Abstract
Enterobacter cloacae is a Gram-negative bacterium associated with high morbidity and mortality in intensive care patients due to its resistance to multiple antibiotics. Currently, therapy against multi-resistant bacteria consists of using colistin, in spite of its toxic effects at higher concentrations. In this context, colistin-resistant E. cloacae strains were challenged with lower levels of colistin combined with other antibiotics to reduce colistin-associated side effects. Colistin-resistant E. cloacae (ATCC 49141) strains were generated by serial propagation in subinhibitory colistin concentrations. After this, three colistin-resistant and three nonresistant replicates were isolated. The identity of all the strains was confirmed by MALDI-TOF MS, VITEK 2 and MicroScan analysis. Furthermore, cross-resistance to other antibiotics was checked by disk diffusion and automated systems. The synergistic effects of the combined use of colistin and chloramphenicol were observed via the broth microdilution checkerboard method. First, data here reported showed that all strains presented intrinsic resistance to penicillin, cephalosporin (except fourth generation), monobactam, and some associations of penicillin and β-lactamase inhibitors. Moreover, a chloramphenicol and colistin combination was capable of inhibiting the induced colistin-resistant strains as well as two colistin-resistant clinical strains. Furthermore, no cytotoxic effect was observed by using such concentrations. In summary, the data reported here showed for the first time the possible therapeutic use of colistin–chloramphenicol for infections caused by colistin-resistant E. cloacae.
Similar content being viewed by others
Introduction
E. cloacae is an important nosocomial pathogen that causes a wide variety of diseases including infections in the respiratory and urinary tracts, the skin, cardiac and soft tissues, the intra-abdominal organs and the eyes.1 This situation has been aggravated as E. cloacae possesses the ability to develop resistance to most carbapenems,2, 3 aztreonam,4 quinolones1, 5 and sulfonamides,6 thus producing an urgent need for novel therapeutic drug development.
However, it is important to emphasize that 10 antibiotics are in clinical trial phases II or III, and they may be suitable for Gram-positive bacterial infection treatment; additionally, five can be used against Gram-negative bacteria.7 This panorama along with the emergence of multi-resistant Gram-negative bacteria such as Acinetobacter baumannii, which causes meningitis, and Pseudomonas aeruginosa, which promotes the exacerbations of cystic fibrosis (CF), have prompted the reintroduction of colistin to the market.8 This antimicrobial is a cationic polypeptide, composed of a cyclic decapeptide linked by an α-amide linkage to a fatty acyl chain.9 Moreover, colistin shows anti-endotoxin activity due to its ability to decrease the exacerbated immunological response that can cause septic shock.10, 11, 12
However, despite the fact that colistin has clinical use against a broad spectrum of Gram-negative bacteria, including Escherichia coli,Klebsiella spp., Acinetobacter spp., Enterobacter spp. and P. aeruginosa,13 it must be cautiously administered because nephrotoxicity is reported among 14–24% of patients in intensive care units. As the development of new antibiotics for use against Gram-negative bacteria has been limited, strategies involving a combination of antibiotics have been employed to obtain synergy by reducing the necessity for higher bactericidal doses while limiting side effects.14
In general, the use of colistin in combination with other antibiotics presents several diverse advantages, including the reduction of toxic effects in mammalian and epithelial cells,15 considering that the therapeutic dose is reduced (2–5 × ). Further, there can be an alteration in pharmacokinetic characteristics, which might increase absorption of others drugs during inhalation therapy,16 and finally the use of a combination reduces the emergence of drug-resistant organisms.17 There is evidence in other studies that the use of a combination of antibiotics with different mechanisms of action could force bacteria to undergo multiple mutations to become resistant, thus slowing the emergence of resistant strains considerably.18
In this context, an E. cloacae strain (ATCC 49141) was cultivated with colistin to select for colistin-resistant E. cloacae strains. To provide a novel treatment against colistin-resistant strains with low cytotoxic effects on mammal cells, the use of colistin combined with other antibiotics showing different mechanisms of action was evaluated. Among the antibiotics were drugs that interfere with cell wall synthesis, as well as in DNA, RNA and protein synthesis.
Materials and methods
Bacterial strains
E. cloacae (ATCC 49141) KwikStik (639P) MBL (Plast Labor, Inhauma, Rio de Janeiro, Brazil) was used as the bacterial model strain. A single colony of E. cloacae was isolated by the streak method in Luria-Bertani (LB) solid medium and propagated in LB broth at 37 °C, and the cell suspension was stored in sterile 10% glycerol at −80 °C. All of the ensuing experiments were carried out from this original stock. The bacterial cells’ growth rate from the original culture was established by measuring the OD at 595 nm, which was monitored at 30 min intervals in LB broth at a constant temperature (37 °C) and with shaking (240 r.p.m.). The direct relationship between OD and CFU was established based on the drop surface plate method,19 and a standard growth curve was constructed and calibrated. In addition, two other clinical strains were used in synergism analyses. One strain (1437710) had its resistance checked by polymerase chain reaction, showing the Klebsiella pneumoniae carbapenemase resistance mechanism. Moreover, another strain (1383251) showed high colistin (CST) resistance levels. Both strains were collected from the blood of the patients from hospitals in Brasília, Brazil. These strains were characterized and provided by the Central Laboratory of Public Health (LACEN-DF), a public diagnostic laboratory in the Federal District of Brazil.
