Abstract
Hereditary hemochromatosis (HH) is an autosomal recessive disorder of iron metabolism characterized by increased iron absorption and progressive storage resulting in organ damage. HFE gene mutations C282Y and H63D are responsible for the majority of HH cases. A third HFE mutation, S65C, has been associated with the development of a mild form of hemochromatosis. The beta-thalassemia trait is characterized by mild, ineffective erythropoiesis that can induce excess iron absorption and ultimately lead to iron overload. The aim of this study was to evaluate the effect of genetic markers (HFE mutations C282Y, H63D, and S65C) on the iron status of beta-thalassemia carriers. A total of 101 individuals heterozygous for beta-thalassemia and 101 normal control individuals were studied. The allelic frequencies of C282Y (1.5 versus 3.5%), H63D (15.3 versus 18.3%), and S65C (1.0 versus 1.5%) did not differ significantly between beta-thalassemia carriers and normal controls. Serum iron (P=0.029) and transferrin saturation (P=0.009) were increased in beta-thalassemia carriers heterozygous for H63D mutation. The number of subjects carrying C282Y or S65C mutations was too low to conclude their effect on the iron status. These results suggest that the beta-thalassemia trait tends to be aggravated with the coinheritance of H63D mutation, even when present in heterozygosity.
Similar content being viewed by others
Introduction
Hereditary hemochromatosis (HH) is an autosomal recessive disorder of iron metabolism and represents one of the most common inherited disorders in individuals of northern European descent (Dadone et al. 1982; Edwards et al. 1998). Increased intestinal absorption leads to iron overload in several organs, resulting in various symptoms such as cirrhosis, hepatocellular carcinoma, diabetes, arthritis, and cardiomyopathy (Cartwright et al. 1979). The gene responsible for HH, the HFE gene, encodes an HLA class I-like protein that binds to β2-microglobulin and is found on the cell surface (Feder et al. 1996). Here, HFE protein also complexes with the transferrin receptor (TfR), lowering its affinity for transferrin (Feder et al. 1998). A missense mutation that changes the 282 amino acid from cysteine to tyrosine (C282Y) has been characterized as the main mutation responsible for hemochromatosis (Feder et al. 1996). The C282Y mutation disrupts a critical disulfide bond in the α3 domain of the protein, preventing the HFE molecule from interacting with β2-microglobulin (Feder et al. 1997; Waheed et al. 1997). A second mutation was also described in HH patients (Feder et al. 1996), changing the aspartic acid for histidine at position 63 of the protein (H63D). Although this mutation does not affect the protein cell surface expression, its ability to reduce the HFE-transferrin receptor interaction may explain its relation with iron overload (Waheed et al. 1997). Given that the presence of these mutations does not explain all the phenotypically affected HH individuals, several polymorphisms have been found in the HFE gene in patients that do not carry either of these two mutations or that have at least one chromosome without an assigned mutation (Pointon et al. 2000). Among these, a substitution in exon 2, altering the 65 amino acid serine to cysteine (S65C), has been associated with the development of a mild form of hemochromatosis (Mura et al. 1999; Asberg et al. 2000).
The beta-thalassemia trait, moderately common in the southern Portugal population (Martins et al. 1993), is characterized by mild, ineffective erythropoiesis that can induce excess iron absorption and ultimately lead to iron overload (Weatherall and Clegg 1981). Since only a minority of patients develop iron overload, the hypothesis that genetic modifiers may be related to this phenotypic variability has been set (Fargion et al. 2000; Weatherall 2001). Among these, HFE gene mutations seem to be the most probable cause (Fargion et al. 2000). Moreover, these mutations (C282Y and H63D) are quite frequent in European populations, and H63D mutation allelic frequency reaches its higher values in southern Europe (about 20%) where the beta-thalassemia trait is also common (Weatherall and Clegg 1981; Merryweather-Clarke et al. 2000). The aim of this study was to evaluate the effect of HFE gene mutations C282Y, H63D, and S65C, on the iron status of beta-thalassemia carriers. Additionally, the allelic frequencies of these mutations in the beta-thalassemia carriers were compared to a normal control group.
