Abstract
A mtDNA A1555G base substitution in a highly conserved region of the 12S rRNA gene has been reported to be the main cause of aminoglycoside induced deafness. This mutation is found in approximately 3% of Japanese and 0.5–2.4% of European sensorineural deafness patients. We report a high prevalence (5.3%) of the A1555G mutation in sensorineural deafness patients in Sulawesi (Indonesia). Our result confirms the importance of determining the prevalence of the mtDNA A1555G mutation in different populations, and the need for mutation detection before the administration of aminoglycoside antibiotics.
Similar content being viewed by others
Introduction
Amongst mutations that underlie sensorineural deafness, an A1555G base substitution in the small (12S) rRNA gene of mtDNA is of particular interest as a main cause of antibiotic-induced deafness (Fischel-Ghodsian, 1999). This mutation increases sensitivity to aminoglycoside ototoxicity, but has been reported also in deaf individuals who have not been exposed to these antibiotics (Fischel-Ghodsian, 1999). It has been detected in sensorineural deafness patients with widely differing ethnic backgrounds (Pandya et al. 1997; Casano et al. 1998; Estivill et al. 1998; Scrimshaw et al. 1999; Kupka et al. 2002; Ostergaard et al. 2002; Tekin et al. 2003), with a prevalence of 0.5–2.4% in European sensorineural deafness patients (Scrimshaw et al. 1999; Kupka et al. 2002; Ostergaard et al. 2002; Tekin et al. 2003).
In Japan, approximately 3% of sensorineural deafness patients and 10% of cochlear implantation patients carry the mtDNA A1555G mutation (Usami et al. 2000), leading to the suggestion that testing for the mutation should be carried out as a routine before the administration of aminoglycoside antibiotics. The A1555G mutation has been reported also in China (Prezant et al. 1993), and recently in a large Balinese family with non-syndromic sensorineural deafness (Malik et al. 2003), raising the possibility that the mutation might also be an important cause of sensorineural deafness in other populations of Asia. We have thus investigated the prevalence of this mutation amongst sensorineural deafness patients in the populations of the island Southeast Asia, focusing in the first instance on that of South Sulawesi in the middle of the large Celebes archipelago.
Patients and Methods
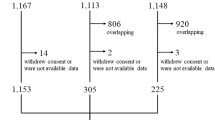
Two groups of sensorineural deafness patients who came to the ENT clinic in the Wahidin Hospital in Makassar, South Sulawesi, were investigated: 75 unrelated non-syndromic sensorineural deafness patients (age 6–43 years; group I), and 50 unrelated patients with diabetes mellitus (DM) and sensorineural deafness (age 40–60 years; group II). In addition, we examined 100 normal healthy unrelated individuals as normal control subjects. All group II patients were confirmed to have Type 2 diabetes following the WHO criteria, and receiving treatment for diabetes mellitus at the hospital. Informed consent to participate in the study was obtained, and the study was approved by the human ethics committee of Hasanuddin University, Makassar (No. 52/KEP/IV/2002).
Sensorineural deafness was diagnosed by audiologic testing with a pure-tone audiometer (Rion Audiometer AA-72B, Tokyo, Japan). The severity of hearing loss was classified according to the better ear: mild (27–40 dB), moderate (41–55 dB), moderate–severe (56–70 dB), severe (71–90 dB) and profound hearing loss (above 90 dB).
The A1555G (and also the A3243G) mutations were detected by PCR-RFLP as previously described (Lertrit et al. 1992; Malik et al. 2003). For sequencing of the hypervariable region 1 (HVR 1) of the mtDNA D-loop, the relevant fragment was PCR amplified using a primer pair, L15904 (5′-CTAATACACCAGTCTTGTAAA CCGGAG-3′) – H504 (5′-ATGGGCGGGGGTTGTATTGATGAG-3′). Purified PCR products were sequenced with L15904, L16204 (5′-GCAAGTACAGCAATCAA CCCTC-3′) and H181 (5′-TAATATTGAACGTAGGTGCG-3′) as sequencing primers (Malik et al. 2002).
Results
Of the 75 patients from group I (non-syndromic sensorineural deafness), two (2.7%) had moderate, two (2.7%) moderate–severe, 18 (24%) severe, and 53 (70.6%) profound hearing loss. In comparison, 40 of the 50 patients with diabetes mellitus and sensorineural deafness (group II; 80%) had mild, five (10%) moderate, and five (10%) moderate–severe hearing loss. All the 100 control individuals were confirmed to have normal hearing. Four (5.3%) of the deafness patients from group I, but none from group II, were found to carry the mtDNA A1555G mutation (Fig. 1). This mutation was not found in the 100 control individuals.