Evaluation of antimicrobial susceptibility via microdilution
The minimum inhibitory concentrations (MICs) of CST and colistin sodium methanesulfonate (CSM) (Sigma-Aldrich, Milwaukee, WI, USA) were tested in LB broth in a 96-well polypropylene microplate by microdilution assay according to the Clinical and Laboratory Standards Institute (CLSI) M07-A8 guideline.20 Milli-Q water was used as a negative control. The plates were incubated at 37 °C at 40 r.p.m. for 16 h, and the OD600 was measured at 30-min intervals using a microplate reader (BioTek, Winooski, VT, USA) for bacterial growth. After incubation, the absence of viable cells in non-turbid wells was confirmed by the culture in LB agar.
Preparation of antibiotic-resistant E. cloacae
The subinhibitory concentration of colistin sulfate salt and CSM (Sigma-Aldrich) used for the preparation of E. cloacae-resistant strains was half the value of the determined colistin MIC for the E. cloacae wild-type strain (designated 0.5 × MIC), as reported in the study by Peng et al.21 During each propagation, four generations were obtained, and the generation time was 20 min, resulting in 40 generations after 10 propagations. In parallel, E. cloacae was cultivated at the same generation number in the absence of colistin and used as a negative control strain. The bacterial suspensions of the last propagations were spread on a colistin-free LB agar plate and cultured overnight at 37 °C. Three colistin-susceptible colonies were selected and isolated by the streak plate method in LB agar at 37 °C. The presence or absence of colistin resistance was evaluated by the broth microdilution assay previously described, and all isolated colonies were challenged with the full colistin MIC (4 μg ml−1). In addition, all colonies were also individually plated in LB agar and supplemented with the full colistin MIC and cultured overnight at 37 °C. When present, a single colony was selected and isolated by the streak plate method in LB agar at 37 °C. Colistin-resistant colonies were named R1, R2 and R3, whereas the control colistin-susceptible colonies were named NR1, NR2 and NR3. Bacterial suspensions were stored in sterile 10% glycerol at −80 °C.
MALDI-TOF MS strain identification
E. cloacae ATCC 49141, E. cloacae CST-susceptible (NR1, NR2 and NR3) and E. cloacae CST-resistant (R1, R2 and R3) strains were subcultured for 12 h in solid LB medium. Six colonies of each strain were transferred to a vial containing 1 ml of 70% ethanol, and further extracted with acetonitrile and 70% formic acid in a 1:1 ratio (v/v), as reported in the study by Calderaro.22 The sample was centrifuged again at 13 000 g for 2 min, and 1 μl of the supernatant was applied to a MALDI plate (Bruker Daltonics, Berlin, Germany) and air-dried at room temperature. Subsequently, a further 1 μl aliquot of a saturated matrix solution of α-cyano-4-hydroxycinnamic acid in 50% acetonitrile and 0.3% trifluoroacetic acid was then added to the spot. Samples were analyzed on a MicroFlex LT mass spectrometer (Bruker Daltonics) in positive linear mode using the MALDI Biotyper (MBT) method. Over 24 spectra of each strain were acquired over the m/z range of 2000–20 000 Da for protein profile generation.
Bruker MALDI Biotyper spectral analysis
Spectra were smoothed, and the baseline was corrected and compared against the MALDI Biotyper database version 3.0 (Bruker Daltonik GmbH), containing 3995 reference microorganisms at the time of comparison. The standard parameters of the pattern-matching algorithm were applied. The MALDI Biotyper output consists of a log (score) in the range 0–3.0, computed by comparing the peak list for an unknown strain with the reference. A log (score) >2.0 is indicative of good correlation within species level. According to Mellmann et al.,23 a score value distance of at least 0.15 between the two best-scored species is defined as necessary for precise species identification.
Main spectrum dendrogram
In addition to identifying all E. cloacae strains by MALDI-TOF MS, a main spectrum of each E. cloacae strain was built upon the combination of 24 individually acquired mass spectra. For the main spectrum creation and construction of dendrogram, all processing steps were automatically performed using the default settings of the FlexControl software (Bruker Daltonics). The main spectrum of each E. cloacae strain that was resistant and susceptible to CST was compared with the original ATCC strain and then assigned to a specific cluster on the cluster analysis tree.
Strain identification and susceptibility assay by automated systems
The stock culture strains E. cloacae (ATCC 49141, NR1, NR2, NR3 controls and R1-, R2-, R3-resistant strains) were subcultured twice on LB agar plates and then grown on MacConkey agar plates at 37 °C for 16 h. Next, all the procedures were carried out according to the manufacturer’s directions. For bacterial identification, the VITEK 2 system (BioMérieux, Lyon, Auvergne-Rhône-Alpes, France) utilized the ID-GNBcard for Gram-negative identification and the AST-N105 for antimicrobial susceptibility testing. The MicroScan WalkAway system (Siemens Healthcare Diagnostics Greenburgh, New York, NY, USA) was used with the MC50 test panel for identification and resistance detection. In relation to the clinical strains, the identification and antibiotic resistance phenotypes were analyzed by the MicroScan WalkAway system (Siemens) using an MC 42 test panel. Values outside these ranges were classified as low discrimination or unidentified organism. Regarding the AST, both automated systems calculated the MIC for each antimicrobial drug tested after incubation. The interpretative breakpoints for MIC obtained from automated systems were analyzed according to the interpretative criteria of CLSI M100-S23,24 and the strain was classified as susceptible (S), intermediate (I) and resistant (R), according to each antibiotic tested.
