Abstract
The dominant role of biofilm-associated protein (Bap) in Staphylococcus aureus biofilm development prompted us to investigate Bap as a potential target for proteinase-mediated biofilm dispersion. Biofilm assay in microtitre plates showed that proteinase K hampered the early adhesion of cells as well as biofilm development. Proteinase K treatment of 24- and 48-h-old biofilms showed enhanced dispersion of bap-positive S. aureus biofilm; however, proteinase K did not affect the bap-negative S. aureus biofilm. When antibiotics were used in combination with proteinase K, significant enhancement in antibiotic action was noticed against bap-positive S. aureus biofilm. This study establishes that antibiotics in combination with proteinase K can be used for controlling S. aureus biofilms in whose development Bap surface protein has a major role. We propose that Bap protein could be a potential target for therapeutic control of S. aureus infections (for example, bovine mastitis).
Similar content being viewed by others
Introduction
Biofilms are complex non-transient microbial communities attached to surfaces and embedded in an extracellular polymeric matrix.1, 2 A mature biofilm is generally composed of polysaccharides, proteins and extracellular DNA. Generally, the process of biofilm development proceeds through a set of discreet stages as follows: (a) adherence of cells to a substratum, (b) development of micro-colonies, (c) maturation of micro-colonies into biofilms, and (d) detachment of bacteria and dispersal of motile cells.3 Among the variety of bacterial species, Staphylococcus aureus and Staphylococcus epidermidis are the predominant microorganisms causing nosocomial infections, mainly associated with implanted medical devices such as catheters, cardiac valves and orthopaedic prostheses.4 The biofilm mode of S. aureus life enhances its recalcitrance and enables the bacterium to survive antibiotic assault.5 This also imposes a challenge to host defence mechanisms and antimicrobial therapy.5, 6 Biofilm dispersal is a natural process, which allows bacterial cells to leave biofilm and migrate to a more favourable environment for resettlement. However, during this transition phase, bacteria lose the advantages of the biofilm mode of life and become relatively more susceptible to antimicrobial agents.
A recent study reported that biofilm disassembly/dispersion by signalling pathway has a very important role in pathogenicity and environmental dispersion of bacteria.7 To promote dispersion, cells synthesize various bacterial extra polymeric substances degrading enzymes.8, 9 Dispersal mechanisms vary in different bacteria and this event is considered as a novel approach to treat drug-resistant S. aureus infections in body implants and catheters.10 In spite of its high potential, there is not much information on biofilm dispersion products because of the ratio of higher investment cost to commercial outcome.11
Quorum sensing, among other things, is involved in biofilm dispersion. In the context of S. aureus, it was reported that biofilm dispersal is controlled by Agr-quorum-sensing system.12 There are several reports on surface protein-dependent biofilm formation by S. aureus, among which protein A and biofilm-associated protein (Bap) were studied in detail.13, 14 Bap is a large, multi-domain, cell surface-anchored protein, which has been reported to have a crucial role in the early stages of S. aureus biofilm development.14 The importance of Bap in S. aureus biofilm was so significant that bap-positive S. aureus can form biofilm even though its ica operon was disrupted.14, 15 The ica operon synthesizes polymeric intercellular adhesin (PIA), a major constituent in S. aureus biofilm. The role of PIA component in the S. aureus biofilm formation was studied in detail.16 Earlier studies showed that the presence of bap gene and its homologues was restricted to bovine mastitis.14, 15, 17 Of late, the presence of the bap gene was also reported in human nosocomial infections.18 Furthermore, the increase in number of occurrences of bap also indicates the presence of alternate PIA-independent mechanism of biofilm formation.15, 19
S. aureus secretes four major extracellular proteases, such as metalloprotease aureolysin (aur), two cysteine proteases (scpA and sspB) and seven serine proteases.20 Theoretically, these extracellular proteases contribute to biofilm detachment; however, their role in staphylococci is still unknown.12, 20, 21 An earlier study showed that among the above four classes of extracellular proteases, serine proteases are dominant and are believed to have a major role in biofilm detachment.12 Proteinase K is a highly reactive serine protease, which is stable in a broad range of conditions, such as pH, buffer salts, detergents (SDS) and temperature.22 This makes proteinase K an ideal choice for disassembly among the various proteases. According to a previous report, biofilms of S. epidermidis, S. lugdunensis and S. aureus showed susceptibility to enzymatic treatments, which was dependent on chemical composition of their biofilm matrices.23 Thus, mimicking the extracellular degrading enzymes is a possible approach that could be used to disintegrate the biofilms. Concurrent use of antibiotics can kill the detached cells and help in eliminating the infection. It was reported that proteinase K was more effective in dispersing S. aureus biofilm when PIA content was very less and the biofilm was probably dominated by the presence of proteins.23 In the above study, the authors used proteinase K at a high concentration (1 mg ml−1), which may increase the cost of treatment. Thus, there is a need for generating data on the use of lesser concentrations of proteinase K for biofilm dispersal. It is already discussed that in Bap-expressing S. aureus strains, the protein has a major role in establishing cell to cell interaction.14 Thus, targeting Bap with a protease may be a very useful approach to control staphylococci infections.
