Abstract
The aims of our research were to define the genotype–phenotype correlations of mutations in the phenylalanine hydroxylase (PAH) gene that cause phenylketonuria (PKU) among the Israeli population. The mutation spectrum of the PAH gene in PKU patients in Israel is described, along with a discussion on genotype–phenotype correlations. By using polymerase chain reaction/denaturing high-performance liquid chromatography (PCR/dHPLC) and DNA sequencing, we screened all exons of the PAH gene in 180 unrelated patients with four different PKU phenotypes [classic PKU, moderate PKU, mild PKU, and mild hyperphenylalaninemia (MHP)]. In 63.2% of patient genotypes, the metabolic phenotype could be predicted, though evidence is also found for both phenotypic inconsistencies among subjects with more than one type of mutation in the PAH gene. Data analysis revealed that about 25% of patients could participate in the future in (6R)-l-erythro-5, 6, 7, 8-tetrahydrobiopterin (BH4) treatment trials according to their mutation genotypes. This study enables us to construct a national database in Israel that will serve as a valuable tool for genetic counseling and a prognostic evaluation of future cases of PKU.
Similar content being viewed by others
Introduction
Hyperphenylalaninemia (HPA) is a group of diseases characterized by the persistent elevation of phenylalanine (Phe) levels in tissues and biological fluids. The most frequent form is phenylalanine hydroxylase (PAH; E.C. 1.14.16.1) deficiency, causing phenylketonuria (PKU; McKusick MIM 261600) or non-PKU HPA and corresponding to about 98% of all HPA cases. PAH deficiency is an autosomal recessive disorder affecting 1:10,000 individuals in Caucasian populations (Scriver et al. 1995; Dilella et al. 1986), but in some populations, the prevalence much higher (e.g., in the Catalonian population—about 1:6,600 and in about 1:5,000 live births in Ireland and western Scotland and among Yemenite Jews (Avigad et al. 1991). PKU results in mental retardation and other neurological complications that can be avoided by early treatment (Güttler and Lou 1990). It presents a broad phenotype spectrum ranging from classic PKU to moderate HPA depending on the residual enzymatic activity (Okano et al. 1991). Since the first mutation in the PAH gene was identified in a PKU patient (Dilella et al. 1986), almost 500 different mutations have been identified and listed in the PAH mutation database (PAHdb; http://www.mcgill.ca/pahdb) with various phenotypic consequences. Most of them are point mutations and microdeletions usually localized to the coding region or the intron–exon boundaries of the PAH gene. The mutations are evenly distributed along the PAH exons, although they are mainly found in its 3′ region.
Studies of PAH 3D structures (Erlandsen and Stevens 1999) reveal that the PAH enzyme is comprised of four monomeric proteins. Each monomer has three structural domains: an N-terminal regulatory domain (residues 1–142), a catalytic domain (residues 143–410), and a C-terminal tetramerization domain (residues 411–452). The studies have provided information on the active site and binding sites for its substrate and cofactor.
The number of different mutations in a given population is usually high, with a few prevalent mutations and a large number of private mutations (Avigad et al. 1991). Moreover, there are substantial differences in the mutational spectra between populations, making it difficult to establish a genotype–phenotype correlation. The associated phenotypes due to PAH deficiency range in severity from classic through mild PKU to mild hyperphenylalaninemia (MHP), as are defined by pretreatment blood phenylalanine levels (Song et al. 2005).
Several reports have been published that describe PAH gene mutations and analyses of genotype–phenotype correlations in European (Guldberg et al. 1993a, b; Zschocke and Hoffmann 1999; Kozak et al. 1997; Mallolas et al. 1999; O’Donnell et al. 2002; Guldberg et al. 1993a, b) and Chinese (Song et al. 2005) populations. From 1990 to 1993, there have been four publications on mutation screening in Israel: a report on a relative small number of different patients (27 patients with non-PKU HPA) that found that all of them were compound heterozygote (Avigad et al. 1990); one splice-site mutation in Palestinian Arabs (Kleiman et al. 1992); the S349P mutation found in Jews from Morocco and Tunisia (Weinstein et al. 1993); and a mutation limited to a common deletion mutation of exon-3 in Yemenite Jews (Avigad et al. 1990). Recently, a report describing the PAH gene mutation spectrum in the Israeli subpopulations was publish (Bercovich et al. 2008).