Evaluation of antimicrobial susceptibility by disk diffusion
All E. cloacae strains were evaluated by a disk diffusion test. For these analyses, distinct classes of antimicrobial disks (Newprov, Pinhais, Paraná, Brazil) were selected, including β-lactam classes such as penicillin (ampicillin (10 μg) and oxacillin (1 μg)), cephalosporins (cefepime (30 μg), cephalothin (30 μg), ceftazidime (30 μg) and cefotaxime (30)), carbapenems (10 μg) and meropenem (10 μg), monobactam (aztreonam (30 μg), and β-Lactam–β-Lactamase Inhibitor Combinations (amoxicillin–clavulanic acid (30 μg), piperacillin–tazobactam (100/10) and ampicillin–sulbactam (10/10)). In addition, antibiotics that inhibit protein synthesis were also available, such as chloramphenicol (CHL; 30 μg), tetracycline (30 μg), aminoglycosides (gentamicin (10 μg) and amikacin (30 μg)) and macrolide classes such as erythromycin (15 μg). Furthermore, one quinolone (ciprofloxacin (5 μg) and one antimicrobial peptide (polymyxin E (300 UI) were also tested. For these analyses, E. cloacae ATCC 49141 was cultured in Mueller–Hinton agar plates, and then different antibiotics were applied to the disk content and further incubated at 37 °C for 18 h. After incubation, each plate was examined and the inhibition zone was measured to the nearest whole millimeter. The zone diameter breakpoints were interpreted according to Table 1a in CLSI document M100-S23.24
Synergy evaluation by checkerboard assay
Colistin (CST and CSM) activities in combination with other antibiotics, such as vancomycin hydrochloride, erythromycin hydrate, ampicillin and CHL (all from Sigma-Aldrich) were used for the synergism assay against colistin-resistant strains. Stock solutions of all antibiotics (1000 μg ml−1) were prepared in sterile distilled water. Plates were set up with increasing concentrations of colistin (0–256 μg ml−1) in the horizontal wells; and other antibiotics, including vancomycin/erythromycin/ampicillin/CHL, all at concentrations of 0–256 μg ml−1 were put in the vertical wells and inoculated with 105 CFU ml−1 of E. cloacae R3 prepared in LB broth. In addition, similar analyses were performed using two clinically isolated strains, characterized and supplied by a public diagnosis laboratory (LACEN-DF of the Federal District, Brazil). After incubation for 16 h at 37 °C, the absence of viable cells in non-turbid wells was confirmed by plating the culture in LB agar. Checkerboard results were interpreted by calculating the FICIs.25 FICIs were calculated as follows: (MIC of CST in combination with other antibiotics/MIC of CST alone)+(MIC of other antibiotics in combination with CST/MIC of other antibiotics alone). The FIC index was interpreted as follows: synergy (FICI<0.5), indifference (0.5<FICI< 4) and antagonism (FICI>4).
Cell cytotoxicity assay
Cytotoxicity was measured for RAW 264.7 murine macrophage-like cells and Vero cells (monkey kidney origin) by (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) (MTT) assay. Cells were seeded at 105 cells per well, 96-well plate (B&D, New Jersey, NJ, USA) and serial dilutions of compounds were added into each well. After 24 h of incubation, the medium was replaced by fresh medium containing 10% MTT solution (Sigma), and the plate was incubated for 4 h in 5% CO2 at 37 °C. The absorbance at the wavelength of 595 nm was measured by microplate spectrophotometer (BioTek). Cytotoxicity was determined as a percentage of the maximum value after subtracting the background. PBS was used as a negative control and lysis buffer (10 mM Tris, pH 7.4, 1 mM EDTA and 0.1% Triton X-100) was used as a positive control.26, 27, 28
Statistical analysis
The results are presented as the mean±s.d. The statistical significance of the experimental results was determined by Student’s t-test. Values of P<0.05 were considered statistically significant. Prism version 5.0 was used for all statistical analyses.
Results
CST-resistant strain obtained
Initially, the correlation of absorbance with CFU was established for E. cloacae (ATCC 49141); (see Supplementary Figure S1a in Supplementary Materials). From the correlational result, 0.08 a.u. was determined to correspond to 5 × 105 CFU ml−1. This was used as the initial bacterial concentration applied in the antimicrobial susceptibility assays. Bactericidal activity was verified using 8 μg ml−1 of CST (see Supplementary Figure S1b). To induce resistance to CST, ½ MIC (4 μg ml−1) was utilized for sequential growth of E. cloacae. All three resistant strains, isolated after sequential cultivation in the presence of CST, demonstrated a considerable increase in CST tolerance growth in the presence of concentrations <64 μg ml−1 for R1 strain, 128 μg ml−1 for R2 and 256 μg ml−1 for R3 (see Supplementary Figures S2a–c). The E. cloacae colonies isolated from sequential cultivation without antibiotic were named NR1, NR2 and NR3, and showed MIC of 8 μg ml−1 of CST.
