Abstract
Mutations in the human gene encoding rapsyn have been linked to a recessive form of postsynaptic congenital myasthenic syndrome due to deficient clustering of acetylcholine receptors at the endplate. All patients reported to date carry the N88K mutation, suggesting a possible common founder effect. To decrease the likelihood of a recombination event occurring within the span of neighboring microsatellite markers, we used seven intragenic single nucleotide polymorphisms (SNPs) spanning 8 kb to characterize the haplotype associated with N88K. In three affected N88K homozygous individuals, we identified a common haplotype present in all heterozygous carriers of N88K. Of note, in two asymptomatic N88K homozygous individuals, a second haplotype was present that differed at three SNP sites downstream from the N88K mutation. Our findings of a common haplotype associated with the N88K mutation support a founder effect. The discordant haplotype found in homozygous individuals suggests that recombination events may have occurred within the rapsyn gene and that this may have implications in the phenotypic expression of the disease.
Similar content being viewed by others
Introduction
Rapsyn is a 43-kDa postsynaptic protein that plays a fundamental role in the process of aggregation of acetylcholine receptors (AChRs) at the postsynaptic membrane. Rapsyn knockout mice have shown deficiency in AChR clustering (Gautam et al. 1999) with an inability to bind β-dystroglycan (Gautam et al. 1995), leading to impaired neuromuscular transmission.
Recently, Ohno et al. (2002) reported four patients with congenital myasthenic syndromes (CMSs) with recessive mutations in the rapsyn gene (RAPSN). Since then, we (Dunne and Maselli 2003) and others (Muller et al. 2003; Richard et al. 2003) have confirmed this initial observation with further reports of CMS patients due to mutations in RAPSN. Of note, all patients reported to date carry the N88K allele, either homozygous or heteroallelic, with a second mutation, with the exception of those with mutations in the RAPSN promoter region (Ohno et al. 2003). This unusual fact has prompted the question of a common founder for the N88K mutation.
Two research groups (Muller et al. 2003; Richard et al. 2003) have addressed the question of a common founder for the N88K mutation by haplotype analysis using microsatellite markers ranging from 4.2 Mb upstream to 0.9 Mb downstream RAPSN. Both studies showed the possibility of a common founder for the N88K mutation, as a consistent haplotype was seen in about 80% of carrier individuals; however, these were inconclusive studies, as 20% of patients and individuals who carried the mutation did not show the same haplotype. Muller et al. (2003) suggested that this was because in those individuals, the mutation arose spontaneously. An alternate hypothesis would be that the discordant haplotypes resulted from a recombination event occurring between the haplotype markers. To address this question, we conducted a haplotype analysis of patients and individuals carrying the N88K mutation using intragenic markers ranging 8 kb to minimize the probability of a recombination event occurring between the markers. Because there are no microsatellite markers within the rapsyn gene, seven single nucleotide polymorphisms (SNPs) were interrogated and statistically analyzed to determine a common haplotype. This haplotype was present in all patients and relatives who carried the N88K mutation, except in two N88K homozygous individuals who were asymptomatic for the disease. The discordant haplotypes occurring in these two individuals suggest that a recombination event can occur intragenically, even in a short span of the rapsyn gene (8 kb).
Materials and methods
Haplotype analysis
Patients
We studied six patients with symptoms of CMS since birth from six independent families who carried the N88K mutation. Three patients were homozygous for the mutation, and three were heterozygous and carried a second mutation (L14P, 46insC, or Y269X). The clinical backgrounds of these patients were reported elsewhere (Maselli et al. 2003). The study also included asymptomatic parents and siblings who carried the N88K mutation. Two families were from Spain; one family was Hindu; three families were of northern European descent. The two homozygous N88K mothers who were asymptomatic were 33 and 58 years old. One was from Spain, and the other was of northern European descent.
SNP identification
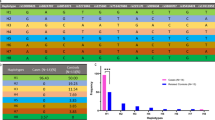
We chose seven previously reported (Ohno et al. 2002, 2003) intragenic SNPs to be used in this study. These SNPs include 172C/T in exon 1 (SNP 1), 264C/A in exon 2 (SNP 2), 456T/C in exon 2 (SNP 3), 855G/A in exon 5 (SNP 4), 1143T/C in exon 7 (SNP 5), IVS7+185G/A in intron 7 (SNP 6), and IVS7+278A/G also in intron 7 (SNP 7, Fig. 1). All SNPs showed no codon variation except 172C/T, which led to R57C and 264C/A, which led to N88K.