PAH is a nonheme iron-dependent enzyme that requires (6R)-l-erythro-5, 6, 7, 8-tetrahydrobiopterin (BH4) as an essential cofactor in the hydroxylation of l-Phe and also uses dioxygen as a substrate (Erlandsen et al. 2004). Certain PKU patients have been responsive to BH4 loading, resulting in a decreased l-Phe level. Several possibilities have previously been put forward to explain the BH4 response in mild PKU (Erlandsen et al. 2004): (a) decreased affinity of the mutant PAH for BH4; (b) stabilization of the active tetramer/dimer forms of the mutant proteins and protection from proteolytic cleavage, i.e., BH4 can act as a chemical chaperone, preventing misfolding and causing subsequent ubiquitin-dependent proteasomal degradation; (c) up-regulation of PAH gene expression; (d) BH4-induced change in BH4 biosynthesis; and (d) PAH mRNA stabilization, as shown for nitric oxide syntheses. In the international database (Blau 2003) is a list of genotypes that would respond well to BH4 treatment (BIOPKU; http://www.bh4.org/BH4DatabasesBiopku.asp), as indicated by the lowering of l-Phe levels in patients’ blood (Waters 2003). Most of the reported mutations in the PAH gene that were found to respond to BH4 treatment were in the catalytic region of the protein without direct connection to the binding of the cofactor (Blau and Erlandsen 2004). Therefore, identification of mutations responsive to BH4 treatment can help in the clinical diagnosis and/or the type of alternative treatment of PKU patients (Blau and Erlandsen 2004).
Mutation analysis of a given population is useful for further understanding the structural and functional aspects of the mutant protein and the correlation between genotype and phenotype. It is helpful in facilitating genetic consultation of patients’ families. In this paper, we present a comprehensive analysis of mutations and respective genotype–phenotype correlations in 360 independent PKU alleles from 180 patients representing the majority of the different ethnic groups in Israel (Jewish and Arabs).
Methods
Patients
DNA samples were collected in the Metabolic Disease Unit at Safra Children’s Hospital, Sheba Medical Center. This unit treats and provides follow-up for 450 patients coming from 200 different families with known ethnic origin. A total of 180 DNA samples (360 independent alleles) were obtained from unrelated patients with PKU.
The PKU phenotypes were determined according to the classification scheme proposed by Guldberg et al. (1998), which subdivides PAH deficiency into four categories: classic PKU, moderate PKU, mild PKU, and mild HPA (MHP). Classic PKU is caused by a complete or near-complete deficiency of PAH activity. Affected individuals typically show very high elevation of phenylalanine (>20 mg/dl) and tolerate less than 250–350 mg/day of dietary phenylalanine to keep plasma concentration of phenylalanine at a safe level of no more than 5 mg/dl. Without dietary treatment, most individuals develop profound, irreversible mental retardation. Individuals with moderate PKU have plasma phenylalanine concentrations of 10–20 mg/dl and tolerate 350–400 mg/day of dietary phenylalanine. Those with mild PKU have plasma phenylalanine concentrations 6.5–10 mg/dl and tolerate 400–600 mg/day of dietary phenylalanine. Infants with MHP have plasma phenylalanine concentrations of less than 6.5 mg/dl on a normal diet. Such individuals may not need dietary treatment and have normal cognitive neuropsychological development.
DNA purification and PCR amplification
Genomic DNA was extracted from ethylenediaminetetraacetic acid (EDTA)-preserved blood samples and isolated according to standard procedures (Bercovich and Beaudet 2003). The 13 exons and their exon-flanking intronic sequences of the PAH gene were amplified by polymerase chain reaction (PCR). The sequences of PCR primer were designed in accordance with the literature (Guldberg et al. 1998) and Table 1. PCR reactions were carried out in a volume of 50 μl with 10 mM Tris hydrochloride (HCl), pH 8.3, 1.5 mM magnesium chloride (MgCl2), 50 mM potassium chloride (KCl), 0.2 mM deoxynucleotide triphosphate (dNTP), and 30 nM primers. The PCR conditions were as described (Bercovich and Beaudet 2003): 94°C for 5 min, followed by 30 cycles with annealing temperatures for 1 min, and 72°C for 1 min; the reactions were ended with a final extension step at 72°C for 7 min.