Distinguishing E. cloacae CST-susceptible and -resistant strains
Considering that CST-resistant strains showed an increased tolerance to this antibiotic, the protein profile (see Figure 1a) and the possibilities of distinguishing resistant from nonresistant strains were tested using MALDI-TOF MS.29 It was verified from the inspection of the dendrogram analysis that the control strains 'named nonresistant (NR)' have a small degree of distance from the original cell (ATCC 49141); (see Figure 1b). However, both NR and ATCC 49141 strains have a greater degree of distance from the CST-resistant strain (see Figure 1b). This result indicates that these resistant strains present physiological differences that can be rapidly detected by MALDI-TOF MS, therefore hinting that MALDI-TOF MS used in conjunction with the Biotyper analysis software can serve not only for species identification, but also to discriminate bacterial antibiotic resistance.
Comparison of the protein profile of E. cloacae strain (E. cloacae original cell ATCC 49141; strains of NR colistin (nonresistant 1, 2 or 3); R-colistin (resistant 1, 2 or 3)). (a) MALDI-TOF mass spectra of proteins analyzed on a MicroFlex LT mass spectrometer in positive linear mode using the MBT method. Axis ‘y’ shows the intensity and axis ‘x’ shows mass/charge. (b) MSP dendogram obtained from ‘main spectra profiles’ of E. cloacae strain (E. cloacae original cell ATCC 49141; strains of NR colistin (nonresistant 1, 2 or 3); R-colistin (resistant 1, 2 or 3)). MSP, main spectrum.
Bacterial growth and cross-resistance evaluation
To identify the standard of susceptibility of all E. cloacae strains (E. cloacae original cell ATCC 49141; strains NR-CST (nonresistant 1, 2 or 3); R-CST (resistant 1, 2 or 3)) to antibiotics of different classes, two methods were used: the automated and the diffusion disk. In such analyses, it was possible to verify that all strains have a similar susceptibility standard, except for CST. Several antibiotics were evaluated in this study (Supplementary Table S1), and the combined use of CST and CHL demonstrated synergistic effects (data not shown). In this case, the resistance process was only observed in CST-resistant strains, as was expected (Supplementary Table S1). These data suggest that the difference between CST-resistant and CST-susceptible strains was only reported for CST and not for other antibiotics. In summary, no cross-resistance was obtained for other antimicrobials tested here. When clinical strains were challenged with antibiotics, it was verified that both strains presented CST and β-lactam resistance. In addition, both strains showed resistance to antibiotics not previously identified. Although the 1437710 strain previously characterized by polymerase chain reaction showed the K. pneumoniae carbapenemase mechanism and also showed resistance to other antibiotics including tetracycline, tobramycin and piperacillin (Supplementary Table S1), the 1383251 strain was also resistant to amikacin (Supplementary Table S1), showing that both strains are multi-resistant for β-lactams, aminoglycoside and tertracycline.
Synergy evaluation by checkerboard assay
The results presented here refer to colistin sulfate salt, as there was no significant difference from those presented by CSM. Initially, the CST MICs against the CST-resistant E. cloacae strain were determined showing MICs of 64 μg ml−1 for R1 strain, 128 μg ml−1 for R2 and 256 μg ml−1 for R3. As the highest CST resistance was observed in E. cloacae R3, this strain was selected to perform synergistic assays. The E. cloacae R3 susceptibility was determined in the range between 2 and 256 μg ml−1 to CHL, vancomycin, erythromycin and ampicillin. The MIC observed for CHL treatment was 16 μg ml−1. Otherwise, vancomycin, erythromycin and ampicillin showed that the MIC was >256 μg ml−1. After MIC analyses, the synergism assays were performed using CST in combination with other antibiotics including CHL, vancomycin, erythromycin and ampicillin in the range of 2–256 μg ml−1. Four combinations of CST and CHL showed synergistic activities against E. cloacae R3 (64 μg ml−1 of CST+1 μg ml−1 of CHL or 32 μg ml−1 of CST+1 μg ml−1 of CHL or 16 μg ml−1 of CST+2 μg ml−1 of CHL or 8 μg ml−1 of CST+2 μg ml−1 of CHL), whereas three combinations showed indifferent activities against this bacterium (8 μg of CST+4 μg ml−1 of CHL and 4 μg ml−1 of CST+8 μg ml−1 of CHL). To confirm the synergistic effect of CST and CHL, further analyses were conducted against the two clinical E. cloacae strains: 1437710 and 1383251. These analyses showed similar synergistic effects of the combined CST and CHL treatment against these clinical strains and also in the subculture of E. cloacae ATCC 49141, which resulted in major resistant level to CST, named E. cloacae R3 (Table 1). CST combined with vancomycin, erythromycin and ampicillin was indifferent, not showing any synergistic effect against such bacterial strains (data not shown).