Antibiotics are used to eradicate biofilm infections; wanton use of antibiotics led to selection pressure and resulted in development of resistant strains among many pathogenic bacteria.24, 25 This has motivated researchers to look for alternative therapeutic approaches, which reduce the use of antibiotics or completely eliminate the need of antibiotics for biofilm removal.24, 25, 26 In this study, we investigated whether proteinase K treatment can be used to enhance biofilm dispersal through cleavage of the surface-anchoring protein in Bap-dependent S. aureus biofilm. Experiments were carried out using the bap-positive S. aureus V329 and the bap-isogenic mutant M556. As Bap contains four Ca2+-binding EF-hand motifs, we also investigated whether binding of Ca2+ to Bap would confer any resistance towards proteinase K-mediated biofilm dispersal. We tested whether proteinase K could be used in combination with antibiotics to enhance the dispersal/control of biofilms.
Materials and methods
Microorganisms and culture conditions
Two S. aureus strains were investigated. The bap-positive S. aureus V329 was originally isolated from bovine mastitis and is known as a hyper-biofilm producing S. aureus strain. The bap-isogenic mutant S. aureus M556 was generated by transposon insertion in the bap gene of S. aureus V329. Transposon was inserted into the downstream part of the bap gene, resulting in the production of truncated protein lacking the cell wall anchoring region.14 Hence, in M556 the Bap protein is synthesized but is non-functional. For each experiment, single colonies were picked from Tryptic Soy Agar culture plates and inoculated in Tryptic Soy Broth (TSB) medium supplemented with 0.25% glucose, and incubated at 37 oC at 150 r.p.m. Overnight grown cultures were used for all experiments.
Quantitative biofilm assay
Biofilm assay was performed in microtitre plates to estimate the dispersion action. S. aureus V329 and M556 biofilms were grown on pre-sterilized 96-well flat-bottom polystyrene microtitre plates. Biofilm quantification was done by classical crystal violet assay.27 For dissolution of bound crystal violet, 33% acetic acid was used.28 Biofilm growth was monitored in terms of absorbance at 570 nm using a micro plate reader (Multiskan; Thermo Labsystems, Beverly, MA, USA). The overnight grown cultures of the two strains in TSB supplemented with 0.25% glucose were diluted 1:40 in sterile TSB medium and added to the microtitre plate wells. The plates were incubated at 37 °C for 2–6 h based on the experimental plan.
Proteinase K preparation
The enzyme proteinase K was purchased from Sigma-Aldrich (St Louis, MO, USA), which had specific activity of 30 units mg−1, where one unit is defined as the amount of enzyme needed to hydrolyse urea-denatured haemoglobin to produce colour equivalent to 1.0 μM of tyrosine per min at pH 7.5 at 37 °C (colour reaction by Folin-Ciocalteu reagent). The working concentration of proteinase K was chosen as 2 μg ml−1 in most of the experiments. To inactivate the proteinase K after the prescribed experimental time, 2 mM of freshly prepared phenyl methyl sulphonyl fluoride was added.