Primers, annealing temperatures, and PCR product sizes for each of PAH exon will be provided by the authors upon request.
Mutations screening methods
Genetic diagnosis depends heavily on the availability of efficient and sensitive methods for detecting DNA mutations and sequence variations. With the expansion in our understanding of the human genome and the relevance of mutations to human disease, there is a compelling need for methods of mutation detection having high sensitivity and allowing for high throughput using partial or complete automation. The ideal method to use for mutation analysis, particularly if large numbers of DNA fragments to be analyzed, should be sensitive, nonhazardous, relatively inexpensive, and semi- or fully automated to minimize costs and labor utilization. dHPLC had been shown to meet these criteria for a growing number of applications in disease-related gene analyses (Bercovich and Beaudet 2003). Scanning for DNA mutations and variants using dHPLC involves subjecting PCR products to chromatography using an ion-pair reversed-phase cartridge. PCR products are denatured and allowed to reanneal. Under conditions of partial denaturation with a linear acetonitrile gradient, heteroduplexes from PCR samples having an internal sequence variation display a reduced column retention time relative to their homoduplex counterparts. The elution profile for heterozygous samples is typically quite distinct from that of either homozygous sequence, making the identification of heterozygous mutations relatively straightforward. An analysis for mutations on the X chromosome in males or for homozygous autosomal mutations requires mixing the test sample with the DNA of a known sequence.
Establishing dHPLC conditions
Mutation analysis was performed using the WAVE apparatus from Transgenomic Inc. (Omaha, NE, USA). The PCR products were denatured at 95°C for 5 min and cooled to 65°C down a temperature gradient of 1°C/min. Samples were kept at 4°C until 5 μl was applied to a preheated C18 reversed-phase column based on nonporous poly(styrene-divinylbenzene) particles (DNA-Sep Cartridge, Cat. no. 450181; all dHPLC catalog numbers are from Transgenomic Inc.). DNA was eluted within a linear acetonitrile gradient consisting of buffer A [0.1 M triethylammonium acetate (TEAA; Cat. no. SP5890)]/buffer B [0.1 M TEAA, 25% acetonitrile (Cat. no. 700001)]. The temperature at which heteroduplex detection occurred was deduced from the Transgenomic software (Wavemaker 4.2) and the Stanford dHPLC melting program (http://insertion.stanford.edu/meltdoc.html), which analyzes the melting profile of each specific DNA fragment. Fragments length and melting temperature (TM) for dHPLC analysis are presented in Table 1.
Homozygous mutations
To identify homozygous mutations, 10 μl PCR product of wild-type DNA and 10 μl PCR product of sample DNA were mixed 1.1 and denatured at 95°C. This enabled detection of homozygous mutations by formation of a heteroduplex (Shlush et al. 2002).
DNA sequencing
DNA sequencing was performed on the PCR products after dHPLC analysis, as previously described (Bercovich and Beaudet 2003). Fragments showing an abnormal dHPLC pattern were investigated for identification of sequence variants by automated sequence analysis on the ABI Prism 377 (Applera). This was performed according to the manufacturer’s protocol using a reamplified PCR product of the abnormal fragment (forward and reverse). The sequence variants were classified according to international databases (http://data.mch.mcgill.ca/pahdb_new/). The numbering of nucleotides follows GenBank accession number U49897.1 (http://www.pahdb.mcgill.ca/).
Genotype–phenotype analysis
In the analysis, nonsense, frameshift, and splice-site mutations are counted as null mutations, and four phenotypes are distinguished: classic PKU, moderate PKU, mild PKU, and MHP. For our analysis, genotypes were first divided into two categories: homoallelic mutant PAH genotype and heteroallelic mutant PAH genotype. Next, the heteroallelic PAH genotypes were further listed roughly in the order of increasing predicted residual activity (PRA), showing a transition from null + null through null + missense (functionally heterozygous) and finally to missense + missense (compound heterozygous).