SNP positions in RAPSN. a Displayed are the eight exons of RAPSN and the location of each of the seven single nucleotide polymorphisms (SNPs), with the name of the SNP above the map and the number of the SNP below the map. Note SNP 2: 264C/T, is the N88K mutation. The 100 bp marker applies to exons. b The table lists each of the seven SNPs with their position, nucleotide change, and distance from the interrogated N88K mutation
PCR
DNA was extracted from intravenously drawn blood samples using QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA). PCR was carried out with primers designed to amplify exons 1, 2, 5, 7 and intron 7 of the RAPSN (GenBank accession number 008978 and Z33905). PCR was run using a reaction mixture including a 1× buffer that contained Tris–HCl, KCl, and Triton X-100, 25 mm MgCl2, 10 mm dNTPs, 100 pmol/μl sense primer, 100 pmol/μl antisense primer, 600 ng genomic DNA, and 2.5 U Taq DNA polymerase (Promega, Madison, WI, USA) in 50 μl total volume. The reactions were run on a thermal cycler using a cycling protocol consisting of initial denaturing at 95°C for 5 min, then 30 cycles of 95°C for 30 s, 60°C for 1 min, and 72°C for 1 min 30 s, then a final extension at 72°C for 5 min. These PCR products were then run on a 1% agarose gel, stained with ethidium bromide, then exposed to UV light to visualize the DNA. The products were purified using the QIAquick Gel Extraction Kit (Qiagen).
Minisequencing
Primers were designed immediately 5′ of SNPs 3, 4, and 5 located in exons 2, 5, and 7 (Table 1). The primers were designed with a 5′ random sequence tail of varying lengths to give total primer lengths of 28, 36, and 44 bp to allow for multiplexing. The purified PCR products were used as templates for minisequencing reactions using the SNaPshot minisequencing kit from Applied Biosystems. The cycling protocol consisted of 35 cycles of 96°C for 10 s, 50°C for 5 s, and 60°C for 30 s, and the samples were held at 4°C until postextension treatment. Samples were then incubated for 1 h at 37°C with 1 U calf intestinal phosphatase to remove the 5′ phosphoryl groups from the unincorporated ddNTPs, then 75°C for 15 min to deactivate the enzyme. Samples were sequenced using the ABI Prism 3100 Genetic Analyzer to determine the fluorescence at each SNP site, and then a GeneScan computer program automatically determined the corresponding ddNTP incorporated at the sites.
Restriction digest
SNPs 1, 6, and 7 located in exon 1 and intron 7 were analyzed in all patients and 50 controls using restriction enzyme digestion. After PCR amplification, 50 ng exon 1 amplicons were digested with 10 U HaeIII restriction enzyme (New England Biolabs, Beverly, MA, USA) and 1× NEBuffer 2 in 20 μl total reaction mix to interrogate SNP 172C/T. The reaction was incubated at 37°C for 1 h then run on a 4% agarose gel and viewed with ethidium bromide staining and UV illumination. To determine the allele at SNP IVS7+185G/A, 50 ng intron 7 amplicons were digested with 10 U SmaI restriction enzyme (Promega, Madison, WI, USA), 1× Buffer J and 0.1 mg/ml BSA in 20 ul total reaction mix. The digest was left at 25°C for 1 h then viewed as described above. 50 ng intron 7 amplicons were separately digested with 10 U AluI restriction enzyme and 1× NEBuffer 3 in a 20 μl reaction mix to determine the allele at SNP IVS7+278A/G. The reaction was incubated at 37°C for 1 h then viewed as described above.
SNP analysis
Results of the minisequencing and restriction analysis were tabulated using an Excel program, and the haplotypes were determined based on pedigrees.