Materials and methods
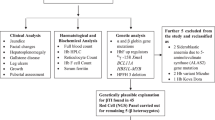
Subjects
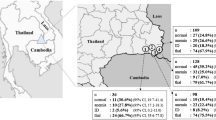
This study was performed on 101 beta-thalassemia carriers (mean age 44.4; SD 17.8) and 101 individuals selected as controls (mean age 41.0; SD 17.2), all unrelated. Due to the geographic heterogeneity of C282Y mutation in Portugal (Cardoso et al. 2001), and being that the beta-thalassemia trait is more frequent in the southern part of the country (Martins et al. 1993), all individuals studied were of southern Portugal origin. Diagnosis of the beta-thalassemia trait was defined by low mean corpuscular volume (MCV <80 fl), low mean corpuscular hemoglobin (MCH <27 pg), and increased HbA2 (>3.5%). Control individuals were characterized by normal hematological parameters. All participants gave informed consent to participate in the study.
Hematological and iron parameters
Hematological data (MCV and MCH) were obtained using a Coulter MAXM, and HbA2 was measured by high-pressure liquid chromatography (Hb-Gold). Serum iron and transferrin levels were measured using a Hitachi 911 analyser and serum ferritin with an Immulite autoanalyzer. Transferrin saturation was calculated, as described elsewhere (Wick et al. 2000).
Molecular analysis
Total genomic DNA was isolated from peripheral blood leukocytes by a salting-out procedure (Miller et al. 1988). The beta-thalassemia genotypes were characterized by amplification refractory mutation system (ARMS) according to the conditions described by Old et al. (1990). This screening was performed to β0Cd39 C→T, β0IVS-I-1 G→A, β+IVS-I-6 T→C and β+IVS-I-110 G→A mutations, as they are the most frequent beta-globin mutations present in southern Portugal (Faustino et al. 1999). In one individual who did not carry any of the former mutations, the beta-globin gene was sequenced using the ABI Prism BigDye Terminator Cycle Sequencing Ready Reaction Kit according to the manufacturer’s instructions. HFE gene mutations (C282Y, H63D, and S65C) were analyzed by a PCR-restriction method, as previously described (Merryweather-Clarke et al. 1997; Mura et al. 1999).
Statistical analysis
Fisher’s exact test was used to compare the allelic frequencies of the HFE gene mutations and the 95% confidence intervals (CI) were calculated by the binomial exact method (Zar 1996). Measurements of iron parameters are expressed by mean and 95% CI. As serum ferritin concentrations distribution approximates a log-normal distribution, geometric means were calculated. Due to the small number of individuals in the other HFE genotype subgroups, comparison of the iron biochemical markers was performed only between the H63D/wild-type and the wild-type/wild-type genotypes. For this purpose, the univariate analysis of variance (ANOVA) was used, including age as a covariate to control for its effect (for serum ferritin, the ANOVA was applied to the log-transformed data). For all statistical tests, the significant level was set at 5%. All statistical analyses were performed using the SPSS version 11.0 software.
Results
Beta-thalassemia genotypes
All beta-thalassemia carriers (except one) revealed heterozygosity for one of the most common beta-globin mutations described in southern Portugal: 50.5% were carriers of the β0Cd39 C→T mutation, 26.7% of the β0IVS-I-1 G→A, 5.0% of the β+IVS-I-6 T→C and 16.8% of the β+IVS-I-110 G→A. These frequencies are similar to those previously described by Faustino et al. (1999). Furthermore, one individual presented heterozygosity for β0Cd6 (-A) mutation, which is a very rare mutation in the southern Portugal.
HFE allelic frequencies and genotypes
The allelic frequencies obtained for HFE gene mutations C282Y, H63D, and S65C in beta-thalassemia carriers and normal controls are presented in Table 1. Fisher’s test did not reveal any statistically significant difference between beta-thalassemia carriers and controls (P>0.05). Nevertheless, all mutations studied had a higher frequency in controls. These frequencies were also compared with those found in a previous study by Cardoso et al. (2001) regarding random controls of southern Portugal origin. Again, no statistically significant difference was found among these three groups.