Statistical analysis
Analyses were performed using the EpiInfo 2000 software (http://www.cdc.gov/epiinfo). The odds ratio (OR) and confidence interval (CI) were calculated as an estimation of risk among mutation carriers. Chi-square was used to determine the statistical significance of the different frequencies of genetic variations between patients and controls.
Results
Phenotype determination in the different ethnic groups of Israel
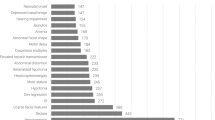
The aims of our research were to define the genotype–phenotype correlations of mutations in the PAH gene that causes PKU among the Israeli population. DNA samples were collected in the Metabolic Disease Unit at Safra Children’s Hospital, Sheba Medical Center. This unit treats and provides follow-up for 450 patients from 200 different families with known ethnic origin. All samples reported in this paper are PKU patients detected after neonatal screening. The patients were tested for the exclusion of lacking the cofactor BH4 for the differential characterization of the cause for the absent of PAH. Out of the 180 samples selected for mutations screening, seven patients did not follow through with this test, so it is not completely clear for these patients whether the cause for the diseases was a defective PAH gene. Patient DNA was screened for mutations in all 13 exons of the PAH gene. Screening was preformed using the dHPLC technique and sequencing DNA alterations for mutation characterization. Of the 180 patients, 114 were Jewish, 58 were Arabs, and eight were European. A total of 49 different mutations were found in our screening: 30 missense, 7 splice, two nonsense, eight deletion, two insertion mutations. Of these, three were only found in a homozygous state (Y198_E205fs, P225T and T117kfs).
PAH mutations spectrum
Mutations were detected in 148 of 154 alleles (96.1%) in classic PKU patients compared with only 55 of 72 alleles (76.4%) in MHP patients (Table 2).
Twenty-two PKU patients that had only one PAH heterozygous mutation were from all the four PKU phenotypes. But this was more frequent in MHP [nine of 36 patients (25%)] in comparison with classic PKU [four of 77 patients (5%)]. Among the 180 patients, the 49 mutations had different frequencies in the four PKU phenotypes (Table 2). In classic PKU patients, 58.4% were homozygous in comparison with only 11.1% in MHP patients. Mild PKU patients were 72.5% compound heterozygous in comparison with only 35.1% in classic PKU. Even though PKU mutations found in Israel are highly heterogeneous and the genotypes of most patients are compound heterozygote (52.2%), classic PKU makes up the predominant type in our sample (42%) in comparison with moderate PKU, mild PKU, and MHP (8.9%, 28.3%, and 20%, respectively, Table 2).
Genotype–phenotype correlation
In our work, nonsense, frame-shift ,and splice-site mutations are calculated as null mutations. Studying genotype–phenotype correlations in homoallelic mutant PAH genotypes and in null + null and null + missense (functionally heterozygous) genotypes has enabled us to discover the effect that single mutation exerts on phenotype (Kayaalp et al. 1997; Waters 2003). Seventeen different null mutations were found, which were 30% of patients’ alleles (125/360, Table 3). In our research, the genotypes were divided in to PAH homoallele (n = 21) and heteroallele (n = 86) (Table 3). The heteroallele genotype was divided in to null + null mutations (n = 3), null + missense mutations (n = 35) that account as functional-homozygote genotype, and missense + missense (n = 34), apparently compound heterozygous (Table 3). Fourteen genotypes did not mach any of these categories. Through this analysis, of the 49 different mutations that found in our project, in 34 we could identify the effect of the PKU phenotypes in cretin (69.4%). Seventeen of them were null mutations, and 17 were missense that, when they appear as homozygous or in combination with a null mutation, give a define phenotype.