Results
Minisequencing and restriction digests in each of the three N88K homozygous patients revealed the alleles C/C at SNP 1, A/A at SNP 2, C/C at SNP 3, G/G at SNP 4, C/C at SNP 5, and A/A at SNP 6. The most distant SNP, SNP 7, differed between homozygotes; one patient was heterozygous A/G, and the other two were homozygous G/G at the site. The first six SNPs defined the CACGCA haplotype associated with N88K homozygous patients. This same haplotype could be extracted from alleles identified by minisequencing and restriction enzyme analysis in all other 14 patients and relatives harboring the N88K mutation.
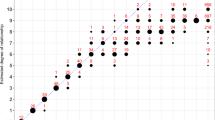
Figure 2 shows the pedigrees of the three families of the N88K homozygous patients. The shaded alleles in each individual indicate the common haplotype. Figure 2 also illustrates a second haplotype (boxed) found in the two asymptomatic mothers. After CACGCA subtraction from the allele pool, both individuals show a CACATG haplotype. This second haplotype was not found in any other individual.
Pedigrees of the three families of homozygous patients. The dark region in the pedigree figures indicates the occurrence of an N88K allele. All N88K heterozygous individuals in all families are asymptomatic. Families 2 and 3 show both the affected patients and their asymptomatic N88K homozygous mothers. The identified alleles are displayed immediately right or left of each individual, with the common haplotype shaded. The two asymptomatic mothers show a second haplotype associated with the N88K mutation, boxed
One hundred alleles from 50 random individuals from the normal population were analyzed using minisequencing and restriction digestion, and the common haplotype CCCGCA was found with SNP 2 being the normal allele at N88. This haplotype was homozygous in 44% and could be deduced from an additional 42% of the sample population. The N88K allele was present in none of the control individuals.
Discussion
In this study, the genotype analysis of patients bearing RAPSN N88K using six intragenic SNP markers demonstrated that three homozygous N88K patients were also homozygotes for an identical SNP haplotype represented by CACGCA. While this result suggests a founder effect, the number of homozygous N88K patients analyzed in this study was small, and since the CACGCA haplotype is relatively common in the normal population, a coincidental association between N88K and the CACGCA haplotype could not be completely excluded. However, since the CACGCA haplotype could also be extracted from the genotype of 14 additional heterozygous carriers of N88K mutation, the findings can be interpreted as either that N88K represents an ancestral mutation (founder) or that N88K arose repetitively in carriers of the CACGCA haplotype.
Previous attempts to investigate a possible founder effect for N88K using extragenic microsatellite markers located in the vicinity of RAPSN have produced mixed results. One group found that only 20% of mutant alleles in ten kinships shared a common haplotype defined by microsatellite markers located near RAPSN (Engel et al. 2003). In contrast, two other groups have reported linkage of N88K with one of the polymorphic microsatellite markers located closest to the gene D11S4117 (Muller et al. 2003; Richard et al. 2003). However, in both studies, the linkage could not be established in all kinships, suggesting that in some families, either the mutation aroused independently or recombination occurred between the mutation and the microsatellite marker.
Taken together, the findings of this study, along with the findings of the studies using microsatellite markers, suggest that RAPSN N88K derives from a common ancestor. Of note is that the families individualized in this and other investigations do not share geographical location, habits, or religion. Furthermore, since only intragenic or extragenic markers located in close proximity to RAPSN showed linkage with the mutation, it appears that N88K represents a very ancient mutation that perpetuated, perhaps as a result of the fact that it is not associated with a severe phenotype.
Surprisingly, we found two N88K homozygotes from two independent families who were not affected. These two individuals, each one the mother of a homozygote CACGCA/N88K patient, carried the C/C A/A C/C A/G T/C A/G genotype, which was different from the C/C A/A C/C G/G C/C A/A genotype found in homozygous N88K patients. Subtraction of the CACGCA haplotype (Clark 1990) from the genotype encountered in these two asymptomatic individuals allowed us to define a second haplotype, CACATG, which was associated with N88K but apparently not with the disease. This finding is particularly interesting in view of the recent report by Burke et al. (2003), which describes a subset of patients with RAPSN mutations with a milder and late-onset phenotype. It would be interesting to see if these patients with a late-onset phenotype carry the CACATG haplotype or another haplotype different from CACGCA. An alternative possibility is that carriers of CACATG may never develop disease. Of note is that one of the carriers of the CACATG haplotype was asymptomatic at the age of 58 years, so it is altogether possible that this individual may never develop symptoms of myasthenia. Still another possibility is that the analysis of a large number of N88K carriers may define several alternative haplotypes associated with the mutation, a finding that may indicate that upon an ancestral mutated allele, multiple haplotypes arose due to intragenic recombination or that in some cases, the mutation indeed occurred independently.