Detection of mtDNA A1555G and A3243G mutations. The A1555G mutation was diagnosed by PCR-RFLP as described by Malik et al. (2003). The PCR amplification of a 551-bp mtDNA fragment was carried out using the primer pair L1231 and H1782. The A1555G base substitution was detected as a loss of a BsmAI restriction site, and confirmed by sequencing using L1231 as the sequencing primer (Malik et al. 2003). Shown on the left panel are RFLP analyses of the PCR-amplified fragments from two sensorineural deafness patients with DM (DM 24 and DM 25), two sensorineural deafness patients showing the mtDNA A1555G mutation (homoplasmic; D12 and D27), and two normal controls (N10 and N12). The A3243G mutation was detected by a similar PCR-RFLP procedure, involving the amplification of a 903-bp fragment of the mtDNA with the primer pair L2826 and H3728, and the detection of the mutation as a gain of an ApaI restriction site (Lertrit et al. 1992)
We have tested at the same time for another mtDNA mutation, A3243G, in the tRNA Leu gene, which has been reported to be associated also with sensorineural deafness in significant prevalence, especially in syndromic cases with DM (Kadowaki et al. 1994; Nagata et al. 2001). However, this mutation was not found in the total of 125 sensorineural deafness patients (groups I and II) examined or in the control group.
We are interested to find out whether the A1555G mutation in the four deafness patients had arisen independently, and have thus sequenced the HVR I of the mtDNA D-loop in these patients. Comparison of the sequencing data revealed that the four deaf patients were not related (Table 1).
Aminoglycosides are broad-spectrum antibiotics, many members of which (such as streptomycin) are still widely used in Asia, because they are relatively inexpensive. Local health authorities confirmed that streptomycin, as well as kanamycin and neomycin, have been widely used in South Sulawesi, but we could not ascertain whether the four mitochondrial sensorineural deafness patients found have been exposed previously to these antibiotics.
Discussion
Our finding has important medical implications. The absence of the mtDNA A3243G mutation in our patients, in particular in those who also had diabetes mellitus, is of significance and consistent with the result of our recent study. Of more than 1,500 Indonesian patients with Type 2 diabetes examined for this mutation, none were found to carry the A3243G mutation (Sudoyo et al. 2003), in contrast to around 0.9–2.8% in Japanese subjects (Kadowaki et al. 1994; Otabe et al. 1994; Kishimoto et al. 1995), 2.5% in Chinese subjects (Ng et al. 2000), and 0.2% in Korean diabetic patients (Lee et al. 1997). The prevalence of this mutation in sensorineural deafness patients in Japan is 1.7% (Nagata et al. 2001), and as high as 50–60% of diabetic patients with sensorineural deafness (Kadowaki et al. 1994; Nagata et al. 2001). Thus, it seems that there is an ethnic-related variation in the prevalence of this mutation, presumably influenced by the overall mitochondrial genetic background.
The relatively high frequency of the A1555G mutation in the Indonesian sensorineural deafness patients indeed suggests that this mutation is an important contributor to sensorineural deafness in this region. The prevalence of the A1555G mutation in group I (non-syndromic sensorineural deafness) was 5.3%. The mutation was not found in the sensorineural deafness patients with diabetes mellitus, the group which has been included in this study for the specific purpose of examining the prevalence of the A3243G mutation. The overall prevalence of the A1555G mutation amongst the sensorineural deafness patients (a total of 125) was 3.2%, but the appropriateness of the diabetic group as part of the analysis of the prevalence of the A1555G mutation amongst the sensorineural deafness patients is uncertain.
The relationship of the phenotypic expression of this mutation and the use of aminoglycoside antibiotics is well established. Between 33% and 59% of sensorineural deafness patients with histories of exposure to aminoglycosides in Japan carry this mutation (Usami et al. 2000). Thus, should a screening for the mitochondrial DNA A1555G mutation be conducted before the administration of aminoglycoside antibiotics? The population prevalence for the A1555G mutation is not known. The average prevalence of deafness in 34 developing nations is estimated to be 1.4 hearing impaired per 1,000 (Mencher 2000). Taking 3–5.3% frequency of the A1555G mutation in Japanese and Indonesian sensorineural deafness patients (Usami et al. 2000 and this study), the population prevalence of the mutation would be around 1 per 13,500 to 1 per 24,000. In phenylketonuria, the clinical outcome of which can be completely ameliorated by early nutritional intervention, newborn screening is recommended on the basis of the incidence of 1 per 13,500–19,000 newborns (NIH Consensus Statement, 2000). By comparison, therefore, the screening for A1555G mutation before the administration of aminoglycosides should be considered.