Eleven mutations were found in at least two different phenotypes, and five mutations were found in at least three different PKU phenotypes (Tables 2, 3). In six mutations, there were no correlations to any of the PKU phenotypes. In some of the missense mutations, in the PAH gene, the PAH PRA in vitro (http://www.pahdb.mcgill.ca) is known. Mutations that cause severe (classic) phenotypes are those in which the PRA is less then 10% (Avigad et al. 1990). The R158Q mutation has a PRA of less then 10%, and so this mutation was found to be associated with the severe phenotype (Erlandsen and Stevens 1999). The PAH enzymatic activity with the R261Q, P281L, S349P and R408W missense mutations are known to be <1%, <1%, <1%, and 30%, respectively. These mutations had a null effect, as can be seen from the fact that when they were in combination with known null mutations, the patient phenotype was always the severe PKU. Two missense mutations (L197F and H271Q) of which there is no knowledge on the influence of PAH activity also showed severe phenotype when they in a homoallelic state (Table 3). In summary, missense mutation genotype–phenotype correlation revealed that eight mutations were associated with the severe phenotype (classic PKU): R252W, S349P, P281L, R158Q, R261Q, L197F, H271Q, and P225T (Tables 3, 4); eight mutations were clearly associated with the mild PKU phenotypes (MHP or mild PKU): V230I, A403V, D415N, A300S, A395G, I174V, I95F, and R261P, and one mutation was associated with the moderate phenotype: R241H. Distribution analysis for the types of missense mutations according to the functional domain in the PAH protein revealed that most were in the catalytic domain, one mutation was found in the tetramerization domain, and none were in the regulatory domain (Table 4). Null mutations were found in all the three domains.
Eight common polymorphic DNA alterations (SNPs) at different frequencies were detected in patients from all ethnic groups and controls group: 5UTR −71 A/C, E56E, IVS2 +19 T/C, Q232Q, V245V, IVS9 +43 G/T, L385L, and IVS12 −35 C/T. Two of the SNPs were found at high frequencies in both Jewish and Arab patients: Q232Q and L385L (66.1% and 81.4%, respectively). The E56E SNP was only found in Arab patients’ DNA (13.8%).
Genotypes respond to BH4 treatment
In the study we found two known mutations that will response well to BH4 treatment: A300S and IVS4 − 5C/G (allelic frequencies 5.8% and 0.8%, respectively) (Blau and Erlandsen 2004). Eight more mutations that cause minor downregulation of enzymatic activities and therefore are potential to BH4 treatment were found: L48S, A104D, R158Q, V230I, R241H, R261Q, A403V, and D415N (allelic frequencies 7.8%, 0.3%, 0.6%, 2.5%, 8.9%, and 0.3%, respectively).
Discussion
Genotype–phenotype correlation
Although PKU mutations detected in Israel are highly heterogeneous and the genotypes of most patients are compound heterozygotes (52.2%), classic PKU comprised the predominant type found in our samples (42%) compared with moderate, mild, and MHP (8.9%, 28.3%, and 20%, respectively, Table 2). Studying the genotype–phenotype correlations in homoallelic mutant PAH genotypes and in null + null and null + missense (functionally heterozygous) genotypes enabled us to discover the effect that a single mutation exerts on the phenotype (Kayaalp et al. 1997; Waters 2003).
By analyzing homozygous (null + null) and functional heterozygous (null + missense) mutations, the effect of 31 of 49 (63.3%) different mutations on the phenotypes could be determined (Table 3). Seventeen mutations were defined as null (nonsense, frame shift, and splice site), causing severe changes in the PAH protein and are associated with the PKU phenotype (more than 20 mg/dl of phenylalanine) (Waters 2003). When missense mutations are located in a functional codon, which has also been conserved during evolution, it can occasionally be defined as a null mutation. This is true of the well-known mutation R408W located in the region connecting the catalytic and tetramerization domains (Zschocke 2003). In some PAH gene missense mutations, the PRA in vitro (http://www.pahdb.mcgill.ca) is known.