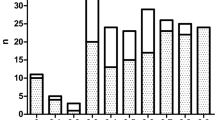
Mutational analysis for the HFE gene (Table 2) showed that, in beta-thalassemia carriers, the genotype wild-type/wild-type was the most frequent, accounting for 67 individuals. Compound heterozygotes C282Y/H63D and H63D/S65C together with C282Y and S65C heterozygotes represent the less-common genotypes with no more than one or two individuals. H63D/wild-type was the most frequent genotype presenting an HFE mutation (n=29 individuals). No individual homozygous for these HFE gene mutations was found.
HFE mutations and iron metabolism
Mean values of biochemical iron markers were analyzed in beta-thalassemia carriers according to their HFE genotype, and all individuals carrying HFE gene mutations were compared to the wild-type/wild-type genotype (Table 2). Serum iron and transferrin saturation presented a generalized increase in the genotypes carrying HFE gene mutations (with the exception of serum iron in C282Y/H63D individual). This increase was statistically significant in the H63D/wild-type (P=0.029 and P=0.009 for serum iron and transferrin saturation, respectively). Regarding serum ferritin, individuals heterozygous for C282Y, H63D, and S65C presented higher values than the wild-type genotype. Although this marker was greatly increased in the C282Y/wild-type group, since only two individuals were found, statistical tests were not performed.
A similar analysis was performed in the normal control group. Although the biochemical iron markers also seem to be increased with the presence of HFE gene mutations, this increase was not statistically significant for the H63D/wild-type genotype (P>0.05), the only group that allowed statistical tests to be performed (n=27) (data not shown).
Discussion
The allelic frequencies found for C282Y and H63D mutations in this study resemble the values obtained by Cardoso et al. (2001) in a southern Portugal population and are in conformity with the distribution pattern found for southern European populations (Merryweather-Clarke et al. 2000). It has been suggested that thalassemia-affected Italians had a lower HFE prevalence than the general Italian population (Fargion et al. 2000). However, we have not found any statistically significant difference for C282Y and H63D frequencies between beta-thalassemia carriers and controls, and our results do not support the previous hypothesis.
Geographic distribution of S65C mutation is relatively unknown, and studies regarding this mutation are generally performed on hemochromatosis patients. However, reports by Mura et al. (1999) and Juan et al. (2001) in French and Spanish individuals, respectively, consider frequency values of 1.9 and 3.0% for this mutation in healthy controls. More recently, in a study performed in the Terceira Island population (Azores), S65C mutation was found with an overall frequency of 2.1% in control individuals (Couto et al. 2003). Similarly, we found an allelic frequency of 1.5% for S65C in the normal control group. Considering genetic heterogeneity in southern European populations where C282Y homozygotes only explain 60–80% of HH phenotypes (Merryweather-Clarke et al. 2000), the presence of S65C, as well as other HFE mutations, should probably be considered when screening for genetic defects in hemochromatosis patients.
This study intended to evaluate the phenotypic expression of HFE genotypes regarding the variation of biochemical iron markers in a group of beta-thalassemia carriers. Some studies have been conducted in order to relate beta-thalassemia and HFE gene mutations, but the results and conclusions obtained seem to vary. A study performed by Rees et al. (1998) where beta-thalassemia intermedia patients were screened for H63D and C282Y mutations, found that the presence of C282Y mutation greatly increased the ferritin levels of one proband. These authors first enhanced the importance of genetic screening for hereditary hemochromatosis in other iron-loading conditions. Similarly, Arruda et al. (2000) and Piperno et al. (2000) associated these two diseases but with the purpose of analyzing the effect of the beta-thalassemia trait in hemochromatosis patients. Both agreed that the beta-thalassemia trait aggravates the clinical picture of C282Y homozygotes. However, Longo et al. (1999) results suggested that the presence of a single mutation in the HFE gene does not influence iron loading in thalassemia-major patients. More recently, Melis et al. (2002) found significantly higher levels of ferritin in beta-thalassemia carriers who were homozygotes for H63D mutation but found no statistical difference in heterozygous H63D individuals.