Early adhesion assay
Overnight grown cultures in TSB supplemented with 0.25% glucose were diluted 1:40 in sterile TSB medium, and mild proteinase K treatment (2 μg ml−1) was given to the cells, to cleave and remove all surface proteins. Then, the proteinase K-treated cells were added to 96-well microtitre plates. Untreated S. aureus cells were used as control. To evaluate the role of surface protein in initial adhesion, post proteinase K-treated cells (proteinase K was inactivated by addition of phenyl methyl sulphonyl fluoride) were allowed to adhere for different time intervals, that is. 0, 1, 2 and 3 h at 37 oC, to aid in surface protein-mediated adherence. Adherence of cells was measured by crystal violet assay as described earlier.
Viable cell counts in biofilm after antibiotic-proteinase K treatment
To investigate the anti-biofilm activity of proteinase K in combination with antibiotics, streptomycin, gentamycin and ampicillin were used against S. aureus V329 biofilms. The antibiotic concentration was chosen as 10 and 50 times the minimum inhibitory concentration against S. aureus V329 planktonic bacterial cells. Proteinase K treatment was given in combination with 10 × concentration of antibiotics. S. aureus V329 biofilms were grown in 96-well microtitre plates at 37 °C and 150 r.p.m. After 24 h, planktonic cells were aspirated by pipette, and the biofilms were gently rinsed twice with sterile phosphate-buffered saline. After rinsing, the biofilms were treated with antibiotics alone (gentamycin, 150 and 750 μg ml−1; streptomycin, 100 and 500 μg ml−1; ampicillin 100 and 500 μg ml−1) and antibiotics–proteinase K combinations, as per the experimental plan. After 24 h of treatment, planktonic cells were aspirated by pipette and biofilms were gently rinsed twice with phosphate-buffered saline. Phosphate-buffered saline (200 μl) was added to each well and the biofilm cells were dislodged by ultrasonication for 5 min. Cells released from the biofilms were collected and the viable cell count was obtained by plating on Tryptic Soy Agar media and incubated at 37 °C overnight.
Confocal laser scanning microscopy study
Confocal laser scanning microscopy (CSLM) analysis was done with a Leica TCS-SP2 AOBS microscope (Leica Microsystem, Hessen Wetzlar, Germany). V329 biofilms were grown on glass cover slips in six-well cell culture plates. Biofilms (24-h-old) were treated with proteinase K for a given time period, gently rinsed with phosphate-buffered saline and stained with 0.2% acridine orange for 5 min. A thin cover slip was placed over the biofilms and the cover slip was mounted upside down over the objective lens of CLSM, equipped with DM IRE 2-inverted microscope (Leica Microsystems). Image stacks were collected from 20 different random points of the biofilm. To get statistically significant data, each experiment was repeated three times. Image stacks were analysed by COMSTAT29 and Imaris software (version 6.2, Bitplane Scientific Solutions, Zurich, Switzerland).
Statistical analysis
Two-tailed Student’s t-test was used to determine the differences in biofilm formation between the groups. Differences were considered statistically significant when P-value was <0.005.
Results
Proteinase K interferes with early adhesion of V329 cells
Figure 1 illustrates the results of early adhesion assay, which shows that proteinase K treatment hampered the primary attachment of V329 cells to microtitre plate. The adherence property of the V329 cells was restored when proteinase K was inactivated by the addition of phenyl methyl sulphonyl fluoride. Figure 1 also shows the number of adhered cells increased with time. On the contrary, strain M556 did not show any change in adhesion or biofilm formation in the presence of proteinase K. This observation signifies the Bap surface protein is important in the early phase of biofilm formation by V329.
Effect of proteinase K on Bap-mediated early adhesion. Results are average of five replicates ±1 s.d. and are representative of three independent experiments. *P-value <0.0001 as compared with S. aureus cells exposed to no proteinase K (control). The 0-h point shows that proteinase K was not inhibited.
