Abstract
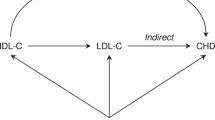
The ATP-binding cassette transporter A1 encoded by ABCA1 plays an integral role in the efflux of cellular cholesterol and phospholipids, but may also be a central mediator of β-amyloid (Aβ) processing. Here, genetic association of the common R219K variant of ABCA1 is shown with cerebrospinal fluid (CSF) Aβ1–42 levels, reinforcing emerging evidence of a connection between lipid and Aβ metabolism. In support of this finding we demonstrate for the first time that CSF cholesterol and Aβ1–42 are correlated. To affirm the plausible impact of ABCA1 variation on cholesterol and related traits as well as to empower a survey of possible interactions (e.g. age, gender, and smoking), a large Swedish population consisting of over 2,700 individuals was enlisted and extensive measures of plasma lipid parameters carried out. These analyses revealed that R219K has a strong effect on apolipoprotein B (APOB) and LDL-cholesterol (LDL-C) among smokers (P=0.000055 and P=0.00059, respectively), but not among non-smokers. In contrast, no effect was evident with apolipoprotein A (APOA1) or HDL-cholesterol (HDL-C) levels. Plasma APOB and LDL-C, but not APOA1 and HDL-C, were shown to be markedly elevated in smokers versus non-smokers, affirming that smoking may selectively impact the former pathway. No other genetic markers in ABCA1 exhibit effects as large as R219K, although a modest independent effect of R1587K was observed. Our data illuminate a possible genetic link between Aβ and cholesterol metabolism, but also provide an intriguing example of an environmental exposure that may modify a genotype–phenotype relationship.
Similar content being viewed by others
Introduction
A perturbation of lipid metabolism is likely to underlie a number of human diseases, and the discovery of genes and/or environmental exposures that differentially modulate this process stands to greatly improve knowledge of their aetiologies. This is exemplified by the finding that variants of the gene encoding apolipoprotein E (APOE) modify lipid levels (Yue et al. 2005;Viiri et al. 2005), which in turn contributes to Alzheimer’s disease (AD OMIM 104300) and cardiovascular disease (CVD) (Corder et al. 1993; Poirier et al. 1993; Strittmatter et al. 1993; Eichner et al. 2002). As well as directly impacting plasma lipid levels, APOE also strongly affects β-amyloid (Aβ) deposition in the brain (Beffert et al. 1999), suggesting a connection between Aβ, the main component of plaques, and apolipoprotein metabolism. In further support of this, another prominent phenotypic effect of APOE variation is upon cerebrospinal fluid (CSF) levels of the 42 amino acid fragment of β-amyloid (Aβ1–42) (Prince et al. 2004). In addition, other genes proven to influence AD (APP, PSEN1, and PSEN2) (Goate et al. 1991; Rogaev et al. 1995; Sherrington et al. 1995) have been shown to be involved in Aβ metabolism (Scheuner et al. 1996). On this basis, the search for genes that modify both Aβ and lipid processing may aid in understanding potentially overlapping biological mechanisms underlying CVD and AD.
The gene encoding the ATP binding cassette A1 transporter (ABCA1) has become widely studied in connection with CVD and related quantitative traits (Clee et al. 2001; Tregouet et al. 2004). Since the discovery that mutations in ABCA1 are the primary cause of Tangier disease (Brooks-Wilson et al. 1999; Bodzioch et al. 1999; Rust et al. 1999), in which HDL-cholesterol (HDL-C) levels are extremely low, several hundred articles have appeared describing the function of the protein, as well as attempts to associate common polymorphism in ABCA1 to cholesterol-related traits. The ABCA1 protein mediates the unidirectional efflux of free cholesterol and phospholipids from cells, facilitating the lipidation of most of the exchangeable apolipoproteins (including APOA1 and APOE) and the formation of nascent HDL molecules (Yancey et al. 2003). The ABCA1 protein has a wide tissue distribution (Wellington et al. 2002), but has been most studied in peripheral tissues. Recent studies have shown that deficiency of ABCA1 in the brain leads to a specific decrease in APOE levels (Hirsch-Reinshagen et al. 2004; Wahrle et al. 2004). Interestingly, ABCA1 shares a commonality with APOE in that it appears to be involved in Aβ metabolism (Fukumoto et al. 2002); this is supported by evidence suggesting a relationship between cholesterol metabolism and Aβ metabolism (Simons et al. 1998, 2001; Kojro et al. 2001). Emerging data thus suggest that ABCA1 plays an important role in lipid metabolism in both peripheral tissues and the central nervous system (CNS) and, like APOE, may also influence Aβ.
Genetic association studies on ABCA1 have been abundant, but have also left many questions unanswered. The accumulated literature supports the existence of functionally different alleles of ABCA1 that affect both discrete disease states (Singaraja et al. 2003) and quantitative traits (Wang et al. 2000; Clee et al. 2001; Frikke-Schmidt et al. 2004). One of the principal problems has been that the sample sizes of most studies have been small, typically entailing less than 1,000 individuals. In the present study, we have employed two different samples to explore the possible influence of ABCA1 sequence variants on both Aβ levels and on measures of lipid metabolism. For the latter in particular, we surveyed a large epidemiological sample to empower both the detection of genetic association and the illumination of possible interactions.