Our main purpose was to analyze the effect of several HFE genotypes on iron biochemical markers in beta-thalassemia carriers. The results reveal that the presence of H63D mutation aggravates the individuals’ iron status, presenting higher serum iron, transferrin saturation, and serum ferritin compared with the wild-type group. Age was included as a covariate in the ANOVA to assure that the effect of H63D mutation was not being influenced by age. Unfortunately, the number of individuals carrying C282Y and S65C mutations was too small to conclude their effect on iron status. Some discrepancies, such as the lowering of some parameters, can also be explained by the small number of individuals in some HFE genotype groups or by the fact that both male and female individuals were included in this study. Additional studies should consider a larger sample number in order to determine the effect of these or other rare HFE mutations in the development of iron overload in beta-thalassemia carriers.
Our overall results demonstrate that the beta-thalassemia trait, already related with the potential development of iron overload, tends to be aggravated with the coinheritance of H63D mutation, even when present in heterozygosity.
References
Arruda VR, Agostinho MF, Cancado R, Costa FF, Saad ST (2000) Beta-thalassemia trait might increase the severity of hemochromatosis in subjects with the C282Y mutation in the HFE gene. Am J Hematol 63:230–233
Asberg A, Thorstensen K, Hveem K, Bjerve KS (2000) Hereditary hemochromatosis: the clinical significance of the S65C mutation. Genet Test 6:59–62
Cardoso CS, Oliveira P, Porto G, Oberkanins C, Mascarenhas M, Rodrigues P, Kury F, de Sousa M (2001) Comparative study of the two more frequent HFE mutations (C282Y and H63D): significant different allelic frequencies between the North and South of Portugal. Eur J Hum Genet 9:843–848
Cartwright GE, Edwards CQ, Kravitz K, Skolnick M, Amos DB, Johnson A, Buskjaer L (1979) Hereditary hemochromatosis. Phenotypic expression of the disease. N Engl J Med 301:175–179
Couto AR, Peixoto MJ, Garrett F, Laranjeira F, Cipriano T, Armas JB (2003) Linkage disequilibrium between S65C HFE mutation and HLA A29-B44 haplotype in Terceira Island, Azores. Hum Immunol 64:625–628
Dadone MM, Kushner JP, Edwards CQ, Bishop DT, Skolnick MH (1982) Hereditary hemochromatosis. Analysis of laboratory expression of the disease by genotype in 18 pedigrees. Am J Clin Pathol 78:196–207
Edwards CQ, Griffen LM, Goldgar D, Drummond C, Skolnick MH, Kushner JP (1998) Prevalence of hemochromatosis among 11,065 presumably healthy blood donors. N Engl J Med 318:1355–1362
Fargion S, Sampietro M, Cappellini MD (2000) Thalassemias and their interactions with hemochromatosis. In: Barton JC, Edwards CQ (eds) Hemochromatosis. Cambridge University Press, Cambridge, pp 435–441
Faustino P, Pacheco P, Loureiro P, Nogueira PJ, Lavinha J (1999) The geographic pattern of beta-thalassaemia mutations in the Portuguese population. Br J Haematol 107:903–904
Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, Dormishian F, Domingo R Jr, Ellis MC, Fullan A, Hinton LM, Jones NL, Kimmel BE, Kronmal GS, Lauer P, Lee VK, Loeb DB, Mapa FA, McClelland E, Meyer NC, Mintier GA, Moeller N, Moore T, Morikang E, Prass CE, Quintana L, Starnes SM, Schatzman RC, Brunke KJ, Drayna DT, Risch NJ, Bacon BR, Wolff RK (1996) A novel MHC class-I gene is mutated in patients with hereditary hemochromatosis. Nat Genet 13:399–408
Feder JN, Tsuchihashi Z, Irrinki A, Lee VK, Mapa FA, Morikang E, Prass CE, Starnes SM, Wolff RK, Parkkila S, Sly WS, Schatzman RC (1997) The hemochromatosis founder mutation in HLA-H disrupts beta2-microglobulin interaction and cell surface expression. J Biol Chem 272:14025–14028
Feder JN, Penny DM, Irrinki A, Lee VK, Lebron JA, Watson N, Tsuchihashi Z, Sigal E, Bjorkman PJ, Schatzman RC (1998) The hemochromatosis gene product complexes with the transferrin receptor and lowers its affinity for ligand binding. Proc Natl Acad Sci U S A 95:1472–1477