Cell cytotoxicity assay
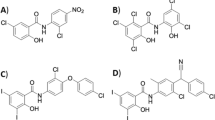
As described in the checkerboard antimicrobial assay, the results presented here also refer to colistin sulfate salt, as there was no significant difference from that presented by CSM. To evaluate whether the combination of antibiotics proposed here could cause any damage to mammalian host cells, RAW 264.7 and VERO cells were incubated with different concentrations of CST and CHL alone and in combination. MTT assay revealed that the use of CHL at 256 μg ml−1 (4 × MIC); (Figure 2) and CST (Figure 2b) reduced cell viability for ~39.7% (P<0.01) in comparison with the control. When cells were treated with 128 μg ml−1 CST (P<0.05), the cell viability was reduced to 26.3%. Cells treated with CHL at lower concentrations showed a smooth cell viability reduction without statistical significance. The combination of CHL and CST in concentrations of 4 and 128 μg ml−1, respectively, decreased cell viability to 23.8% (P<0.05); (Figure 2c). Furthermore, the CHL and CST combination at concentrations of 8 and 64 μg ml−1, respectively, decreased cell viability to 25.3% (P<0.05); (Figure 2d).
Effect of antibiotics on cell viability RAW 264.7 (white bars) and Vero cells (black bars) after 24 h with different concentrations of antibiotics including (a) chloramphenicol (CHL; 2–256 μg ml−1), (b) colistin sulfate salt (CST; 2–256 μg ml−1), (c) a combination of CHL (0.03–4 μg ml−1) and CST (1–128 μg ml−1), and (d) CHL (0.06–8 μg ml−1) and CST (0.05–64 μg ml−1). Cell viability was measured following a standard MTT assay procedure. The mean absorbance of the control values representing 100% cell viability, and the mean absorbance of treated cells was related to control values to determine sensitivity. Error bars represent s.d. from mean cell viability of three independent replicates.
Discussion
Infections caused by multidrug-resistant E. cloacae strains are increasing worldwide.30 This situation has been aggravated by widespread dissemination and by difficulties in the precise identification of such species. Current phenotypical and molecular characterizations present difficulties in identifying six species of the Enterobacter genus including E. cloacae,E. asburiae,E. hormaechei,E. kobei,E. ludwigii and E. nimipressuralis.31
Although both automated methods have been efficient in identifying E. cloacae species, both require more time (24–48 h) when compared with the utilization of MALDI-TOF MS, which is capable of identifying strains in a few minutes. In addition, the use of the Biotype 100 (bioMérieux) system and the other conventional tests including biochemical, microbiological and molecular identification at the DNA and messenger RNA levels32, 33, 34 is necessary in some cases for accurate identification. MALDI-TOF MS analyses allow for the distinction of susceptible and CST-resistant bacteria. Recent studies have demonstrated that MALDI-TOF MS analysis may be used to differentiate bacterial strains with resistance to a single antibiotic such as carbapenem-resistant Bacteroides fragilis,35 methicillin-resistantStaphylococcus aureus,36 E. coli-resistant to streptothricin or streptomycin or kanamycin,37 and fluoroquinolone-resistant Streptococcus pneumoniae.38
To identify the susceptibility of strains to diverse antibiotics, four methods were used: the two automated methods (VITEK and MicroScan), the microdilution method and the diffusion disk method. In these analyses, all E. cloacae strains were verified to be resistant to penicillin, first-, second- and third-generations of cephalosporin, monobactam, ampicillin–sulbactam and amoxicillin–clavulanate (Supplementary Table S1). According to Hilty et al.,39 E. cloacae is naturally resistant to penicillin, first- and second-generation cephalosporin and amoxicillin–clavulanic acid, owing to the production of chromosomal AmpC β-lactamases. Many studies support the use of CST in combination with other antibiotics including cecropin A against clinical CST-resistant strains of A. baumannii.40 In other studies, utilizing A. baumannii susceptible to CST, synergistic effects were demonstrated with the use of CST with vancomycin or trimethoprim, and also with trimethoprim and sulfamethoxazole.41 In these same studies, a decrease in the growth of CST-resistant strains of A. baumannii and K. pneumoniae was also reported; however, synergistic effects in any combination were verified against CST-resistant P. aeruginosa strains.41 In a recent study, Phee et al.42 showed that the combination of CST and fusidic acid is efficient for treatment of multidrug-resistant A. baumannii infections.
For these reasons, the synergistic effects of CST with other antibiotics that differ greatly in physicochemical and biopharmaceutical properties in E. cloacae CST-resistant strains were evaluated here. The synergistic CST (polymyxin) effects in association with other antibiotics such as vancomycin (glycopeptide), erythromycin and ampicillin (both β-lactam), and CHL (protein synthesis inhibitor) were analyzed, demonstrating that the association of CST with β-lactams, erythromycin and ampicillin, and a glycopeptide (vancomycin) were ineffective. A similar result was found in a previous study using vancomycin plus CST against CST-resistant P. aeruginosa strains.41 However, in this study, the combination of vancomycin with CST was effective against CST-resistant A. baumannii,P. aeruginosa and K. pneumoniae.41
It is important to emphasize that synergistic effects of CST in association with CHL against induced CST-resistant strains (R3), as well as clinical strains 1437710 and 1383251 were observed here. The mechanisms of resistance observed in clinical isolated strains were not determined until now. Here, small quantities of CST (32 μg ml−1) and CHL (8 μg ml−1) were capable of reducing the development of multi-resistant microorganisms, demonstrating that this combination could be utilized in clinical strategies to increase the potential antimicrobial activity and reduce the deleterious effects of these antimicrobials as observed in cytotoxic assays (Figures 1a), thus improving the effectiveness of clinical treatment. However, it is important to emphasize that the adverse events of the two drug in combination will need to be characterized thoroughly.
