Abstract
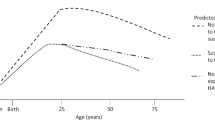
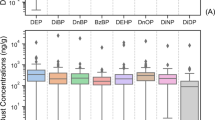
Few studies have examined the relationship between ambient polycyclic aromatic hydrocarbons (PAHs) and pulmonary function in children. Major sources include vehicular emissions, home heating, wildland fires, agricultural burning, and power plants. PAHs are an important component of fine particulate matter that has been linked to respiratory health. This cross-sectional study examines the relationship between estimated individual exposures to the sum of PAHs with 4, 5, or 6 rings (PAH456) and pulmonary function tests (forced expiratory volume in one second (FEV1) and forced expiratory flow between 25% and 75% of vital capacity) in asthmatic and non-asthmatic children. We applied land-use regression to estimate individual exposures to ambient PAHs for averaging periods ranging from 1 week to 1 year. We used linear regression to estimate the relationship between exposure to PAH456 with pre- and postbronchodilator pulmonary function tests in children in Fresno, California (N=297). Among non-asthmatics, there was a statistically significant association between PAH456 during the previous 3 months, 6 months, and 1 year and postbronchodilator FEV1. The magnitude of the association increased with the length of the averaging period ranging from 60 to 110 ml decrease in FEV1 for each 1 ng/m3 increase in PAH456. There were no associations with PAH456 observed among asthmatic children. We identified an association between annual PAHs and chronic pulmonary function in children without asthma. Additional studies are needed to further explore the association between exposure to PAHs and pulmonary function, especially with regard to differential effects between asthmatic and non-asthmatic children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Abbreviations
- ATS:
-
American Thoracic Society
- CHAPS:
-
Children’s Health and Air Pollution Study
- CI:
-
confidence interval
- FACES:
-
Fresno Asthmatic Children’s Environment Study
- FEF25–75:
-
forced expiratory flow between 25% and 75% of vital capacity
- FEV1:
-
forced expiratory volume in one second
- PAH456:
-
PAHs with 4, 5, or 6 rings
- PAHs:
-
polycyclic aromatic hydrocarbons
- PM:
-
particulate matter
References
Gauderman WJ, Avol E, Gilliland F, Vora H, Thomas D, Berhane K et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med 2004; 351 (11): 1057–1067.
Rojas-Martinez R, Perez-Padilla R, Olaiz-Fernandez G, Mendoza-Alvarado L, Moreno-Macias H, Fortoul T et al. Lung function growth in children with long-term exposure to air pollutants in Mexico City. Am J Respir Crit Care Med 2007; 176 (4): 377–384.
Schultz ES, Gruzieva O, Bellander T, Bottai M, Hallberg J, Kull I et al. Traffic-related air pollution and lung function in children at 8 years of age: a birth cohort study. Am J Respir Crit Care Med 2012; 186 (12): 1286–1291.
Gruzieva O, Bergstrom A, Hulchiy O, Kull I, Lind T, Melen E et al. Exposure to air pollution from traffic and childhood asthma until 12 years of age. Epidemiology 2013; 24 (1): 54–61.
Gauderman WJ, Vora H, McConnell R, Berhane K, Gilliland F, Thomas D et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet 2007; 369 (9561): 571–577.
Kim JJ, Huen K, Adams S, Smorodinsky S, Hoats A, Malig B et al. Residential traffic and children's respiratory health. Environ Health Perspect 2008; 116 (9): 1274–1279.
Sram RJ, Benes I, Binkova B, Dejmek J, Horstman D, Kotesovec F et al. Teplice program – the impact of air pollution on human health. Environ Health Perspect 1996; 104 (Suppl 4): 699–714.
Holgate ST . Air Pollution and Health. Academic Press: San Diego, CA, USA. 1999.
Pope CA, 3rd . Respiratory disease associated with community air pollution and a steel mill, Utah Valley. Am J Public Health 1989; 79 (5): 623–628.
Jeng HA, Pan CH, Diawara N, Chang-Chien GP, Lin WY, Huang CT et al. Polycyclic aromatic hydrocarbon-induced oxidative stress and lipid peroxidation in relation to immunological alteration. Occup Environ Med 2011; 68 (9): 653–658.
Miller RL, Garfinkel R, Horton M, Camann D, Perera FP, Whyatt RM et al. Polycyclic aromatic hydrocarbons, environmental tobacco smoke, and respiratory symptoms in an inner-city birth cohort. Chest 2004; 126 (4): 1071–1078.