Materials and methods
Human subjects
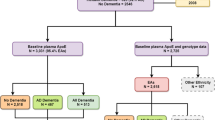
Swedish subjects for CSF analyses were recruited as part of a longitudinal geriatric population study in Piteå, Sweden (mean age-at-exam ±SD=75.4±7.8, n=226; 86 males and 140 females). More detailed descriptions of the subjects can be found elsewhere (Andreasen et al. 1999). This sample consists of both AD (n=156) and frontotemporal dementia (FTD) cases (n=70). This sample was not examined in our previous work on ABCA1 (Katzov et al. 2004). For analyses involving ANOVA, a sample identifier was included as a covariate to adjust for differences in average Aβ1–42 levels between AD and FTD groups. Clinical DNA samples employed in this study to explore for quantitative metabolic trait effects derive from individuals participating in the Stockholm Heart Epidemiology Program (SHEEP), a population based case-control study aimed at investigating the effects of various risk factors for myocardial infarction (MI) in men and women (Reuterwall et al. 1999). The subjects were aged 45–70 and were selected from the Stockholm County population registry (mean age-at-exam±SD=59.6±7.1). The sample consists of healthy controls (n=1,526; 1,033 males and 493 females) and individuals who have suffered a non-fatal, first MI event (n=1,177; 829 males and 348 females) (Bennet et al. 2003). Exposure information was obtained from a detailed questionnaire, and a health examination that included blood sampling and anthropometric tests. The latter was conducted at least 3 months after the MI event to allow metabolic stability to be regained (Hamsten et al. 1986). Current smokers were defined as those who smoked tobacco regularly, or had stopped within the last 2-year period. Former smokers were subjects who used to smoke regularly but who had stopped 2 or more years previously. Non-smokers were defined as those who reported never having smoked, or having smoked regularly for less than 1 year.
Genotyping
Information on the R219K, I883M, and R1587K variants [representing cDNA (GenBank accession number NM_005502.2) rs2230806, c.658 G>A; rs4149313, c.2650 A>G; rs2230808, c.4762 G>A, respectively] may be found at dbSNP (http://www.ncbi.nlm.nih.gov/SNP/). Genotyping was performed using Dynamic Allele Specific Hybridization (DASH) (Prince et al. 2001). DASH and PCR were performed using previously published oligonucleotide sequences and assay conditions (Katzov et al. 2004).
Cerebrospinal fluid collection and Aβ1–42 measurement
CSF samples were obtained by lumbar puncture in the L3/L4 or L4/L5 inter-space. Further details of CSF collection can be found elsewhere (Andreasen et al. 1999). CSF Aβ1–42 was determined using a sandwich ELISA (Innotest amyloid-β(1–42), Innogenetics, Ghent, Belgium) constructed to specifically measure Aβ1–42 (Vanderstichele et al. 1998).
Preparation for gas chromatography analysis of sterols
One microgram [26.26.26.27.27.27-2H6] cholesterol (10 μl from a stock solution of d6-cholesterol in cyclohexane; 0.1 mg/ml) and 2 ng racemic [23.23.24.25-2H4] 24-OH-cholesterol (Medical Isotopes, Pelham) and 4 ng [2H5] 27-OH-Chol [50 μl from a stock solution 40 ng 24S-hydroxycholesterol (24S-OH-Chol) and 80 ng 27-hydroxycholesterol per millilitre cyclohexane] were added as internal standards to 500 μl CSF. This solution was evaporated under nitrogen gas. After alkaline hydrolysis with 1 ml 1 M sodium hydroxide in 90% ethanol for 1 h at 50°C and addition of 1 ml distilled water, the sterols and oxysterols were extracted twice with 3 ml cyclohexane. The combined organic phases were dried under nitrogen at 60°C. The residue was dissolved in 160 μl n-decan. Eighty microlitres of the solution was transferred into a micro-vial for gas–liquid chromatography–mass spectrometric (GC–MS) analysis of cholesterol precursors, metabolites and plant sterols. Another 80 μl was diluted with 400 μl n-decan for analysis of cholesterol by gas–liquid chromatography–flame ionisation detection (GC–FID). The sterols and oxysterols were derivatised to trimethylsilyl-(TMSi) ethers by adding 40 μl TMSi-reagent (pyridine:hexamethyldisalazane:trimethylchlorosilane; 9:3:1, by volume; all reagents were supplied by Merck, Darmstadt, Germany) into each micro-vial and incubated for 1 h at 60°C.