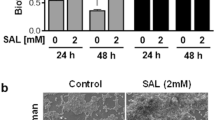
Ca2+binding to EF-hand domains in Bap do not render protection towards proteolytic degradation
As Bap contains Ca2+-binding EF-hand motif, we evaluated whether binding of Ca2+ to Bap would confer resistance against proteinase K-mediated degradation. Biofilm assay showed that in the presence of proteinase K, biofilm formation of V329 was inhibited. Addition of Ca2+ (3 mM) did not influence the proteinase K-mediated inhibition of early adherence of cells and biofilm development (Figure 2). This observation demonstrates that binding of Ca2+ to Bap does not confer any immunity against proteolytic degradation.
Proteinase K enhances dispersal in bap-positive S. aureus
To investigate the biofilm dispersal activity, a range of proteinase K concentrations were tested against mature bap-positive S. aureus V329 biofilms. Figure 3 shows dose-dependent dispersal of V329 biofilm. Approximately 36% biofilm dispersal was observed with 2 μg ml−1 proteinase K treatment, whereas the highest dose of 250 μg ml-1 showed ∼76% biofilm dispersal. Therefore, it was clearly evident from this observation that increasing concentration of proteinase K did not result in proportional enhancement of dispersal, and 100% biofilm dispersal could not be achieved. To keep this approach economical, 2 μg ml−1 of proteinase K was chosen for further experiments.
Figure 4 illustrates that proteinase K treatment of 24- and 48-h-old V329 and M556 biofilms has enhanced the dispersion of bap-positive V329 biofilm, whereas the bap-isogenic mutant M556 biofilm was not at all dispersed. Figure 4 further shows that M556 forms a rather weak biofilm as compared with V329 at 24 h, hence estimating M556 biofilm dispersal was difficult and rather inappropriate. However, after 48 h it also produced significant biofilm and it was clearly evident that proteinase K treatment did not disperse M556 biofilm. On the basis of the crystal violet assay data, percentage removal of V329 biofilm by proteinase K was estimated to be 15, 24 and 30% after 2, 4 and 6 h of contact time, respectively.
The CSLM study further strengthened the observations of the biofilm assay. The V329 biofilm (Figure 5) after 2, 4 and 6 h of contact with proteinase K showed considerable dispersion. COMSTAT analysis of the CLSM image showed that the maximum biofilm thickness was reduced from 28.09±7.24 to 15.82±6.47 μm (P-value=0.0008, n=10), whereas the average thickness was reduced from 21.41±4.68 to 9.82±3.77 μm (P-value <0.0001, n=10; Figure 6a). Total biofilm biomass (μm3 μm−2) was reduced from 34 to 62% after 6 h of proteinase K treatment (Figure 6b). A substantial change was noticed in the maximum diffusion distance that reduced from 1.28±0.26 to 1.03±0.24 (P-value=0.0446, n=10; Figure 6c). Considerable reduction was observed in the average diffusion distance, which was reduced from 0.331±0.194 to 0.0165±0.002 μm (P-value <0.0001; Figure 6c). Another important change in the biofilm parameter that determines the interface for exchange of the metabolites, flow of nutrient/antimicrobial agents through biofilm, was roughness coefficient and surface to biovolume ratio (Figures 6d, e and Supplementary Table 1). Enhanced roughness coefficient and surface to biovolume ratio indicates more accessibility of nutrients, as well as penetration of antimicrobial agents into the biofilm.
Proteinase K enhances antibiotic efficacy against bap-positive S. aureus biofilm
Figure 7 shows that efficacy of the antibiotics (gentamycin, streptomycin and ampicillin) increased when the biofilm was treated with proteinase K. The addition of proteinase K in combination with antibiotics had more impact against the S. aureus biofilm cells when compared with the addition of antibiotics alone. When the antibiotic concentration was increased by five times, one log reduction in the CFU count was observed. On the other hand, the addition of 2 μg ml−1 proteinase K in combination with antibiotic resulted in a 3-log reduction in the case of gentamycin and streptomycin, and a 1.3-log reduction in the case of ampicillin.