Gale SL, Noth EM, Mann J, Balmes J, Hammond SK, Tager IB . Polycyclic aromatic hydrocarbon exposure and wheeze in a cohort of children with asthma in Fresno, CA. J Expo Sci Environ Epidemiol 2012; 22 (4): 386–392.
Liu J, Zhang L, Winterroth LC, Garcia M, Weiman S, Wong JW et al. Epigenetically mediated pathogenic effects of phenanthrene on regulatory T cells. J Toxicol 2013; 2013: 967029.
Nadeau K, McDonald-Hyman C, Noth EM, Pratt B, Hammond SK, Balmes J et al. Ambient air pollution impairs regulatory T-cell function in asthma. J Allergy Clin Immunol 2010; 126 (4): 845–52 e10.
Jedrychowski W, Galas A, Pac A, Flak E, Camman D, Rauh V et al. Prenatal ambient air exposure to polycyclic aromatic hydrocarbons and the occurrence of respiratory symptoms over the first year of life. Eur J Epidemiol 2005; 20 (9): 775–782.
Hertz-Picciotto I, Baker RJ, Yap PS, Dostal M, Joad JP, Lipsett M et al. Early childhood lower respiratory illness and air pollution. Environ Health Perspect 2007; 115 (10): 1510–1518.
Perera FP, Rauh V, Whyatt RM, Tsai WY, Tang D, Diaz D et al. Effect of prenatal exposure to airborne polycyclic aromatic hydrocarbons on neurodevelopment in the first 3 years of life among inner-city children. Environ Health Perspect 2006; 114 (8): 1287–1292.
Perera FP, Li Z, Whyatt R, Hoepner L, Wang S, Camann D et al. Prenatal airborne polycyclic aromatic hydrocarbon exposure and child IQ at age 5 years. Pediatrics 2009; 124 (2): e195–e202.
Jedrychowski W, Perera FP, Whyatt R, Mroz E, Flak E, Jacek R et al. Wheezing and lung function measured in subjects exposed to various levels of fine particulates and polycyclic aromatic hydrocarbons. Central Eur J Med 2007; 2 (1): 66–78.
Wilson JG, Kingham S, Sturman AP . Intraurban variations of PM10 air pollution in Christchurch, New Zealand: implications for epidemiological studies. Sci Total Environ 2006; 367 (2-3): 559–572.
Kelly FJ, Fussell JC . Air pollution and airway disease. Clin Exp Allergy 2011; 41 (8): 1059–1071.
Levy JI, Houseman EA, Spengler JD, Loh P, Ryan L . Fine particulate matter and polycyclic aromatic hydrocarbon concentration patterns in Roxbury, Massachusetts: a community-based GIS analysis. Environ Health Perspect 2001; 109 (4): 341–347.
Noth EM, Hammond K, Biging GS, Tager IB . A spatial–temporal regression model to predict daily outdoor residential PAH concentrations in an epidemiologic study in Fresno, CA. Atmos Environ 2011; 45: 2394–2403.
Noth EM, Hammond SK, Biging GS, Tager IB . Mapping and modeling airborne urban phenanthrene distribution using vegetation biomonitoring. Atmos Environ 2013; 77: 518–524.
Briggs DJ, de Hoogh C, Gulliver J, Wills J, Elliott P, Kingham S et al. A regression-based method for mapping traffic-related air pollution: application and testing in four contrasting urban environments. Sci Total Environ 2000; 253 (1–3): 151–167.
Balmes JR, Earnest G, Katz PP, Yelin EH, Eisner MD, Chen H et al. Exposure to traffic: lung function and health status in adults with asthma. J Allergy Clin Immunol 2009; 123 (3): 626–631.
Tager I . Final Report on FACES. University of California: Berkeley, CA, USA. 2006.
Umbach KW . San Joaquin Valley: Land, People, and Economy. California Research Bureau: Sacramento, CA, USA. 2005 Contract No.: No. CRB 05-007.
Kohlmeier JE, Woodland DL . Memory T cell recruitment to the lung airways. Curr Opin Immunol 2006; 18 (3): 357–362.
Margolis HG, Mann JK, Lurmann FW, Mortimer KM, Balmes JR, Hammond SK et al. Altered pulmonary function in children with asthma associated with highway traffic near residence. Int J Environ Health Res 2009; 19 (2): 139–155.
District SJVAPUC 2012 PM2.5 Plan. San Joaquin Valley Air Pollution Unified Control District: Fresno, CA, 20 December 2012.
Marr LC, Kirchstetter TW, Harley RA, Miguel AH, Hering SV, Hammond SK . Characterization of polycyclic aromatic hydrocarbons in motor vehicle fuels and exhaust emissions. Environ Sci Technol 1999; 33 (18): 3091–3099.