Sterol analysis by GC-MS
Cholesterol, and the oxysterol 24S-OH-Chol, extracted from CSF samples was separated on a cross-linked methyl silicone DB-XLB 122–1232 fused silica capillary column (J&W Scientific, Folsom, CA) (30 m×0.25 mm i.d.×0.25 μm film thickness) in a HP 5890 Series II (Hewlett Packard, Los Angeles, CA) gas-chromatograph combined with a HP 5972 Series mass selective detector. An aliquot of 2 μl (or 3 μl for the CSF aliquot) was injected by automated injection (HP 7673 auto sampler and automatic injection) in splitless mode at an injection temperature of 280°C. Helium was used as the carrier gas with an inlet pressure of 1.03 bar. The initial oven temperature was kept at 150°C for 3 min; thereafter it was increased at a rate of 30°C/min to a final temperature of 290°C for 28 min. The temperature of the transfer line was kept at 280°C. Multiplier voltage was set to 2,650 eV (2,950 eV for CSF). Electron impact ionisation was employed at 70 eV. Selected-ion monitoring (SIM) was performed by cycling the quadrupole mass filter between the chosen m/z values at a rate of 2.5–5 (1.5–3 for CSF) cycles per second. TMSi-ether of 24S-OH-Chol was measured at m/z 413 (M+-OTMSi–CH(CH3)2) and deuterated 24S-OH-Chol at m/z 416 [M+-OTMSi–CD(CH3)2]. The concentrations of 24S-OH-Chol and cholesterol in CSF samples were calculated from standard curves using the corresponding deuterated compounds (isotope dilution method). Identity of all sterols was proven by comparison with the full scan mass spectra of authentic compounds. Additional qualifiers (characteristic fragment ions) were used for structural identification.
Statistical analysis
Deviation from Hardy–Weinberg equilibrium for genotypes at individual loci, as well as differences in genotype distributions between groups was assessed using the χ2 statistic. Tests for association of single marker genotypes with CSF Aβ1–42 levels and other metabolic quantitative traits were performed using analysis of variance (ANOVA), and significance of pair-wise comparisons were assessed using Fisher’s PLSD when F ratios were significant. Skewed traits (skewness>1.0) were log-transformed prior to analysis. The above statistical analyses were performed using StatView version 5.0 (Abacus Concepts). Haplotypes were estimated using PHASE v2.1 which implements a Bayesian method of haplotype estimation for unrelated individuals (Stephens et al. 2001; Stephens and Donnelly 2003). For estimation of empirical P values in case-control tests, 1,000 permutations were used with all other settings at default.
Results
We began by testing ABCA1 variants for a potential influence on CSF Aβ1–42 levels. We focussed on the R219K, I883M, and R1587K variants since these give rise to amino acid changes and because they are common in European populations (Clee et al. 2001). These are also among the most widely studied variants at this locus in relation to CVD phenotypes (Clee et al. 2001; Zwarts et al. 2002; Evans and Beil 2003; Srinivasan et al. 2003; Wollmer et al. 2003; Frikke-Schmidt et al. 2004; Tregouet et al. 2004). A significant effect of the R219K variant on CSF Aβ1–42 levels was observed whereby RK heterozygotes had the highest trait levels (547±19.2, n=141; 658±35.1, n=71; 443±60.6, n=4; F2,212=6.2, P=0.0024, for RR, RK, and KK genotype classes, respectively; pg/ml ±SEM). An age- and gender-adjusted model was not markedly different (F2,210=5.9, P=0.0031). The most significant pair-wise comparison was between the RR and RK classes (P=0.0007, Fisher’s PLSD post hoc test). Neither of the other markers exhibited significant effects on the CSF Aβ1–42 trait (data not shown). We also note that an independent AD study suggested that the R variant was associated with earlier age-at-onset (AAO) in AD (Wollmer et al. 2003). However, we observed no AAO effect in this sample, consistent with our previous observations (Katzov et al. 2004) (data not shown).
Although there is considerable literature suggesting a relationship between Aβ and lipid metabolism, to our knowledge no study has ever specifically tested whether cholesterol levels and Aβ are correlated, either in peripheral tissues or in the CNS. To address this question, we measured cholesterol and 24S-hydroxycholesterol (24S-OH-Chol) in CSF from 42 individuals from the above sample. Data depicting the correlation between Aβ1–42 and both cholesterol and 24S-OH-Chol are shown in Fig. 1. The modest significance reflects the small sample size, but we note that the effect size is large, with approximately 10% of the variance in each trait being explained by the other trait. Age and gender adjustment improved model fits slightly (P=0.016 for Aβ1–42 vs cholesterol, and P=0.0091 for Aβ1–42 vs 24S-OH-Chol). Not shown in the figure is the regression between cholesterol and 24S-OH-Chol, which is highly significant (r2=0.26, P=0.0006, N=42). Given the size of this sample, we did not attempt to explore for effects of ABCA1 variants on these measures of cholesterol.
We had difficulty obtaining additional CSF samples to replicate the finding of an effect of ABCA1 on Aβ1–42. However, presuming a possible fundamental relationship between cholesterol and Aβ metabolism, we considered the alternative approach of examining lipid traits in a large CVD sample instead. From available phenotypes, we selected six traits that are commonly examined in CVD studies (Table 1). In an initial screen, we tested the R219K variant using ANOVA for effects upon these selected traits in the entire set of samples. A few modest signals emerged from this analysis, including significant findings for LDL-cholesterol (LDL-C), total cholesterol (TC), and APOB levels (Table 1). Interaction terms were then included for age, gender, disease status (MI or control), and smoking (current smokers or non-smokers) in second-order factorial ANOVA models, testing all three of these traits. Among these, the interaction term for smoking was significant for the APOB trait and thus stratified analyses were performed in smokers and non-smokers. The results of this analysis were highly significant in the smoking group but not in non-smokers (Table 2). On this basis, we also tested the LDL-C and TC traits, which were both significantly but modestly associated with R219K in smokers (P=0.031 and P=0.019, respectively), but not in non-smokers (Table 2). Notably, the data for the effect of R219K on APOB were similar to those for Aβ1–42, whereby heterozygote levels differed from both homozygote groups, but in a non-additive fashion (i.e. the heterozygous class did not fall midway between opposite homozygotes).