Mutations that cause the severe phenotypes are those in which the PRA is less than 10% (Avigad et al. 1990). The R158Q mutation has a PRA of less then 10%, associating this mutation with the severe phenotype (Erlandsen and Stevens 1999). We found that these missense mutations (L197F, P225T, and H271Q) could be identified as null mutations, since they caused the severe phenotype (Table 3). Four mutations were associated with the mild PKU phenotype (I95F, I174V, R261P, and D415N, Table 3). These amino acids are probably located in a region that is not critical to PAH activity, and therefore, their substitution did not completely abolish PAH function. Most missense mutations were observed in the catalytic domain in which the functional site of PAH is located. One mutation was in the tetramerization domain, and two mutations were discovered in the regulatory region (Table 4). Null mutations were found in all three functional domains (Table 4). It seems that none of these domains plays a roll in the genotype–phenotype correlation. Two known missense mutations (R261Q and L48s), which have been previously reported not to show this correlation, did not demonstrate any such correlation in this study either. The R261Q has a PRA of 30% (Okano et al. 1991), which is probably not enough to completely abolish PAH activity. The amino acid derived from the L48S mutation, which does not show any damaging effect on the monomeric structure or on the specificity of PAH function, is located far from the active site of the protein (Guldberg et al. 1998; Erlandsen and Stevens 1999). This mutation was present in all phenotypes (Table 3). We found six patients who were homozygous to the L48S mutation. Two of them had a polymorphism in the PAH gene, which means that the entire gene is not deleted (one had the classic PKU and one with the moderate PKU). In the remaining four patients, polymorphisms were found in three different PKU phenotype categories. Therefore, this mutation has the most unpredictable phenotype outcome and should be investigated further.
In compound heterozygote patients, a wide matching range existed between a PAH mutant genotype and a PKU phenotype. When the compound heterozygotes are functional hemizygous (null + missense) genotypes, the less severe mutation of the two is the one that determines the phenotype (Guldberg et al. 1998). Thus, when one of the mutations has a severe effect and the second allows for at least a partially functioning PAH, the PKU metabolic phenotype will be less severe. For example, the IVS10 − 11G > A (null) + A403V (PRA = ∼100%) produces the mild PKU phenotype (Table 3). When the two mutations are in a compound heterozygous state and have the same predicted effect on the phenotype, the phenotype resulting from them will be less severe. For instance, when the R241H and A300S mutations are combined with a null mutation, they will confer a mild PKU phenotype, and when they are together, they will impart the MHP phenotype. When the two different mutations (of the two alleles) are null, the phenotype will tend to be severe. Mutations with a severe effect on PAH activity and which cause the classic PKU phenotype are usually in a homozygous state compared with mutations that cause the MHP phenotype (58.4% and 11.1%, respectively). This is probably true, since most MHP cases are results of compound heterozygotes in which one of the mutations is on one of the alleles and the mild mutation is on the second allele. The mild mutation is probably expressed only when it interacts with another severe mutation (Avigad et al. 1991; Kleiman et al. 1994). Furthermore, if one heterozygous mutation in the PAH gene does not cause the MHP phenotype to be expressed (Kleiman et al. 1994), probably another mutation exists that has not been detected in these patients in regions that have not yet been screened, e.g., the 5′UTR, 3′UTR, promoter, etc.
The main factor that probably influence the sensitivity to BH4 treatment is the allelic composition in the PAH locus. The level of response to treatment is dependent upon the type of mutant allele and its effect on enzymatic activity and enzyme wholeness (Blau and Erlandsen 2004). Therefore, in a situation in which the two mutations that cause low or absent PAH enzymatic activity are on different alleles, the outcome will mostly be the severe phenotype , and it is expected that these patients would not response well to BH4 treatment; in previous cases, it was found that some classic PKU did response to this treatment. On the other hand, patients with two mutations that show relatively high enzymatic activities (>30%) probably will have mild PKU or MHP phenotypes, and therefore are expected to response well to BH4 treatment (Erlandsen et al. 2004). Patients with a combination of a mild mutation and a severe mutation will mostly not response well to this type of treatment, but this response is dependent on the specific genotype (Blau and Erlandsen 2004). The biochemical phenotypes associated with R158Q and R261Q are mostly severe but are inconsistent (Table 4). This fact, combined with reports of response to tetrahydrobiopterin load in patients who carry these mutations (Leuzzi et al. 2006) deserves to be explored more. Response to BH4 is only limited to the mild mutation, which is still an interesting enigma. In our study, about 25% of patients could be candidates in the future for BH4 treatment trials according to their mutations genotypes.
Conclusion
The definition of the PKU mutational profile in Israel enables us to construct a national database covering detailed information on genotype–phenotype correlations. This database may serve as a valuable tool in genetic counseling and in prognostic evaluation of future PKU cases.