Gorin CA, Collett JL, Jr, Herckes P . Wood smoke contribution to winter aerosol in Fresno, CA. J Air Waste Manage Assoc 2006; 56 (11): 1584–1590.
Chen LW, Watson JG, Chow JC, Magliano KL . Quantifying PM2.5 source contributions for the San Joaquin Valley with multivariate receptor models. Environ Sci Technol 2007; 41 (8): 2818–2826.
Chow JC, Watson JG, Lowenthal DH, Chen LWA, Zielinska B, Mazzoleni LR et al. Evaluation of organic markers for chemical mass balance source apportionment at the Fresno Supersite. Atmos Chem Phys 2007; 7 (7): 1741–1754.
Schauer JJ, Cass GR . Source apportionment of wintertime gas-phase and particle-phase air pollutants using organic compounds as tracers. Environ Sci Technol 2000; 34: 1821–1832.
Survey CHI Fresno County Asthma Profile: California Breathing; Available at http://www.californiabreathing.org/asthma-data/county-asthma-profiles/fresno-county-asthma-profile last. accessed 1 July 2013).
Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995; 152 (3): 1107–1136.
Mortimer KM, Fallot A, Balmes JR, Tager IB . Evaluating the use of a portable spirometer a study of pediatric asthma. Chest 2003; 123: 1899–1907.
Hankinson JL, Odencrantz JR, Fedan KB . Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 1999; 159 (1): 179–187.
Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J et al. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect 2003; 111 (4): 455–460.
Salam MT, Lin PC, Avol EL, Gauderman WJ, Gilliland FD . Microsomal epoxide hydrolase, glutathione S-transferase P1, traffic and childhood asthma. Thorax 2007; 62 (12): 1050–1057.
Baccarelli A, Wright RO, Bollati V, Tarantini L, Litonjua AA, Suh HH et al. Rapid DNA methylation changes after exposure to traffic particles. Am J Respir Crit Care Med 2009; 179 (7): 572–578.
Tsien A, Diaz-Sanchez D, Ma J, Saxon A . The organic component of diesel exhaust particles and phenanthrene, a major polyaromatic hydrocarbon constituent, enhances IgE production by IgE-secreting EBV-transformed human B cells in vitro. Toxicol Appl Pharmacol 1997; 142 (2): 256–263.
Hew K, Walker A, Kohli A, Syed A, McDonald-Hyman C, Li ZJ et al. Childhood exposure to polycyclic aromatic hydrocarbons is associated with impaired systemic immunity and epigenetic modifications in T cell subsets. Clin Exp Allergy, (in press).
Balmes JR . How does diesel exhaust impact asthma? Thorax 2011; 66 (1): 4–6.
Acknowledgements
We thank colleagues at Sonoma Technology for the exposure assessment. This work was supported by NIH (K99ES021470, P01ES022849, P20 ES018173, R01 HL081521, R01ES020926), the McCormick Fund at Stanford, the American Academy of Allergy, Asthma, and Immunology Junior Faculty Fund, the Westly Foundation, the Global Health Research Foundation, CDC cooperative agreement 5U19EH000097-04, the California Air Resources Board (contract nos. 99-322, 99-323, and 01-346), the US EPA (PO no. 2A-0540-NASX), the Austin Memorial Fund, and the Mickey Leland National Urban Air Toxics Research Center (RFA 2005-01). This publication was made possible by US EPA STAR Grants RD83459601 and RD83543501. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the US EPA. Further, the US EPA does not endorse the purchase of any commercial products or services mentioned in the publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Padula, A., Balmes, J., Eisen, E. et al. Ambient polycyclic aromatic hydrocarbons and pulmonary function in children. J Expo Sci Environ Epidemiol 25, 295–302 (2015). https://doi.org/10.1038/jes.2014.42
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2014.42
Keywords
This article is cited by
-
An overview of the impacts of coal mining and processing on soil: assessment, monitoring, and challenges in the Czech Republic
Environmental Geochemistry and Health (2023)
-
Association of human cohorts exposed to blood and urinary biomarkers of PAHs with adult asthma in a South Asian metropolitan city
Environmental Science and Pollution Research (2022)
-
Oxidative damage mediates the association between polycyclic aromatic hydrocarbon exposure and lung function
Environmental Health (2020)
-
Potential role of polycyclic aromatic hydrocarbons in air pollution-induced non-malignant respiratory diseases
Respiratory Research (2020)
-
The impact of calcium peroxide on groundwater bacterial diversity during naphthalene removal by permeable reactive barrier (PRB)
Environmental Science and Pollution Research (2019)