Antimicrobial efficacy of antibiotics in combination of proteinase K against 48-h-old S. aureus V329 biofilm. Results are average of five replicates ±1s.d. and are representative of three independent experiments. Proteinase K was used at 2 μg ml−1. GEN 150, gentamycin 150 μg ml−1; GEN 750, gentamycin 750 μg ml−1; STR 100, streptomycin 100 μg ml−1; STR 500, streptomycin 500 μg ml−1; AMP 100, ampicillin 100 μg ml−1; AMP 500, ampicillin 500 μg ml−1. *P<0.05 as compared with corresponding S. aureus biofilm exposed to no proteinase K.
Discussion
There are many reports on the role of surface proteins in S. aureus infection and biofilm development.16, 17 Among the various proteins, Bap has been reported to have a major role in early adhesion, as well as in biofilm development.17 In this study we found that when mild treatment of proteinase K was given to S. aureus V329 cells to remove surface proteins, a reduction in early adhesion was observed. The observations emphasize the fact that Bap has an important role in early adhesion, as similar effect was not observed in bap-negative M556. In general, metal-binding proteins are structurally stable and show resistance towards proteolytic degradation.30 The presence of potential Ca2+-binding domain in Bap intrigued us to check whether binding of Ca2+ to Bap resulted in protection against proteolytic cleavage and, in turn, against biofilm dispersion. Biofilm assay using Ca2+ alone and Ca2+ with proteinase K showed that Ca2+ offered no protection to Bap.
Treatment of 24-h-old S. aureus biofilm with proteinase K showed that the enzyme enhanced the dispersion of bap-positive V329 in a time-dependent manner (2–6 h) but did not affect the M556 biofilm, as up to 24 h M556 did not produce significant biofilm. Thus, 48-h-old biofilms of V329 and M556 were also investigated for the treatment of proteinase K. As the bap-isogenic mutant M556 harbours functional ica operon, biofilm development of the strain is essentially Bap-independent and probably dependent on PIA. We conjecture that the observed difference in dispersion of both the S. aureus strains upon proteinase K treatment is due to the different constituents of biofilm matrix. V329 biofilm matrix is dominated by Bap proteins, whereas M556 biofilm (48 h) matrix is mainly composed of PIA; hence, proteinase K had no effect. The potential application of this study denotes that proteinase K can be used in biofilm dispersion as well as for anti-biofilm activity. However, proteinase K treatment showed significant removal of biofilm (Figure 3), but 100% removal could not be accomplished even after 24 h of treatment. The enzyme’s ability to trigger the dispersal in Bap-expressing S. aureus reflects its potential use in combination with antibiotics. Hence, three different antibiotics were investigated to test whether proteinase K might have a synergistic effect on antibiotic-mediated killing. It is an established fact that biofilm cells are extremely (1000 times or more) resistant to antibiotics as compared with planktonic cells.31 There are physical as well as genetical basis for the enhanced antimicrobial resistance in biofilm mode.31, 32 Biofilm control results indicated that proteinase K treatment increased the susceptibility of bacterial cells towards antibiotic treatment. The CSLM data analysis by COMSTAT (Figure 6 and Supplementary Table 1) showed that proteinase K treatment increased the surface to volume ratio and roughness coefficient of the V329 biofilm. If the surface to biovolume ratio and the roughness coefficient is more, it indicates that a high fraction of cells in the biofilm are exposed to the bulk liquid and, consequently, to dissolved antimicrobial agents.28 Thus, the enhanced values of surface to biovolume ratio and roughness coefficient after proteinase K treatments signify that more biofilm surface becomes available for antibiotics action. In general, biofilm forms a physical barrier, limiting diffusion of antibiotics and thereby reducing its efficacy.31, 33, 34 COMSTAT analysis showed that proteinase K treatment significantly decreased the average diffusion distance as well as the maximum diffusion distance. This enables the antibiotics to penetrate deep inside the biofilm and kill the cells. Thus, it can be inferred that proteinase K shows synergistic effect when associated with antibiotics for biofilm removal.