The model for the effect of R219K on APOB and CSF Aβ1–42 suggested by the above data implies either heterosis (Comings and MacMurray 2000) or a possible interaction with other variants in ABCA1 (or a nearby gene). To begin exploring this latter possibility in the CVD sample (since it affords the most power to detect such effects), genotyping of the I883M and R1587K variants was performed, and ANOVA used to model the potential independent main effects in a joint analysis of all three markers (including R219K). We noted that LD is very weak between these sites (Katzov et al. 2004) and therefore assumed that colinearity would likely not be a problem. In smokers, the main effect for R219K improved when adjusting for the other sites from F2,943=8.4, P=0.00024 in isolation to F2,898=9.9, P=0.000055 when all three markers were included. An independent effect for the R1587K variant was also noted in the full model (F2,898=3.8, P=0.023). The I883M variant was not associated with the APOB trait either in isolation or in the full model. A final model was also constructed including all three markers and age, gender, and case-control status as covariates. The main effect of the R219K variant was not markedly changed in this analysis (F2,895=9.6, P=0.000077). None of the markers were significantly associated with APOB levels in non-smokers.
Having provided evidence of their potential independent effects, we used a diplotype strategy (Gu et al. 2004) to test for interactions between the R219K and R1587K variants, focussing on the smoking population. This strategy allows testing of haplotype effects, and can expose hybrids (individuals with two unlike haplotypes) that may contribute to trait variance. For this, we used PHASE v2.1 (Stephens et al. 2001; Stephens and Donnelly 2003), which produced estimates of approximately 0.7 probability for all heterozygous individuals. We note for reference that this strategy is essentially identical to the strategy that has long been used with APOE, whereby two sites distinguish the ε2, ε3, and ε4 alleles and their diplotype configurations. The results from this analysis were highly significant (F7,905=4.7, P=0.000037) and are shown in Fig. 2. Given the uncertainty of the double heterozygote class, it was excluded in an additional model, which did not markedly alter significance (F6,776=4.9, P=0.000057).
Diplotype analysis of quantitative traits considering the joint contributions of the R219K and R1587K variants. Categories represent the diplotype configurations of each individual from among four possible haplotypes (RR, KK, RK, and KR, where R219K is at the first position). Values shown are mean ±SEM. F ratios from ANOVA omnibus tests and associated P values are shown in the upper-right corner of each panel. The number of individuals in each category is shown below each column. The highest trait levels occur in individuals that are homozygous for the K variant of R219K and homozygous for the R variant of R1587K. LDL-C Low density lipoprotein cholesterol
We also tested the R219K, I883M, and R1587K markers for association with MI risk in the whole sample and in smokers and non-smokers. Among these tests, the only significant finding to emerge was modest significance for R1587K in the smoking population (P=0.025) (Table 3). Diplotype distributions (constructed with R219K and R1587K) between cases and controls in the smoking population were not significantly different (data not shown). We further tested whether ABCA1 haplotype distributions were different in MI versus control samples using PHASE v2.1 but found no significant effects in the whole sample or in either smokers and non-smokers (data not shown).
The primary outstanding question from this study is how smoking and ABCA1 might be interacting to affect lipid profiles. We note that smoking has long been known to influence lipid metabolism (Doll and Hill 1996; Talmud and Humphries 2002) but to specifically address this question here we tested for differences in six lipid-related traits between smokers and non-smokers. We adjusted for gender, age, and disease status (MI or control), and found highly significant differences for APOB, LDL-C, TC, and TG (triglycerides), but not for APOA1 and HDL-C. The strongest difference was observed for APOB levels (F1,2624=25.1, P=0.00000058; 1.514±0.009 mean g/l ±SEM for non-smokers and 1.608±0.013 for smokers). Importantly, in examining the data for the effect of ABCA1 on APOB levels shown in Table 2, we note that there is no significant difference in the heterozygote class between smokers and non-smokers (F1,923=2.1, P=0.14). This contrasts with the differences in the rare allele homozygous class (F1,150=9.4, P=0.0025) and the common-allele homozygous class (F1,1400=20.4, P=0.0000068). Thus, the lack of effect in heterozygotes does not appear to derive from the smaller number of individuals in this category compared to common-allele homozygotes, since rare-allele homozygotes do exhibit a highly significant difference between smokers and non-smokers.
To explore the possible functional effects of ABCA1 variants, we used the PolyPhen tool (http://www.bork.embl-heidelberg.de/PolyPhen/) (Ramensky et al. 2002) for five coding SNPs (cSNPs) in ABCA1 (R219K rs2230806; V771M rs2066718; V825I rs4149312; I883M rs2066714; R1587K rs2230808) (Frikke-Schmidt et al. 2004). As a control we also tested the APOE-ε4 (R130C rs428358) variant. We found the predicted effects of all the tested cSNPs in ABCA1 to be benign (i.e. most likely lacking any phenotypic effect), whilst the functional effect of the APOE-ε4 (rs428358) variant was predicted to be probably damaging.