Indeed in special cases, such a recommendation could be strongly advocated, e.g., when aminoglycosides have to be used for prolonged treatment. A particular example is the use of streptomycin in the treatment of tuberculosis. Despite its ototoxicity, this aminoglycoside antibiotic is still one of the first-line (essential) anti-tuberculosis drugs recommended by WHO (2003). In addition, kanamycin and amikacin are used as reserve (second-line) anti-tuberculosis (WHO, 2003). It is essential that further study is conducted to confirm the importance of this mutation as the cause of sensorineural deafness in Asia and elsewhere.
References
Anderson S, Bankier AT, Barrell BG, de Bruijn MH, Coulson AR, Drouin J, Eperon IC, Nierlich DP, Roe BA, Sanger F, Schreier PH, Smith AJ, Staden R, Young IG (1981) Sequence and organization of the human mitochondrial genome. Nature 290:457–465
Andrews RM, Kubacka I, Chinnery PF, Lightowlers RN, Turnbull DM, Howell N (1999) Reanalysis and revision of the Cambridge reference sequence for human mitochondrial DNA. Nat Genet 23:147
Casano RA, Bykhovskaya Y, Johnson DF, Hamon M, Torricelli F, Bigozzi M, Fischel-Ghodsian N (1998) Hearing loss due to the mitochondrial A1555G mutation in Italian families. Am J Med Genet 79:388–391
Estivill X, Govea N, Barcelo E, Badenas C, Romero E, Moral L, Scozzri R, D'Urbano L, Zeviani M, Torroni A (1998) Familial progressive sensorineural deafness is mainly due to the mtDNA A1555G mutation and is enhanced by treatment of aminoglycosides. Am J Hum Genet 62:27–35
Fischel-Ghodsian N (1999) Mitochondrial deafness mutations reviewed. Hum Mutat 13:261–270
Kadowaki T, Kadowaki H, Mori Y, Tobe K, Sakuta R, Suzuki Y, Tanabe Y, Sakura H, Awata T, Goto Y, Hayakawa T, Matsuoka K, Kawamori R, Takenobu K, Horai S, Nonaka I, Habura R, Akanuma Y, Tazaki Y (1994) A subtype of diabetes mellitus associated with a mutation of mitochondrial DNA. N Engl J Med 330:962–968
Kishimoto M, Hashiramoto M, Araki S, Ishida Y, Kazumi T, Kanda E, Kasuga M (1995) Diabetes mellitus carrying a mutation in the mitochondrial tRNA(Leu(UUR)) gene. Diabetologia 38:193–200
Kupka S, Toth T, Wrobel M, Zeissler U, Szyfter W, Szyfter K, Niedzielska G, Bal J, Zenner HP, Sziklai I, Blin N, Pfister M (2002) Mutation A1555G in the 12S rRNA gene and its epidemiological importance in German, Hungarian, and Polish patients. Hum Mutat 19:308–309
Lee HC, Song YD, Li HR, Park JO, Suh HC, Lee E, Lim S, Kim K, Huh K (1997) Mitochondrial gene transfer ribonucleic acid (tRNA)Leu(UUR) 3243 and tRNALys 8344 mutations and diabetes mellitus in Korea. J Clin Endocrinol Metab 82:372–374
Lertrit P, Noer AS, Jean-Francois MJ, Kapsa R, Dennett X, Thyagarajan D, Lethlean K, Byrne E, Marzuki S (1992) A new disease-related mutation for mitochondrial encephalopathy lactic acidosis and stroke-like episodes (MELAS) syndrome affects the ND4 subunit of the respiratory complex I. Am J Hum Genet 51:457–68
Malik S, Sudoyo H, Sasmono T, Winata S, Arhya IN, Pramoonjago P, Sudana W, Marzuki S (2003) Non-syndromic sensorineural deafness in a Balinese family associated with the A1555G mutation in the mitochondrial small subunit ribosomal RNA. J Hum Genet 48:119–124
Malik S, Sudoyo H, Pramoonjago P, Suryadi H, Sukarna T, Njunting M, Sahiratmadja E, Marzuki S (2002) Nuclear mitochondrial interplay in the modulation of the homopolymeric tract length heteroplasmy in the control (D-loop) region of the mitochondrial DNA. Hum Genet 110:402–411
Mencher GT (2000) Challenge of epidemiological research in the developing world: overview. Audiology 39:178–183
Nagata H, Kumahara K, Tomemori T, Arimoto Y, Isoyama K, Yoshida K, Konno A (2001) Frequency and clinical features of patients with sensorineural hearing loss associated with the A3243G mutation of the mitochondrial DNA in otorhinolaryngic clinics. J Hum Genet 46:595–599