Juan MD, Reta A, Castiella A, Pozueta J, Prada A, Cuadrado E (2001) HFE gene mutations analysis in Basque hereditary haemochromatosis patients and controls. Eur J Hum Genet 9:961–964
Longo F, Zecchina G, Sbaiz L, Fisher R, Piga A, Camashella C (1999) The influence of hemochromatosis mutations on iron overload of thalassemia major. Haematologica 84:799–803
Martins MC, Olim G, Melo J, Magalhaes HA, Rodrigues MO (1993) Hereditary anaemias in Portugal: epidemiology, public health significance, and control. J Med Genet 30:235–239
Melis MA, Cau M, Deidda F, Barella S, Cao A, Galanello R (2002) H63D mutation in the HFE gene increases iron overload in β-thalassemia carriers. Haematologica 87:242–245
Merryweather-Clarke AT, Pointon JJ, Shearman JD, Robson KJ (1997) Global prevalence of putative haemochromatosis mutations. J Med Genet 34:275–278
Merryweather-Clarke AT, Pointon JJ, Jouanolle AM, Rochette J, Robson KJH (2000) Geography of HFE C282Y and H63D mutations. Genet Test 4:183–198
Miller SA, Dykes DD, Polesky HF (1988) A simple salting-out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16:1215
Mura C, Raguenes O, Férec C (1999) HFE mutations analysis in 711 hemochromatosis probands: evidence for S65C implication in mild form of hemochromatosis. Blood 93:2502–2505
Old JM, Varawalla NY, Weatherall DJ (1990) Rapid detection and prenatal diagnosis of beta-thalassaemia: studies in Indian and Cypriot populations in the UK. Lancet 336:834–837
Piperno A, Mariani R, Arosio C, Vergani A, Bosio S, Fargion S (2000) Haemochromatosis in patients with beta-thalassaemia trait. Br J Haematol 111:908–914
Pointon JJ, Wallace D, Merryweather-Clarke AT, Robson KJ (2000) Uncommon mutations and polymorphisms in the hemochromatosis gene. Genet Test 4:151–161
Rees DC, Singh BM, Luo LY, Wickramasinghe S, Thein SL (1998) Nontransfusional iron overload in thalassemia: association with hereditary hemochromatosis. Ann N Y Acad Sci 850:490–494
Waheed A, Parkkila S, Zhou XY, Tomatsu S, Tsuchihashi Z, Feder JN, Schatzman RC, Britton RS, Bacon BR, Sly WS (1997) Hereditary hemochromatosis: effects of C282Y and H63D mutations on association with beta2-microglobulin, intracellular processing, and cell surface expression of the HFE protein in COS-7 cells. Proc Natl Acad Sci U S A 94:12384–12389
Weatherall DJ (2001) Phenotype-genotype relationships in monogenic disease: lessons from the thalassaemias. Nat Rev Genet 2:245–255
Weatherall DJ, Clegg JB (1981) The thalassaemia syndromes, 3rd edn. Blackwell Scientific Publication, Oxford
Wick M, Pinggera W, Lehmann P (2000) Iron metabolism, anemias, diagnosis and therapy, 4th edn. Springer, Berlin Heidelberg New York
Zar JH (1996) Biostatistical analysis, 3rd edn. Prentice Hall International Editions, London
Acknowledgements
This work was partially supported by the Comissão de Fomento da Investigação em Cuidados de Saúde, Ministério da Saúde, Proj 199/2001.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martins, R., Picanço, I., Fonseca, A. et al. The role of HFE mutations on iron metabolism in beta-thalassemia carriers. J Hum Genet 49, 651–655 (2004). https://doi.org/10.1007/s10038-004-0202-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-004-0202-z
Keywords
This article is cited by
-
PIEZO1 gene mutation in a Japanese family with hereditary high phosphatidylcholine hemolytic anemia and hemochromatosis-induced diabetes mellitus
International Journal of Hematology (2016)
-
MR imaging of spleen in beta-thalassemia major
Abdominal Imaging (2015)
-
Bone marrow changes in beta-thalassemia major: quantitative MR imaging findings and correlation with iron stores
European Radiology (2007)
-
MRI evaluation of tissue iron burden in patients with β-thalassaemia major
Pediatric Radiology (2007)