Finally, we tallied the number of statistical hypothesis tested in this study in its entirety. There were 57 independent tests; note that applying a strict Bonferroni correction for multiple testing does not eliminate the significance of the primary findings for either CSF Aβ1–42 (P=0.0007uncorrected and P=0.04corrected) or APOB levels (P=0.000037uncorrected and P=0.0021corrected).
Discussion
We have previously shown that CSF Aβ1–42 is robustly affected by polymorphism in APOE (Prince et al. 2004), the most widely replicated genetic risk factor for AD, and have thus presumed that other true AD-modifying genes might also exhibit effects upon Aβ metabolism. That ABCA1 can directly influence Aβ has been demonstrated (Fukumoto et al. 2002), and more recent evidence suggests that ABCA1 also interacts with APOE in the CNS (Hirsch-Reinshagen et al. 2004). In the present study, we suggest that genetic variants of ABCA1 may influence CSF Aβ1–42 levels, possibly reflecting its involvement with Aβ metabolism. This is supported by the finding here that Aβ1–42 and cholesterol levels are correlated in CSF. Thus, ABCA1 shares a similarity with APOE in that both appear to be involved in lipid and Aβ metabolism.
To further investigate the potential consequences of ABCA1 variation on lipid metabolism, we examined a large CVD sample, focussing on six commonly studied lipid traits. Since its discovery as the cause of Tangier disease (Brooks-Wilson et al. 1999; Bodzioch et al. 1999; Rust et al. 1999), many genetic association studies have been performed providing evidence that common polymorphism in ABCA1 impacts cholesterol-related phenotypes, the most replicable of which is plasma HDL-C level (Clee et al. 2001). However, not all studies have demonstrated effects upon HDL-C levels (Kakko et al. 2003). One of the primary weaknesses of prior genetic association studies on ABCA1 has been that sample sizes have been relatively small. The results of the present investigation suggest that variants of ABCA1 primarily affect APOB levels given that there was no evidence for effects upon HDL-C or APOA1 levels, the two principal phenotypes for which several prior studies suggest association (Wang et al. 2000; Srinivasan et al. 2003; Tregouet et al. 2004). Studies in animal models point to several phenotypes that are affected by ABCA1 modification, including plasma APOB levels, which has been shown both in transgenic mice (Vaisman et al. 2001) and more recently in studies exploiting RNA interference (Ragozin et al. 2005). In the present study, significant effects were also evident for LDL-C and TC levels, but this is perhaps unsurprising given the strong correlations of these traits with APOB. Our findings nonetheless illuminate the question of what specific phenotypes may be best suited to provide evidence that a particular pathway is affected by a gene. The consideration of multiple lipid-related traits in future studies will probably be essential to resolving this question.
An intriguing aspect of these findings was that effects appear to occur only in individuals who smoke. One prior study did suggest stronger effects of R219K upon coronary heart disease in smokers (Cenarro et al. 2003). In contrast, one of the most comprehensive studies to date on ABCA1 variation found an association with MI exclusively in non-smokers (Tregouet et al. 2004). Thus, it appears possible that smoking modifies the phenotypic effects of ABCA1, but the nature of the interaction is unclear at present. This may have a bearing on the success or failure of future studies that attempt to relate ABCA1 variation to other disease phenotypes, but may also serve as a point to revisit in large published studies, such as that of Frikke-Schmidt et al. (2004). In particular, our own results on AD (Katzov et al. 2004) and on CSF Aβ1–42 levels in the present study may be influenced by this potential modification. Unfortunately, it is uncommon for AD sample collection strategies to include information about smoking or other lifestyle data, and this is admittedly true for the majority of our own samples. Larger studies on ABCA1 in AD are ongoing in samples from the Swedish Twin Registry (Lichtenstein et al. 2002), for which these kinds of data are available, and should help to resolve this issue. This and other studies that consider smoking should help illuminate an appropriate genetic model to facilitate further replication efforts. This will be necessary in order to corroborate findings across phenotypes (for example, earlier observations of modest effects on senile plaque load in the AD brain) (Katzov et al. 2004).
The extent of local sequence variation in ABCA1 is fairly well resolved after a number of exhaustive DNA sequencing efforts (Wang et al. 2000; Tregouet et al. 2004). Among discovered and examined variable sites, the best evidence for potentially functional polymorphism is for the commonly studied R219K and R1587K variants (Tregouet et al. 2004). Interestingly, pair-wise linkage disequilibrium for variants in ABCA1 is fairly weak (Katzov et al. 2004; Tregouet et al. 2004), and on this basis it is intriguing that studies have found sporadic effects of these particular markers on different phenotypes. Discrepancies of this nature may reflect low power in a study but might also indicate allelic heterogeneity in the region (i.e. two or more functional variants). In support of this latter possibility, we obtained evidence that R219K and R1587K have independent effects upon plasma APOB levels and our data indicate that there may be complex interactions between the two variants. In addition to these common variants, there is also evidence that rare mutations in ABCA1 can often be a cause of extremely low HDL-C levels in the population (Cohen et al. 2004), but the extent to which these contribute to more normal variation is still unknown. We acknowledge that promoter or other regulatory regions may also be important, but more comprehensive studies would be needed to test these effects.