It was evidenced that outer membrane variations may influence the hydrophobic CST-bacterium interaction.43 Furthermore, methodological considerations such as salt concentration, pH of the electrolyte in which cells are suspended, and adherence of CST to a glass and plastic surface may lower the available concentrations of these drugs in test systems.44 Previous studies have reported the susceptibility of E. cloacae to CHL alone45 and in combination with ethyl acetate extract of Salvia officinalis.46 The activity of CHL in association with ethyl acetate extract of S. officinalis also decreases the growth of S. aureus,Bacillus subtilis,K. pneumoniae,E. coli and Proteus mirabilis.46 Moreover, the synergistic effect of CHL in association with P5, a hybrid peptide of cecropin and magainin 2, is able to reduce S. aureus growth.47 Similar data were obtained by the combination of moxifloxacin, a fourth-generation fluoroquinolone and piperacillin–tazobactam or additionally the combination of moxifloxacin with cefepime, a fourth-generation cephalosporin.44
In addition, the triple combination of CST with cefepime and amikacin, an aminoglycoside, has been used against E. cloacae cefotaxime-susceptible strains,48 as well as in combat of E. cloacae ceftazidime-resistant strains.47 In these two assays, the combination of these antibiotics caused a reduction of pulmonary infection caused by that were resistant and susceptible to third-generation cephalosporins.47, 48 In another study, a triple combination of CST, rifampicin and imipenem44 was reported as effective in controlling the E. cloacae producer of metallo β-lactamases. These authors described the combination of a drug that acts in cell walls plus another that acts in cell membranes, in association inhibiting DNA and RNA synthesis, and which is capable of eliminating the infection caused by these bacteria.
Several studies have reported the use of CHL in combination with other compounds, such as fosfomycin-CHL, which was synergistic against Salmonella sp.,47 CHL with ampicillin, carbenicillin and cephaloridine against strains of Enterobacteriaceae.47 CHL and ampicillin were active against Haemophilus influenzaemeningitis.47 However, it is noteworthy that none of these studies evaluated the effect of cytotoxic compounds.
It is well established that CHL has numerous toxic effects such as reticulocytopenia, thrombocytopenia and metabolic acidosis, and severe cases can cause aplastic anemia, often resulting in the death of patients.47 In this study, it is noteworthy that CST and CHL were toxic only at a concentration of 256 μg ml−1, and the effective CHL concentration that has bactericidal effects on strains of E. cloacae ATCC 49141 has an MIC that corresponds to 16 μg ml−1. This concentration also has bactericidal effects on nonresistant E. cloacae subcultures and those resistant to CST, as well as on one of the clinical strains, and at this concentration, toxic effects of the antibiotic were not observed. However, for clinical strain, the MIC was 512 μg ml−1, indicating that therapy with CHL and CST was not the best choice, as an infection caused by this strain resulted in the need for extremely high dosages that would promote cytotoxicity.
Considering that, in some cases, the combination of two or more antibiotics can cause toxic effects, the in vitro cytotoxicity was analyzed here. For this purpose, RAW 264.7 monocyte cells were used to evaluate the safeness of the proposed therapy. In these analyses, a reduction of ~40% of cell viability was observed when mammalian cells were treated with 256 μg ml−1 of CHL and CST concentrations. Similar results have been observed with the use of CHL at concentrations >200 μg ml−1, where 50% cytotoxicity was observed.17, 18, 25, 27
However, when utilizing CHL and CST, in two combinations referent to synergistic effect as 1 μg ml−1 of CHL+32 μg ml−1 of CST, or 2 μg ml−1 of CHL+16 μg ml−1 of CST, cytotoxic effects on RAW 264.7 and VERO cells were not observed here. Thus, the results obtained here strongly indicate that the combination of these two antibiotics could be a feasible strategy for allowing dose reductions for effective bacterial control with a concomitant reduction in the collateral toxic effects in mammalian cells. Our data suggest that the CST–CHL combination shows no cytotoxic effects in doses 5 × higher than the MIC. Furthermore, this could be observed as a first step for future in vivo studies.
In conclusion, the synergistic effects of CST with CHL against induced CST-resistant E. cloacae strains, as well as against clinical multi-resistant strains were clearly demonstrated. The clinical application of these two antibiotics might be considered for infection control, as the synergistic effects could decrease the dose, treatment costs and toxic effects inherent to CST and CHL treatments.
References
He, G. X. et al. EmmdR, a new member of the MATE family of multidrug transporters, extrudes quinolones from Enterobacter cloacae. Arch. Microbiol. 193, 759–765 (2011).
Yang, F. C., Yan, J. J., Hung, K. H. & Wu, J. J. Characterization of ertapenem-resistant Enterobacter cloacae in a Taiwanese university hospital. J. Clin. Microbiol. 50, 223–226 (2012).
Heller, I., Grif, K. & Orth, D. Emergence of VIM-1-carbapenemase-producing Enterobacter cloacae in Tyrol, Austria. J. Med. Microbiol. 61, 567–571 (2012).