It is unclear why the N88K mutation associated with the CACATG may have a more benign implication than N88K associated with the CACGCA, since CACATG does not change the amino acid sequence of rapsyn. However, the change of the haplotype can be constructed as evidence of an intragenic recombination that may modify transregulatory elements controlling the efficiency of expression of RAPSN or another yet undefined regulatory genetic factor involving other genes. Evidently, more work is needed to elucidate the unique high frequency and high genotype/phenotype variability associated with the RAPSN N88K mutation.
References
Burke G, Cossins J, Maxwell S, Owens G, Vincent A, Robb S, Nicolle M, Hilton-Jones D, Newsom-Davis J, Palace J, Beeson D (2003) Rapsyn mutations in hereditary myasthenia: distinct early- and late-onset phenotypes. Neurology 61(6):826–828
Clark AG (1990) Inference of haplotypes from PCR-amplified samples of diploid populations. Mol Biol Evol 7(2):111–122
Dunne VP, Maselli RA (2003) Identification of pathogenic mutations in the human rapysn gene. J Hum Genet 48:204–207
Engel AG, Ohno K, Sine SM (2003) Sleuthing molecular targets for neurological diseases at the neuromuscular junction. Nat Rev Neurosci 4(5):339–352
Gautam M, Noakes PG, Mudd J, Nichol M, Chu GC, Sanes JR, Merlie JP (1995) Failure of postsynaptic specialization to develop at neuromuscular junctions of rapsyn-deficient mice. Nature 337:232–236
Gautam M, DeChiara TM, Glass DJ, Yancopoulos GD, Sanes JR (1999) Distinct phenotypes of mutant mice lacking agrin, MuSK or rapsyn. Brain Res Dev Brain Res 114:171–178
Maselli RA, Dunne V, Pascual-Pascual SI, Bowe C, Agius M, Frank R, Wollman RL (2003) Rapsyn mutations in myasthenic syndrome due to impaired receptor clustering. Muscle Nerve 28:293–301
Muller JS, Mildner G, Muller-Felber W, Schara U, Krampfl K, Petersen B, Petrova S, Stucka R, Mortier W, Bufler J, Kurlemann G, Huebner A, Merlini L, Lochmuller H, Abicht A (2003) Rapsyn N88K is a frequent cause of congenital myasthenic syndromes in European patients. Neurology 60(11):1805–1810
Ohno K, Engel AG, Shen X-M, Selcen P, Brengman J, Harper CM, Tsujino A, Milone M (2002) Rapsyn mutations in humans cause endplate acetylcholine-receptor deficiency and myasthenic syndrome. Am J Hum Genet 70:875–885
Ohno K, Sadeh M, Blatt I, Brengman JM, Engel AG (2003) E-box mutations in the RAPSN promoter region in eight cases with congenital myasthenic syndrome. Hum Mol Genet 12:739–748
Richard P, Gaudon K, Andreux F, Yasaki E, Prioleau C, Bauche S, Barois A, Ioos C, Mayer M, Routon MC, Mokhtari M, Leroy JP, Fournier E, Hainque B, Koenig J, Fardeau M, Eymard B, Hantai D (2003) Possible founder effect of rapsyn N88K mutation and identification of novel rapsyn mutations in congenital myasthenic syndromes. J Med Genet 40(6):e81
Acknowledgements
We acknowledge the Muscular Dystrophy Association and the Myasthenia Gravis Association of California for financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dunne, V., Maselli, R.A. Common founder effect of rapsyn N88K studied using intragenic markers. J Hum Genet 49, 366–369 (2004). https://doi.org/10.1007/s10038-004-0159-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-004-0159-y
Keywords
This article is cited by
-
Mutation loci and intragenic selection marker of the granule-bound starch synthase gene in waxy maize
Molecular Breeding (2007)