In summary, substantial evidence that Aβ and cholesterol metabolism are tightly linked exists (Hartmann 2001; Simons et al. 2001), and the data presented here on a potential role for genetic variants of ABCA1 supports this. We believe that continued efforts to map AD and CVD susceptibility genes will benefit from the joint consideration of both AD- and CVD-related phenotypes, especially those connected to cholesterol metabolism. Given the extent of positive published data on ABCA1, there is a high likelihood that functionally relevant sequence variation occurs in this genomic region, but it may most appropriately be explored further in the context of potential modification by allelic and environmental heterogeneity.
References
Andreasen N, Hesse C, Davidsson P, Minthon L, Wallin A, Winblad B, Vanderstichele H, Vanmechelen E, Blennow K (1999) Cerebrospinal fluid beta-amyloid(1–42) in Alzheimer’s disease: differences between early- and late-onset Alzheimer’s disease and stability during the course of disease. Arch Neurol 56:673–680
Beffert U, Aumont N, Dea D, Lussier-Cacan S, Davignon J, Poirier J (1999) Apolipoprotein E isoform-specific reduction of extracellular amyloid in neuronal cultures. Brain Res Mol Brain Res 68:181–185
Bennet AM, Prince JA, Fei GZ, Lyrenas L, Huang Y, Wiman B, Frostegard J, Faire U (2003) Interleukin-6 serum levels and genotypes influence the risk for myocardial infarction. Atherosclerosis 171:359–367
Bodzioch M, Orso E, Klucken J, Langmann T, Bottcher A, Diederich W, Drobnik W, Barlage S, Buchler C, Porsch-Ozcurumez M, Kaminski WE, Hahmann HW, Oette K, Rothe G, Aslanidis C, Lackner KJ, Schmitz G (1999) The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. Nat Genet 22:347–351
Brooks-Wilson A, Marcil M, Clee SM, Zhang LH, Roomp K, van Dam M, Yu L, Brewer C, Collins JA, Molhuizen HO, Loubser O, Ouelette BF, Fichter K, Ashbourne-Excoffon KJ, Sensen CW, Scherer S, Mott S, Denis M, Martindale D, Frohlich J, Morgan K, Koop B, Pimstone S, Kastelein JJ, Hayden MR (1999) Mutations in ABC1 in Tangier disease and familial high-density lipoprotein deficiency. Nat Genet 22:336–345
Cenarro A, Artieda M, Castillo S, Mozas P, Reyes G, Tejedor D, Alonso R, Mata P, Pocovi M, Civeira F (2003) A common variant in the ABCA1 gene is associated with a lower risk for premature coronary heart disease in familial hypercholesterolaemia. J Med Genet 40:163–168
Clee SM, Zwinderman AH, Engert JC, Zwarts KY, Molhuizen HO, Roomp K, Jukema JW, van Wijland M, van Dam M, Hudson TJ, Brooks-Wilson A, Genest J Jr, Kastelein JJ, Hayden MR (2001) Common genetic variation in ABCA1 is associated with altered lipoprotein levels and a modified risk for coronary artery disease. Circulation 103:1198–1205
Cohen JC, Kiss RS, Pertsemlidis A, Marcel YL, McPherson R, Hobbs HH (2004) Multiple rare alleles contribute to low plasma levels of HDL cholesterol. Science 305:869–872
Comings DE, MacMurray JP (2000) Molecular heterosis: a review. Mol Genet Metab 71:19–31
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261:921–923
Doll R, Hill AB (1996) Mortality of British doctors in relation to smoking: observations on coronary thrombosis. Natl Cancer Inst Monogr 19:205–268
Eichner JE, Dunn ST, Perveen G, Thompson DM, Stewart KE, Stroehla BC (2002) Apolipoprotein E polymorphism and cardiovascular disease: a HuGE review. Am J Epidemiol 155:487–495
Evans D, Beil FU (2003) The association of the R219K polymorphism in the ATP-binding cassette transporter 1 (ABCA1) gene with coronary heart disease and hyperlipidaemia. J Mol Med 81:264–270
Frikke-Schmidt R, Nordestgaard BG, Jensen GB, Tybjaerg-Hansen A (2004) Genetic variation in ABC transporter A1 contributes to HDL cholesterol in the general population. J Clin Invest 114:1343–1353
Fukumoto H, Deng A, Irizarry MC, Fitzgerald ML, Rebeck GW (2002) Induction of the cholesterol transporter ABCA1 in central nervous system cells by liver X receptor agonists increases secreted Abeta levels. J Biol Chem 277:48508–48513
Goate A, Chartier-Harlin MC, Mullan M, Brown J, Crawford F, Fidani L, Giuffra L, Haynes A, Irving N, James L (1991) Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature 349:704–706
Gu HF, Efendic S, Nordman S, Ostenson CG, Brismar K, Brookes AJ, Prince JA (2004) Quantitative trait loci near the insulin-degrading enzyme (IDE) gene contribute to variation in plasma insulin levels. Diabetes 53:2137–2142