Panopoulou, M. et al. Emergence of VIM-12 in Enterobacter cloacae. J. Clin. Microbiol. 48, 3414–3415 (2010).
Hornsey, M. et al. Emergence of AcrAB-mediated tigecycline resistance in a clinical isolate of Enterobacter cloacae during ciprofloxacin treatment. Int. J. Antimicrob. Agents 35, 478–481 (2010).
Nigro, S. J. & Hall, R. M. GIsul2, a genomic island carrying the sul2 sulphonamide resistance gene and the small mobile element CR2 found in the Enterobacter cloacaesubspecies cloacae type strain ATCC 13047 from 1890, Shigella flexneri ATCC 700930 from 1954 and Acinetobacter baumannii ATCC 17978 from 1951. J. Antimicrob. Chemother. 66, 2175–2176 (2011).
Coates, A. R. & Halls, G. Antibiotics in phase II and III clinical trials. Handb. Exp. Pharmacol. 211, 167–183 (2012).
Zucca, M., Scutera, S. & Savoia, D. New antimicrobial frontiers. Mini. Rev. Med. Chem. 11, 888–900 (2011).
Moffatt, J. H. et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob. Agents Chemother. 54, 4971–4977 (2010).
Gupta, S. et al. Colistin and polymyxin B: a re-emergence. Indian J. Crit. Care Med. 13, 49–53 (2009).
Srivastava, S. & Ghosh, J. K. Introduction of a lysine residue promotes aggregation of temporin L in lipopolysaccharides and augmentation of its antiendotoxin property. Antimicrob. Agents Chemother. 57, 2457–2466 (2013).
David, S. A. Antimicrobial peptides for gram-negative sepsis: a case for the polymyxins. Front. Immunol. 3, 252 (2012).
Lin, X. M., Yang, J. N., Peng, X. X. & Li, H. A novel negative regulation mechanism of bacterial outer membrane proteins in response to antibiotic resistance. J. Proteome. Res. 9, 5952–5959 (2010).
Shlaes, D. M. New beta-lactam-beta-lactamase inhibitor combinations in clinical development. Ann. N. Y. Acad. Sci. 1277, 105–114 (2013).
Naghmouchi, K. et al. Synergistic effect between colistin and bacteriocins in controlling gram-negative pathogens and their potential to reduce antibiotic toxicity in mammalian epithelial cells. Antimicrob. Agents Chemother. 57, 2719–2725 (2013).
Wallace, S. J., Nation, R. L., Li, J. & Boyd, B. J. Physicochemical aspects of the coformulation of colistin and azithromycin using liposomes for combination antibiotic therapies. J. Pharm. Sci. 102, 1578–1587 (2013).
Kasiakou, S. K. et al. Combination therapy with intravenous colistin for management of infections due to multidrug-resistant Gram-negative bacteria in patients without cystic fibrosis. Antimicrob. Agents Chemother. 49, 3136–3146 (2005).
Olofsson, S. K. & Cars, O. Optimizing drug exposure to minimize selection of antibiotic resistance. Clin. Infect. Dis. 45 (suppl 2), S129–S136 (2007).
Pomales-Lebron, A. & Fernandez, C. A method for estimating the number of bacteria in liquids and tissues. J. Bacteriol. 64, 837–845 (1952).
CLSI. in Approved Standard - 8th ed. CLSI document M07-A8 (Clinical and Laboratory Standards Institute, Wayne, PA, 2009).
Peng, X. et al. Proteomic analysis of the sarcosine-insoluble outer membrane fraction of Pseudomonas aeruginosa responding to ampicilin, kanamycin, and tetracycline resistance. J. Proteome. Res. 4, 2257–2265 (2005).
Calderaro, A. et al. Identification of Borrelia species after creation of an in-house MALDI-TOF MS database. PLoS One. 9, e88895 (2014).
Mellmann, A. et al. High interlaboratory reproducibility of matrix-assisted laser desorption ionization-time of flight mass spectrometry-based species identification of nonfermenting bacteria. J. Clin. Microbiol. 47, 3732–3734 (2009).
CLSI. in Twentieth Informational Supplement CLSI document M100-S20 (Clinical and Laboratory Standards Institute, Wayne, PA, 2010).
Gordon, N. C., Png, K. & Wareham, D. W. Potent synergy and sustained bactericidal activity of a vancomycin-colistin combination versus multidrug-resistant strains of Acinetobacter baumannii. Antimicrob. Agents Chemother. 54, 5316–5322 (2010).
Lopez-Abarrategui, C. et al. Functional characterization of a synthetic hydrophilic antifungal peptide derived from the marine snail Cenchritis muricatus. Biochimie 94, 968–974 (2012).
Silva, O. N. et al. Cn-AMP1: a new promiscuous peptide with potential for microbial infections treatment. Biopolymers 98, 322–331 (2012).
Pasupuleti, M., Schmidtchen, A., Chalupka, A., Ringstad, L. & Malmsten, M. End-tagging of ultra-short antimicrobial peptides by W/F stretches to facilitate bacterial killing. PLoS ONE 4, e5285 (2009).
Josten, M. et al. Analysis of the matrix-assisted laser desorption ionization-time of flight mass spectrum of staphylococcus aureus identifies mutations that allow differentiation of the main clonal lineages. J. Clin. Microbiol. 51, 1809–1817 (2013).
