including standing alone, walking without support and speaking single words.
References
Kornfeld, S. & Sly, W. S. I-cell disease and Pseudo-Hurler Polydystrophy: Disorders of lysosomal enzyme phosphorylation and localization. In The Metabolic and Molecular Bases of Inherited Disease (eds Scriver, C. R., Beaudet, A. L., Sly, W. S., Valle, D.) Ch. 138, 3469–3482 (McGraw-Hill, New York, 2001).
Bao, M., Booth, J. L., Elmendorf, B. J. & Canfield, W. M. Bovine UDP-N-acetylglucosamine:lysosomal-enzyme N-acetylglucosamine-1-phosphotransferase. I. Purification and subunit structure. J. Biol. Chem. 271, 31437–31445 (1996).
Raas-Rothschild, A., Cormier-Daire, V., Bao, M., Genin, E., Salomon, R., Brewer, K. et al. Molecular basis of variant pseudo-hurler polydystrophy (mucolipidosis IIIC). J. Clin. Invest. 105, 673–681 (2000).
Cathey, S. S., Kudo, M., Tiede, S., Raas-Rothschild, A., Braulke, T., Beck, M. et al. Molecular order in mucolipidosis II and III nomenclature. Am. J. Med. Genet. A 146A, 512–513 (2008).
Kudo, M., Bao, M., D’Souza, A., Ying, F., Pan, H., Roe, B. A. et al. The alpha- and beta-subunits of the human UDP-N-acetylglucosamine:lysosomal enzyme N-acetylglucosamine-1-phosphotransferase [corrected] are encoded by a single cDNA. J. Biol. Chem. 280, 36141–36149 (2005).
Kudo, M. & Canfield, W. M. Structural requirements for efficient processing and activation of recombinant human UDP-N-acetylglucosamine:lysosomal-enzyme-N-acetylglucosamine-1-phosphotransferase. J. Biol. Chem. 281, 11761–11768 (2006).
Honey, N. K., Mueller, O. T., Little, L. E., Miller, A. L. & Shows, T. B. Mucolipidosis III is genetically heterogeneous. Proc. Natl. Acad. Sci. USA 79, 7420–7424 (1982).
Mueller, O. T., Honey, N. K., Little, L. E., Miller, A. L. & Shows, T. B. Mucolipidosis II and III. The genetic relationships between two disorders of lysosomal enzyme biosynthesis. J. Clin. Invest. 72, 1016–1023 (1983).
Little, L. E., Mueller, O. T., Honey, N. K., Shows, T. B. & Miller, A. L. Heterogeneity of N-acetylglucosamine-1-phosphotransferase within mucolipidosis III. J. Biol. Chem. 261, 733–738 (1986).
Kudo, M., Brem, M. S. & Canfield, W. M. Mucolipidosis II (I-cell disease) and mucolipidosis IIIA (classical pseudo-hurler polydystrophy) are caused by mutations in the GlcNAc-phosphotransferase alpha/beta-subunits precursor gene. Am. J. Hum. Genet. 78, 451–463 (2006).
Paik, K. H., Song, S. M., Ki, C. S., Yu, H. W., Kim, J. S., Min, K. H. et al. Identification of mutations in the GNPTA (MGC4170) gene coding for GlcNAc-phosphotransferase alpha/beta subunits in Korean patients with mucolipidosis type II or type IIIA. Hum. Mutat. 26, 308–314 (2005).
Tiede, S., Storch, S., Lübke, T., Henrissat, B., Bargal, R., Raas-Rothschild, A. et al. Mucolipidosis II is caused by mutations in GNPTA encoding the alpha/beta GlcNAc-1-phosphotransferase. Nat. Med. 11, 1109–1112 (2005).
Bargal, R., Zeigler, M., Abu-Libdeh, B., Zuri, V., Mandel, H., Ben Neriah, Z. et al. When mucolipidosis III meets mucolipidosis II: GNPTA gene mutations in 24 patients. Mol. Genet. Metab. 88, 359–363 (2006).
Kojima, S., Okada, S., Kai, H., Ha, K., Nose, O., Ikeda, T. et al. A case of mucolipidosis II: biochemical, nutritional, and immunological studies. Brain. Dev. 1, 26–30 (1979).
Okada, S., Owada, M., Sakiyama, T., Yutaka, T. & Ogawa, M. I-cell disease: clinical studies of 21 Japanese cases. Clin. Genet. 28, 207–215 (1985).
Grewal, S., Shapiro, E., Braunlin, E., Charnas, L., Krivit, W., Orchard, P. et al. Continued neurocognitive development and prevention of cardiopulmonary complications after successful BMT for I-cell disease: a long-term follow-up report. Bone Marrow Transplant. 32, 957–960 (2003).
Plante, M., Claveau, S., Lepage, P., Lavoie, E. M., Brunet, S., Roquis, D. et al. Mucolipidosis II: a single causal mutation in the N-acetylglucosamine-1-phosphotransferase gene (GNPTAB) in a French Canadian founder population. Clin. Genet. 73, 236–244 (2008).
Acknowledgements
This study was supported in part by grants from the Research on Measures for Intractable Diseases, the Ministry of Health, Labour and Welfare in Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website (http://www.nature.com/jhg)
Supplementary information
Rights and permissions
About this article
Cite this article
Otomo, T., Muramatsu, T., Yorifuji, T. et al. Mucolipidosis II and III alpha/beta: mutation analysis of 40 Japanese patients showed genotype–phenotype correlation. J Hum Genet 54, 145–151 (2009). https://doi.org/10.1038/jhg.2009.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2009.3
Keywords
This article is cited by
-
GCAF(TMEM251) regulates lysosome biogenesis by activating the mannose-6-phosphate pathway
Nature Communications (2022)
-
Identification and characterization of 30 novel pathogenic variations in 69 unrelated Indian patients with Mucolipidosis Type II and Type III
Journal of Human Genetics (2020)
-
Identification of predominant GNPTAB gene mutations in Eastern Chinese patients with mucolipidosis II/III and a prenatal diagnosis of mucolipidosis II
Acta Pharmacologica Sinica (2019)
-
Mucolipidosis type III, a series of adult patients
Journal of Inherited Metabolic Disease (2018)
-
Clinical, biochemical and molecular characterization of Korean patients with mucolipidosis II/III and successful prenatal diagnosis
Orphanet Journal of Rare Diseases (2017)