Hamsten A, Iselius L, Dahlen G, de Faire U (1986) Genetic and cultural inheritance of serum lipids, low and high density lipoprotein cholesterol and serum apolipoproteins A-I, A-II and B. Atherosclerosis 60:199–208
Hartmann T (2001) Cholesterol, A beta and Alzheimer’s disease. Trends Neurosci 24:S45–S48
Hirsch-Reinshagen V, Zhou S, Burgess BL, Bernier L, McIsaac SA, Chan JY, Tansley GH, Cohn JS, Hayden MR, Wellington CL (2004) Deficiency of ABCA1 impairs apolipoprotein E metabolism in brain. J Biol Chem 279:41197–41207
Kakko S, Kelloniemi J, von Rohr P, Hoeschele I, Tamminen M, Brousseau ME, Kesaniemi YA, Savolainen MJ (2003) ATP-binding cassette transporter A1 locus is not a major determinant of HDL-C levels in a population at high risk for coronary heart disease. Atherosclerosis 166:285–290
Katzov H, Chalmers K, Palmgren J, Andreasen N, Johansson B, Cairns NJ, Gatz M, Wilcock GK, Love S, Pedersen NL, Brookes AJ, Blennow K, Kehoe PG, Prince JA (2004) Genetic variants of ABCA1 modify Alzheimer’s disease risk and quantitative traits related to beta-amyloid metabolism. Hum Mutat 23:358–367
Kojro E, Gimpl G, Lammich S, Marz W, Fahrenholz F (2001) Low cholesterol stimulates the nonamyloidogenic pathway by its effect on the alpha-secretase ADAM 10. Proc Natl Acad Sci USA 98:5815–5820
Lichtenstein P, De Faire U, Floderus B, Svartengren M, Svedberg P, Pedersen NL (2002) The Swedish Twin Registry: a unique resource for clinical, epidemiological and genetic studies. J Intern Med 252:184–205
Poirier J, Davignon J, Bouthillier D, Kogan S, Bertrand P, Gauthier S (1993) Apolipoprotein E polymorphism and Alzheimer’s disease. Lancet 342:697–699
Prince JA, Feuk L, Howell WM, Jobs M, Emahazion T, Blennow K, Brookes AJ (2001) Robust and accurate single nucleotide polymorphism genotyping by dynamic allele-specific hybridization (DASH): design criteria and assay validation. Genome Res 11:152–162
Prince JA, Zetterberg H, Andreasen N, Marcusson J, Blennow K (2004) APOE epsilon4 allele is associated with reduced cerebrospinal fluid levels of Abeta42. Neurology 62:2116–2118
Ragozin S, Niemeier A, Laatsch A, Loeffler B, Merkel M, Beisiegel U, Heeren J (2005) Knockdown of hepatic ABCA1 by RNA interference decreases plasma HDL cholesterol levels and influences postprandial lipemia in mice. Arterioscler Thromb Vasc Biol 25:1–7
Ramensky V, Bork P, Sunyaev S (2002) Human non-synonymous SNPs: server and survey. Nucleic Acids Res 30:3894–3900
Reuterwall C, Hallqvist J, Ahlbom A, De Faire U, Diderichsen F, Hogstedt C, Pershagen G, Theorell T, Wiman B, Wolk A (1999) Higher relative, but lower absolute risks of myocardial infarction in women than in men: analysis of some major risk factors in the SHEEP study. The SHEEP Study Group. J Intern Med 246:161–174
Rogaev EI, Sherrington R, Rogaeva EA, Levesque G, Ikeda M, Liang Y, Chi H, Lin C, Holman K, Tsuda T (1995) Familial Alzheimer’s disease in kindreds with missense mutations in a gene on chromosome 1 related to the Alzheimer’s disease type 3 gene. Nature 376:775–778
Rust S, Rosier M, Funke H, Real J, Amoura Z, Piette JC, Deleuze JF, Brewer HB, Duverger N, Denefle P, Assmann G (1999) Tangier disease is caused by mutations in the gene encoding ATP-binding cassette transporter 1. Nat Genet 22:352–355
Scheuner D, Eckman C, Jensen M, Song X, Citron M, Suzuki N, Bird TD, Hardy J, Hutton M, Kukull W, Larson E, Levy-Lahad E, Viitanen M, Peskind E, Poorkaj P, Schellenberg G, Tanzi R, Wasco W, Lannfelt L, Selkoe D, Younkin S (1996) Secreted amyloid beta-protein similar to that in the senile plaques of Alzheimer’s disease is increased in vivo by the presenilin 1 and 2 and APP mutations linked to familial Alzheimer’s disease. Nat Med 2:864–870
Sherrington R, Rogaev EI, Liang Y, Rogaeva EA, Levesque G, Ikeda M, Chi H, Lin C, Li G, Holman K (1995) Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature 375:754–760
Simons M, Keller P, De Strooper B, Beyreuther K, Dotti CG, Simons K (1998) Cholesterol depletion inhibits the generation of beta-amyloid in hippocampal neurons. Proc Natl Acad Sci USA 95:6460–6464
Simons M, Keller P, Dichgans J, Schulz JB (2001) Cholesterol and Alzheimer’s disease: is there a link? Neurology 57:1089–1093
Singaraja RR, Brunham LR, Visscher H, Kastelein JJ, Hayden MR (2003) Efflux and atherosclerosis: the clinical and biochemical impact of variations in the ABCA1 gene. Arterioscler Thromb Vasc Biol 23:1322–1332
Srinivasan SR, Li S, Chen W, Boerwinkle E, Berenson GS (2003) R219K polymorphism of the ABCA1 gene and its modulation of the variations in serum high-density lipoprotein cholesterol and triglycerides related to age and adiposity in white versus black young adults. The Bogalusa heart study. Metabolism 52:930–934