Ng MC, Yeung VT, Chow CC, Li JK, Smith PR, Mijovic CH, Critchley JA, Barnett AH, Cockram CS, Chan JC (2000) Mitochondrial DNA A3243G mutation in patients with early- or late-onset type 2 diabetes mellitus in Hong Kong Chinese. Clin Endocrinol 52:557–564
Ostergaard E, Montserrat-Sentis B, Gronskov K, Brondum-Nielsen K (2002) The A1555G mtDNA mutation in Danish hearing-impaired patients: frequency and clinical signs. Clin Genet 62:303–305
Otabe S, Sakura H, Shimokawa K, Mori Y, Kadowaki H, Yasuda K, Nonaka K, Hagura R, Akanuma Y, Yazaki Y, Kadowaki T (1994) The high prevalence of the diabetic patients with a mutation in the mitochondrial gene in Japan. J Clin Endocrinol Metab 79(3):768–771
Pandya A, Xia X, Radnaabazar J, Batsuuri J, Dangaansuren B, Fischel-Ghodsian N, Nance WE (1997) Mutation in the mitochondrial 12S rRNA gene in two families from Mongolia with matrilineal aminoglycoside ototoxicity. J Med Genet 34:169–172
Phenylketonuria: Screening and management. (2000) NIH Consensus Statement Online 17:1–27
Prezant TR, Agapian JV, Bohlman MC, Bu X, Oztas S, Qiu W, Arnos KS, Cortopassi GA, Jaber L, Rotter JI, Shohat M. Fischel-Ghodsian N (1993) Mitochondrial ribosomal RNA mutation associated with both antibiotic-induced and non-syndromic deafness. Nat Genet 4:289–294
Scrimshaw BJ, Faed JM, Tate WP, Yun K (1999) Rapid identification of an A1555G mutation in human mitochondrial DNA implicated in aminoglycoside-induced ototoxicity. J Hum Genet 44:388–390
Sudoyo H, Suryadi H, Sitorus N, Tresnasari K, Safari D, Soegondo D and Pranoto A (2003) Mitochondrial genome and susceptibility to diabetes mellitus. Adv Exp Med Biol 531:19–36
Tekin M, Duman T, Bogoclu G, Incesulu A, Comak E, Fitoz S, Yilmaz E, Ilhan I, Akar N (2003) Frequency of mtDNA A1555G and A7445G mutations among children with prelingual deafness in Turkey. Eur J Pediatr 162:154–158
Treatment of Tuberculosis: guidelines for national programmes. (2003) Third edition. World Health Organization, Geneva. p 87–104.
Usami S, Abe S, Akita J, Namba A, Shinkawa H, Ishii M, Iwasaki S, Hoshino T, Ito J, Doi K, Kubo T, Nakagawa T, Komiyama S, Tono T, Komune S (2000) Prevalence of mitochondrial gene mutations among hearing impaired patients. J Med Genet 37:38–40
Acknowledgements
We thank all the patients that have participated in the present study. The Eijkman Institute is supported by a development grant from the Ministry of Research and Technology of the Republic of Indonesia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malik, S.G., Pieter, N., Sudoyo, H. et al. Prevalence of the mitochondrial DNA A1555G mutation in sensorineural deafness patients in island Southeast Asia. J Hum Genet 48, 480–483 (2003). https://doi.org/10.1007/s10038-003-0056-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-003-0056-9
Keywords
This article is cited by
-
Prevalence of the mitochondrial 1555 A>G and 1494 C>T mutations in a community-dwelling population in Japan
Human Genome Variation (2020)
-
Mutations in the two ribosomal RNA genes in mitochondrial DNA among Finnish children with hearing impairment
BMC Medical Genetics (2015)
-
Developing regional genetic counseling for southern Chinese with nonsyndromic hearing impairment: a unique mutational spectrum
Journal of Translational Medicine (2014)
-
Genetic mutations in nonsyndromic deafness patients of Chinese minority and han ethnicities in Yunnan, China
Journal of Translational Medicine (2013)
-
Frequency and spectrum of mitochondrial 12S rRNA variants in 440 Han Chinese hearing impaired pediatric subjects from two otology clinics
Journal of Translational Medicine (2011)