References
Avigad S, Cohen BE, Bauer S, Schwartz G, Frydman M, Woo SL, Niny Y, Shiloh Y (1990) A single origin of phenylketonuria in Yemenite Jews. Nature 344:168–170
Avigad S, Kleiman S, Weinstein M, Cohen BE, Schwartz G, Woo SL, Shiloh Y (1991) Compound heterozygosity in nonphenylketonuria hyperphenylalanemia: the contribution of mutations for classical phenylketonuria. Am J Hum Genet 49:393–399
Blau N (2003) BIOPKU: international database of patients and mutations causing tetrahydrobiopterin-responsive. HPA/PKU. http://www.bh4.org
Blau N, Erlandsen H (2004) The metabolic and molecular bases of tetrahydrobiopterin-responsive phenylalanine hydroxylase deficiency. Mol Genet Metab 82:101–111
Bercovich D, Beaudet AL (2003) Denaturing high-performance liquid chromatography for the detection of mutations and polymorphisms in UBE3A. Genet Test 7:189–194
Bercovich D, Elimelech A, Yardeni T, Korem S, Zlotogora J, Gal N, Goldstein N, Vilensky B, Segev R, Avraham S, Loewenthal R, Schwartz G, Anikster Y (2008) A mutation analysis of the phenylalanine hydroxylase (PAH) gene in the Israeli population. Ann Hum Genet AHG-07-0124 (in press)
DiLella AG, Kwok SC, Ledley FD, Marvit J, Woo SL (1986) Molecular structure and polymorphic map of the human phenylalanine hydroxylase gene. Biochemistry 25:743–749
Erlandsen H, Stevens RC (1999) The structural basis of phenylketonuria. Mol Genet Metab 68:103–125
Erlandsen H, Pey AL, Gamez A, Perez B, Desviat LR, Aguado C, Koch R, Surendran S, Tyring S, Matalon R, Scriver CR, Ugarte M, Martinez A, Stevens RC (2004) Correction of kinetic and stability defects by tetrahydrobiopterin in phenylketonuria patients with certain phenylalanine hydroxylase mutations. Proc Natl Acad Sci USA 101:16903–16908
Guldberg P, Henriksen KF, Guttler F (1993a) Molecular analysis of phenylketonuria in Denmark: 99% of the mutations detected by denaturing gradient gel electrophoresis. Genomics 17:141–146
Guldberg P, Romano V, Ceratto N, Bosco P, Ciuna M, Indelicato A, Mollica F, Meli C, Giovannini M, Riva E et al (1993b) Mutational spectrum of phenylalanine hydroxylase deficiency in Sicily: implications for diagnosis of hyperphenylalaninemia in southern Europe. Hum Mol Genet 2:1703–1707
Guldberg P, Rey F, Zschocke J, Romano V, Francois B, Michiels L, Ullrich K, Hoffmann GF, Burgard P, Schmidt H et al (1998) A European multicenter study of phenylalanine hydroxylase deficiency: classification of 105 mutations and a general system for genotype-based prediction of metabolic phenotype. Am J Hum Genet 63:71–79
Güttler F, Lou H (1990) Phenylketonuria and hyperphenylalaninemia. In: Fernandes J, Saudubray JM, Tada K (eds) Inborn metabolic disease: diagnosis and treatment. Springer, Berlin, pp 161–174
Kayaalp E, Treacy E, Waters PJ, Byck S, Nowacki P, Scriver CR (1997) Human phenylalanine hydroxylase mutations and hyperphenylalaninemia phenotypes: a meta-analysis of genotype–phenotype correlations. Am J Hum Genet 61:1309–1317
Kleiman S, Bernstein J, Schwartz G, Eisensmith RC, Woo SL, Shiloh Y (1992) A defective splice site at the phenylalanine hydroxylase gene in phenylketonuria and benign hyperphenylalaninemia among Palestinian Arabs. Hum Mutat 1:340–343
Kleiman S, Avigad S, Vanagaite L, Shmuelevitz A, David M, Eisensmith RC, Brand N, Schwartz G, Rey F, Munnich A et al (1994) Origins of hyperphenylalaninemia in Israel. Eur J Hum Genet 2:24–34
Kozak L, Blazkova M, Kuhrova V, Pijackova A, Ruzickova S, St’astna S (1997) Mutation and haplotype analysis of phenylalanine hydroxylase alleles in classical PKU patients from the Czech Republic: identification of four novel mutations. J Med Genet 34:893–898