Kremer, A. & Hoffmann, H. Prevalences of the Enterobacter cloacae complex and its phylogenetic derivatives in the nosocomial environment. Eur. J. Clin. Microbiol. Infect. Dis. 31, 2951–2955 (2012).
Paauw, A. et al. Genomic diversity within the Enterobacter cloacaecomplex. PLoS ONE 3, e3018 (2008).
Risch, M. et al. Comparison of MALDI TOF with conventional identification of clinically relevant bacteria. Swiss Med. Wkly. 140, w13095 (2010).
Munoz Bellido, J. L., Vega Castano, S., Ferreira, L., Sanchez Juanes, F. & Gonzalez Buitrago, J. M. Proteomic applications in the clinical microbiology laboratory. Enferm. Infecc. Microbiol. Clin. 30, 383–393 (2012).
Mezzatesta, M. L., Gona, F. & Stefani, S. Enterobacter cloacae complex: clinical impact and emerging antibiotic resistance. Future Microbiol. 7, 887–902 (2012).
Wybo, I. et al. Differentiation of cfiA-negative and cfiA-positive Bacteroides fragilis isolates by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J. Clin. Microbiol. 49, 1961–1964 (2011).
Wolters, M. et al. MALDI-TOF MS fingerprinting allows for discrimination of major methicillin-resistant Staphylococcus aureus lineages. Int. J. Med. Microbiol. 301, 64–68 (2011).
Muroi, M., Shima, K., Igarashi, M., Nakagawa, Y. & Tanamoto, K. Application of matrix-assisted laser desorption ionization-time of flight mass spectrometry for discrimination of laboratory-derived antibiotic-resistant bacteria. Biol. Pharm. Bull. 35, 1841–1845 (2012).
Malakhova, M. V. et al. MALDI-ToF mass-spectrometry in analysis of genetically determined resistance of Streptococcus pneumoniae to fluoroquinolones. Antibiot. Khimioter. 52, 10–17 (2007).
Hilty, M. et al. Characterisation and clinical features of Enterobacter cloacae bloodstream infections occurring at a tertiary care university hospital in Switzerland: is cefepime adequate therapy? Int. J. Antimicrob. Agents 41, 236–249 (2013).
Saugar, J. M. et al. Activity of cecropin A-melittin hybrid peptides against colistin-resistant clinical strains of Acinetobacter baumannii: molecular basis for the differential mechanisms of action. Antimicrob. Agents Chemother. 50, 1251–1256 (2006).
Vidaillac, C., Benichou, L. & Duval, R. E. In vitrosynergy of colistin combinations against colistin-resistant Acinetobacter baumannii,Pseudomonas aeruginosa, and Klebsiella pneumoniae isolates. Antimicrob. Agents Chemother. 56, 4856–4861 (2012).
Phee, L. M. et al. Colistin and fusidic acid, a novel potent synergistic combination for treatment of multidrug-resistant Acinetobacter baumannii infections. Antimicrob. Agents Chemother. 59, 4544–4550 (2015).
Mimoz, O. et al. Cefepime and amikacin synergy in vitro and in vivo against a ceftazidime-resistant strain of Enterobacter cloacae. J. Antimicrob. Chemother. 41, 367–372 (1998).
Jung, R., Husain, M., Choi, M. K. & Fish, D. N. Synergistic activities of moxifloxacin combined with piperacillin-tazobactam or cefepime against Klebsiella pneumoniae,Enterobacter cloacae, and Acinetobacter baumannii clinical isolates. Antimicrob. Agents Chemother. 48, 1055–1057 (2004).
Traub, W. H., Haberle, R. & Bauer, D. Characterization of two clinical, multiple-drug-resistant isolates of Enterobacter cloacae. Chemotherapy 30, 308–321 (1984).
Stefanovic, O. D., Stanojevic, D. D. & Comic, L. R. Synergistic antibacterial activity of Salvia officinalis and Cichorium intybus extracts and antibiotics. Acta. Pol. Pharm. 69, 457–463 (2012).
Park, Y. et al. Synergism of Leu-Lys rich antimicrobial peptides and chloramphenicol against bacterial cells. Biochim. Biophys. Acta. 1764, 24–32 (2006).
Mimoz, O. et al. Cefepime and amikacin synergy against a cefotaxime-susceptible strain of Enterobacter cloacae in vitro and in vivo. J. Antimicrob. Chemother. 39, 363–369 (1997).
Acknowledgements
This study was supported by grants from CNPq, CAPES, FUNDECT, FAPDF, EMBRAPA, UCB and UCDB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on The Journal of Antibiotics website
Supplementary information
Rights and permissions
About this article
Cite this article
Lima, T., Silva, O., de Almeida, K. et al. Antibiotic combinations for controlling colistin-resistant Enterobacter cloacae. J Antibiot 70, 122–129 (2017). https://doi.org/10.1038/ja.2016.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2016.77
This article is cited by
-
The dose regimen formulation of doxycycline hydrochloride and florfenicol injection based on ex vivo pharmacokinetic-pharmacodynamic modeling against the Actinobacillus pleuropneumoniae in pigs
Animal Diseases (2023)
-
Overcoming mcr-1 mediated colistin resistance with colistin in combination with other antibiotics
Nature Communications (2018)