Stephens M, Donnelly P (2003) A comparison of Bayesian methods for haplotype reconstruction from population genotype data. Am J Hum Genet 73:1162–1169
Stephens M, Smith NJ, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS, Roses AD (1993) Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer’s disease. Proc Natl Acad Sci USA 90:1977–1981
Talmud PJ, Humphries SE (2002) Gene:environment interaction in lipid metabolism and effect on coronary heart disease risk. Curr Opin Lipidol 13:149–154
Tregouet DA, Ricard S, Nicaud V, Arnould I, Soubigou S, Rosier M, Duverger N, Poirier O, Mace S, Kee F, Morrison C, Denefle P, Tiret L, Evans A, Deleuze JF, Cambien F (2004) In-depth haplotype analysis of ABCA1 gene polymorphisms in relation to plasma ApoA1 levels and myocardial infarction. Arterioscler Thromb Vasc Biol 24:775–781
Vaisman BL, Lambert G, Amar M, Joyce C, Ito T, Shamburek RD, Cain WJ, Fruchart-Najib J, Neufeld ED, Remaley AT, Brewer HB Jr, Santamarina-Fojo S (2001) ABCA1 overexpression leads to hyperalphalipoproteinemia and increased biliary cholesterol excretion in transgenic mice. J Clin Invest 108:303–309
Vanderstichele HBK, D’Heuvaert N, Buyse MA, Wallin A, Andreasen N, Seubert PVDVA, Vanmechelen E (1998) Development of a specific diagnostic test for the measurement of beta-amyloid(1–42) in CSF. In: Fisher A, Hanin I, Yoshida M (eds) Progress in Alzheimer’s and Parkinson’s diseases. Plenum, New York
Viiri LE, Loimaala A, Nenonen A, Islam S, Vuori I, Karhunen PJ, Lehtimaki T (2005) The association of the apolipoprotein E gene promoter polymorphisms and haplotypes with serum lipid and lipoprotein concentrations. Atherosclerosis 179:161–167
Wahrle SE, Jiang H, Parsadanian M, Legleiter J, Han X, Fryer JD, Kowalewski T, Holtzman DM (2004) ABCA1 is required for normal central nervous system ApoE levels and for lipidation of astrocyte-secreted apoE. J Biol Chem 279:40987–40993
Wang J, Burnett JR, Near S, Young K, Zinman B, Hanley AJ, Connelly PW, Harris SB, Hegele RA (2000) Common and rare ABCA1 variants affecting plasma HDL cholesterol. Arterioscler Thromb Vasc Biol 20:1983–1989
Wellington CL, Walker EK, Suarez A, Kwok A, Bissada N, Singaraja R, Yang YZ, Zhang LH, James E, Wilson JE, Francone O, McManus BM, Hayden MR (2002) ABCA1 mRNA and protein distribution patterns predict multiple different roles and levels of regulation. Lab Invest 82:273–283
Wollmer MA, Streffer JR, Lutjohann D, Tsolaki M, Iakovidou V, Hegi T, Pasch T, Jung HH, Bergmann K, Nitsch RM, Hock C, Papassotiropoulos A (2003) ABCA1 modulates CSF cholesterol levels and influences the age at onset of Alzheimer’s disease. Neurobiol Aging 24:421–426
Yancey PG, Bortnick AE, Kellner-Weibel G, de la Llera-Moya M, Phillips MC, Rothblat GH (2003) Importance of different pathways of cellular cholesterol efflux. Arterioscler Thromb Vasc Biol 23:712–719
Yue P, Isley WL, Harris WS, Rosipal S, Akin CD, Schonfeld G (2005) Genetic variants of ApoE account for variability of plasma low-density lipoprotein and apolipoprotein B levels in FHBL. Atherosclerosis 178:107–113
Zwarts KY, Clee SM, Zwinderman AH, Engert JC, Singaraja R, Loubser O, James E, Roomp K, Hudson TJ, Jukema JW, Kastelein JJ, Hayden MR (2002) ABCA1 regulatory variants influence coronary artery disease independent of effects on plasma lipid levels. Clin Genet 61:115–125
Acknowledgements
Financial support was provided by Pfizer Inc., The Swedish Medical Research Council, Loo and Hans Ostermans Foundation, The Swedish Old Servants Foundation (Gamla Tjänarinnor), Åke Wibergs Foundation, Torsten and Ragnar Söderbergs Foundation, Fredrik and Ingrid Thurings Foundation, The Swedish Alzheimer’s Foundation (Alzheimer’sfonden), and the Swedish Heart and Lung Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katzov, H., Bennet, A.M., Höglund, K. et al. Quantitative trait loci in ABCA1 modify cerebrospinal fluid amyloid-β1-42 and plasma apolipoprotein levels. J Hum Genet 51, 171–179 (2006). https://doi.org/10.1007/s10038-005-0341-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-005-0341-x
Keywords
This article is cited by
-
Association between the ABCA1 (R219K) polymorphism and lipid profiles: a meta-analysis
Scientific Reports (2021)
-
Association studies of several cholesterol-related genes (ABCA1, CETP and LIPC) with serum lipids and risk of Alzheimer’s disease
Lipids in Health and Disease (2012)