This study concludes that proteolytic degradation of the Bap-mediated biofilm matrix could be a promising therapeutic approach in controlling infections involving S. aureus. However, in other S. aureus strains in which PIA, rather than surface protein, has a major role in adhesion, this approach will not be useful. There is need to study the effect of a mixture of degradative enzymes on various components of biofilm matrix. Moreover, for therapeutic purposes, detailed clinical studies on biofilm dispersion using animal models are needed.
References
Stoodley, P., Sauer, K., Davies, D. G. & Costerton, J. W. Biofilms as complex differentiated communities. Annu. Rev. Microbiol. 56, 187–209 (2002).
Flemming, H. C. & Wingender, J. The biofilm matrix. Nat. Rev. Microbiol. 8, 623–633 (2010).
O’Toole, G., Kaplan, H. B. & Kolter, R. Biofilm formation as microbial development. Annu. Rev. Microbiol. 54, 49–79 (2000).
Gotz, F. Staphylococcus and biofilms. Mol. Microbiol. 43, 1367–1378 (2002).
Parsek, M. R. & Singh, P. K. Bacterial biofilms: an emerging link to disease pathogenesis. Annu. Rev. Microbiol. 57, 677–701 (2003).
del Pozo, J. L. & Patel, R. The challenge of treating biofilm-associated bacterial infections. Clin. Pharmacol. Ther. 82, 204–209 (2007).
Boles, B. R. & Horswill, A. R. Staphylococcal biofilm disassembly. Trends Microbiol. 19, 449–455 (2011).
Boyd, A. & Chakrabarty, A. M. Role of alginate lyase in cell detachment of Pseudomonas aeruginosa. Appl. Environ. Microbiol. 60, 2355–2359 (1994).
Kaplan, J. B., Ragunath, C., Ramasubbu, N. & Fine, D. H. Detachment of Actinobacillus actinomycetemcomitans biofilm cells by an endogenous beta-hexosaminidase activity. J. Bacteriol. 185, 4693–4698 (2003).
Kiedrowski, M. R. & Horswill, A. R. New approaches for treating staphylococcal biofilm infections. Ann. N. Y. Acad. Sci. 104–121 (2011).
Romero, D. & Kolter, R. Will biofilm disassembly agents make it to market? Trends Microbiol. 19, 304–306 (2011).
Boles, B. & Horswill, A. Agr-mediated dispersal of Staphylococcus aureus biofilms. Plos Pathog. 4, e1000052 (2008).
Merino, N. et al. Protein A-mediated multicellular behavior in Staphylococcus aureus. J. Bacteriol. 191, 832–843 (2009).
Cucarella, C. et al. Bap, a Staphylococcus aureus surface protein involved in biofilm formation. J. Bacteriol. 183, 2888–2896 (2001).
Tormo, M. A., Knecht, E., Gotz, F., Lasa, I. & Penades, J. R. Bap-dependent biofilm formation by pathogenic species of Staphylococcus: evidence of horizontal gene transfer? Microbiology. 151, 2465–2475 (2005).
O’Gara, J. P. Ica and beyond: biofilm mechanisms and regulation in Staphylococcus epidermidis and Staphylococcus aureus. FEMS Microbiol. Lett. 270, 179–188 (2007).
Vautor, E., Abadie, G., Pont, A. & Thiery, R. Evaluation of the presence of the bap gene in Staphylococcus aureus isolates recovered from human and animals species. Vet. Microbiol. 127, 407–411 (2008).
Potter, A. et al. The gene bap, involved in biofilm production, is present in Staphylococcus spp. strains from nosocomial infections. J. Microbiol. 47, 319–326 (2009).
Hennig, S., Nyunt Wai, S. & Ziebuhr, W. Spontaneous switch to PIA-independent biofilm formation in an ica-positive Staphylococcus epidermidis isolate. Int. J. Med. Microbiol. 297, 117–122 (2007).
Dubin, G. Extracellular proteases of Staphylococcus spp. Biol. Chem. 383, 1075–1086 (2002).
Shaw, L., Golonka, E., Potempa, J. & Foster, S. J. The role and regulation of the extracellular proteases of Staphylococcus aureus. Microbiology. 150, 217–228 (2004).