Leuzzi V, Carducci C, Carducci C, Chiarotti F, Artiola C, Giovanniello A, Antonozzi I (2006) The spectrum of phenylalanine variations under tetrahydrobiopterin load in subjects affected by phenylalanine hydroxylase deficiency. J Inherit Metab Dis 29:38–46
Mallolas J, Vilaseca MA, Campistol J, Lambruschini N, Cambra FJ, Estivill X, Mila M (1999) Mutational spectrum of phenylalanine hydroxylase deficiency in the population resident in Catalonia: genotype–phenotype correlation. Hum Genet 105:468–473
O’Donnell KA, O’Neill C, Tighe O, Bertorelle G, Naughten E, Mayne PD, Croke DT (2002) The mutation spectrum of hyperphenylalaninaemia in the Republic of Ireland: the population history of the Irish revisited. Eur J Hum Genet 10:530–538
Okano Y, Eisensmith RC, Guttler F, Lichter-Konecki U, Konecki DS, Trefz FK, Dasovich M, Wang T, Henriksen K, Lou H et al (1991) Molecular basis of phenotypic heterogeneity in phenylketonuria. N Engl J Med 324:1232–1238
Scriver CR, Eisensmith RC, Woo SLC (1995) The hyperphenylalaninemias. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic and molecular basis of inherited disease, vol 1. McGraw-Hill, New York, pp 1015–1077
Song F, Qu YJ, Zhang T, Jin YW, Wang H, Zheng XY (2005) Phenylketonuria mutations in Northern China. Mol Genet Metab 86(1):107–118
Shlush LI, Behar DM, Zelazny A, Keller N, Lupski JR, Beaudet AL, Bercovich D (2002) Molecular epidemiological analysis of the changing nature of a meningococcal outbreak following a vaccination campaign. J Clin Microbiol 40:3565–3571
Waters PJ (2003) How PAH gene mutations cause hyper-phenylalaninemia and why mechanism matters: insights from in vitro expression. Hum Mutat 21:357–369
Weinstein M, Eisensmith RC, Abadie V, Avigad S, Lyonnet S, Schwartz G, Munnich A, Woo SL, Shiloh Y (1993) A missense mutation, S349P, completely inactivates phenylalanine hydroxylase in north African Jews with phenylketonuria. Hum Genet 90:645–649
Zschocke J, Hoffmann GF (1999) Phenylketonuria mutations in Germany. Hum Genet 104:390–398
Zschocke J (2003) Phenylketonuria mutations in Europe. Hum Mutat 21:345–356
Acknowledgments
The study was supported in part by grants from The Elsa and Leo Abramson Fund and The Rivka Nacht Fund for Research in Neurology. This study was part of a master’s degree at Tel Aviv University (AE). We also thank the Israeli PKU Family Foundation for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bercovich, D., Elimelech, A., Zlotogora, J. et al. Genotype–phenotype correlations analysis of mutations in the phenylalanine hydroxylase (PAH) gene. J Hum Genet 53, 407–418 (2008). https://doi.org/10.1007/s10038-008-0264-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-008-0264-4
Keywords
This article is cited by
-
The spectrum of phenylalanine hydroxylase variants and genotype–phenotype correlation in phenylketonuria patients in Gansu, China
Human Genomics (2023)
-
Spectrum of PAH gene mutations in 1547 phenylketonuria patients from Iran: a comprehensive systematic review
Metabolic Brain Disease (2021)
-
Mutation spectrum of PAH gene in phenylketonuria patients in Northwest China: identification of twenty novel variants
Metabolic Brain Disease (2019)
-
Analysis of the genotype-phenotype correlation in patients with phenylketonuria in mainland China
Scientific Reports (2018)
-
Molecular characterisation of phenylketonuria in a Chinese mainland population using next-generation sequencing
Scientific Reports (2015)