Kristjansson, M. M., Magnusson, O. T., Gudmundsson, H. M., Alfredsson, G. A. & Matsuzawa, H. Properties of a subtilisin-like proteinase from a psychrotrophic Vibrio species comparison with proteinase K and aqualysin I. Eur. J. Biochem. 260, 752–760 (1999).
Chaignon, P. et al. Susceptibility of staphylococcal biofilms to enzymatic treatments depends on their chemical composition. Appl. Microbiol. Biotechnol. 75, 125–132 (2007).
Alanis, A. J. Resistance to antibiotics: are we in the post-antibiotic era? Arch. Med. Res 36, 697–705 (2005).
Soderblom, T. et al. Alarming spread of vancomycin resistant enterococci in Sweden since 2007. Euro. Surveill. 15, 19620 (2010).
Hryniewicz, W. Antibiotic resistance--what we have to do now? Pol. Merkur. Lekarski 30, 305–309 (2011).
O’Toole, G. A. & Kolter, R. Initiation of biofilm formation in Pseudomonas fluorescens WCS365 proceeds via multiple, convergent signalling pathways: a genetic analysis. Mol. Microbiol. 28, 449–461 (1998).
Stepanovic, S., Vukovic, D., Jezek, P., Pavlovic, M. & Svabic-Vlahovic, M. Influence of dynamic conditions on biofilm formation by staphylococci. Eur. J. Clin. Microbiol. Infect. Dis. 20, 502–504 (2001).
Heydorn, A. et al. Quantification of biofilm structures by the novel computer program COMSTAT. Microbiology 146, 2395–2407 (2000).
Villalonga, M. L., Reyes, G. & Villalonga, R. Metal-induced stabilization of trypsin modified with alpha-oxoglutaric acid. Biotechnol. Lett. 26, 209–212 (2004).
Hoyle, B. D. & Costerton, J. W. Bacterial resistance to antibiotics: the role of biofilms. Prog. Drug. Res. 37, 91–105 (1991).
Mah, T. F. et al. A genetic basis for Pseudomonas aeruginosa biofilm antibiotic resistance. Nature 426, 306–310 (2003).
Hoyle, B. D., Alcantara, J. & Costerton, J. W. Pseudomonas aeruginosa biofilm as a diffusion barrier to piperacillin. Antimicrob. Agents. Chemother. 36, 2054–2056 (1992).
Singh, R., Ray, P., Das, A. & Sharma, M. Penetration of antibiotics through Staphylococcus aureus and Staphylococcus epidermidis biofilms. J. Antimicrob. Chemother. 65, 1955–1958 (2010).
Acknowledgements
We are grateful to Professor Inigo Lasa, Institute of Agro-Biotechnology, Spain, and Dr José R Penadés, Universidad Cardenal Herrera-CEU, Moncada, Spain, for providing bap-positive S. aureus V329 and bap-isogenic mutant M556 strains, respectively. We also thank Dr VP Venugopalan for helpful discussion and suggestions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on The Journal of Antibiotics website
Supplementary information
Rights and permissions
About this article
Cite this article
Kumar Shukla, S., Rao, T. Dispersal of Bap-mediated Staphylococcus aureus biofilm by proteinase K. J Antibiot 66, 55–60 (2013). https://doi.org/10.1038/ja.2012.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2012.98
Keywords
This article is cited by
-
Using next generation antimicrobials to target the mechanisms of infection
npj Antimicrobials and Resistance (2023)
-
Optimized sample buffer for dispersed, high-resolution capillary zone electrophoretic separation of Escherichia coli B
Scientific Reports (2023)
-
Extracellular matrix-degrading enzymes as a biofilm control strategy for food-related microorganisms
Food Science and Biotechnology (2023)
-
Responsive Polymeric Nanoparticles for Biofilm-infection Control
Chinese Journal of Polymer Science (2021)
-
Synergistic anti-biofilm effects of Brassicaceae plant extracts in combination with proteinase K against Escherichia coli O157:H7
Scientific Reports (2020)