Abstract
Linezolid is an important therapeutic option for infections from multi-drug resistant Gram-positive pathogens. However, prolonged linezolid treatment (>14 days) is considered to increase the risk of hematological adverse events. We aimed to evaluate the hematological safety profile of an i.v. single dose of linezolid in healthy volunteers of different body weight. We conducted a phase I clinical trial involving 20 healthy male Chinese volunteers that received an i.v. single dose of linezolid (600 mg). The study participants were assigned to two groups: low-weight (LW) group: 50 kg ⩽55 kg and high-weight (HW) group: ⩾80 kg. A significant decrease in the hemoglobin (Hb) levels and red blood cell (RBC) count was observed at the end of administration of the study drug in both groups. White blood cell (WBC) count was simultaneously decreased in the HW group. In the LW group, Hb levels and RBC count were also significantly decreased at 5, 7 and 24 h. In the HW group, both values were significantly decreased at 5 h. At 48 h all values were normal. The observed decreases were numerically higher in the LW group compared with the HW group. Yet, no statistical significance was noted. No difference was observed in the platelet count in both the groups. Our findings suggest that linezolid-associated hematological toxicity may also occur shortly after the i.v. administration of the drug in both LW and HW healthy volunteers. Early initiated continuous monitoring of hematological values and linezolid dosage adjustment for body weight are recommended.
Similar content being viewed by others
Introduction
Linezolid, the first commercially available representative of the antibiotic class of oxazolidinones, is considered as an important therapeutic option for infections caused from multi-drug resistant Gram-positive pathogens. Specifically, linezolid is highly active against methicillin-resistant Staphylococcus aureus, vancomycin-intermediate resistant and vancomycin-resistant S. aureus, and vancomycin-resistant Enterococci.1
Linezolid is generally well tolerated. It is mainly associated with mild gastrointestinal adverse events (AEs) (nausea, vomiting and diarrhea), headaches and fever.1 However, linezolid use, particularly prolonged linezolid courses (>14 days), has been associated with hematological AEs, including anemia, leucopenia, thrombocytopenia or even pancytopenia.2, 3, 4 Reversible myelosuppression and immune-mediated toxicity have been suggested as potential explanations for this observation.3, 5, 6
In the current era, obesity seems to acquire an epidemic profile, especially in developed countries. Published evidence suggests that the outcome of infections may be associated with body mass index distribution. Specifically, obesity and morbid obesity seem to be associated with worse infection outcomes.7 In this regard, adjustment for body weight was suggested for antimicrobial dosing in adult patients.8 Linezolid is considered as a moderately lipophilic agent, thus its pharmacokinetic/pharmacodynamic aspects may be influenced by changes in body weight.9, 10 Consequently, one may also speculate that the clinical effectiveness and safety profile of linezolid may differ in patients with different body weight.
In this regard, we conducted a phase I clinical trial in order to evaluate the safety profile of single-dose linezolid administered intravenously in healthy Chinese male volunteers with differences in body weight. Additionally, we aimed to continuously and dynamically monitor any changes in blood routine tests following the administration of i.v. single-dose linezolid, which, to our knowledge, had not been evaluated in any linezolid clinical trials.
Materials and methods
This phase I trial was registered with http://www.chictr.org (ChiCTR-TRC-10001174). The trial was conducted in accordance with principles of Good Clinical Practice, and the Declaration of Helsinki and was approved by the Ethics Committee of People's Liberation Army (PLA) general hospital (20101222001). A written informed consent was obtained from all study the participants before any trial-related procedures.
Study participants
Eligible subjects were men aged between 18 and 40 years with body mass index range 18–30 kg m−2 (permissible body weight between 50 and 55 kg or ⩾80 kg). Eligible subjects were required to have a free medical history, as well as normal clinical examination/laboratory values and electrocardiogram. Subjects were excluded if any of the following criteria were met: (1) informed consent not obtained; (2) history of hemorrhagic/cardiac/nervous/ocular region abnormalities/endocrine disease; (3) history of hypersensitivity, especially to drugs or foods; (4) any known considerable clinical or laboratory abnormality; (5) history of human immunodeficiency virus or hepatitis B virus infection; (6) blood donation within a month of study enrollment or intention to donate blood during study or 1 month after the study; (7) drug, alcohol and cigarettes abuse (light smokers included (smoking index=the number of cigarettes smoked per day × smoking years, light smokers: smoking index ⩽200)); (8) intake of experimental medication within 4 months before the study enrollment; (9) intake of any prescribed or over-the-counter medicine within 3 weeks before the study enrollment; (10) consumption of alcoholic beverages 2 days before the study enrollment until the end of hospitalization; and (11) anyone that was considered as not capable of completing the study for any reason was also excluded.
Study design
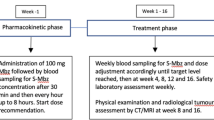
This is an open-label phase 1 study involving 20 healthy male participants. The study participants were assigned to two groups according to their body weight: low-weight group (LW): 50 kg ⩽55 kg and high-weight group (HW): body weight ⩾80 kg. The study participants were administered an i.v. single-dose of linezolid (600 mg per 30 min) at constant speed (Linezolid (600 mg per 300 ml, batch number 10C20Z47, production date: 1 March 2010, validity: 3 years, Fresenius kabi norge AS, Norway, Denmark), Pfizer Pharmaceuticals Limited, Beijing, China). To enable a proper monitoring, the study participants were hospitalized for a 7-day/6-night period starting on study day 1.
Sampling method and safety evaluation
Serial blood samples were obtained from a peripheral vein before administration of the study drug, as well as at 30 min, 5, 7, 24 and 48 h after administration. The safety profile of the study drug was evaluated by the reported AEs, as well as by scheduled physical examinations, evaluation of vital signs, 12-lead electrocardiograms and laboratory test results. Hematological AE was defined as a decrease <75% of lower limit of normal values or a decrease <50% for neutrophils, including anemia, leucopenia, thrombocytopenia or pancytopenia. Additionally, the reported AEs were evaluated in terms of major manifest, degree, turnover and drug-correlation.
Statistical analysis
The Student's t-test was used for comparisons regarding the evaluated continuous variables, whereas the χ2 test was used for comparisons regarding the evaluated dichotomous variables. A P-value <0.05 was used to denote statistical significance. The above-mentioned comparisons were performed with the SAS software v.9.1.3.
Results
Characteristics of study participants and laboratory test results
All 20 male Han Chinese participants completed the study (Figure 1). Age ranged from 18 to 37 years; mean age of the HW and LW group was 27 and 25 years, respectively. Mean body weight of the HW and LW group was 86 and 52.8 kg, respectively. The detailed results of blood testing performed at specific time points are presented in Table 1. Specifically, at the end of administration of i.v. single-dose linezolid, a significant decrease in hemoglobin (Hb) levels, white blood cell (WBC) and red blood cell (RBC) counts was observed in the HW group, whereas in the LW group a significant decrease was observed regarding Hb levels and RBC count. No difference was observed in the number of platelets in either the compared groups at the end of administration of the study drug.
Five hours following the administration of i.v. single-dose linezolid, a significant decrease in Hb levels and RBC count was observed in both the HW and LW groups. This observation was consistent at 7 and 24 h in the LW group. In the HW group, only RBC count was significantly decreased at 7 h, whereas no difference was observed regarding any of the evaluated laboratory parameters at 24 h. Finally, at 48 h, no difference was observed in either the compared groups regarding the evaluated laboratory parameters.
The decrease in Hb levels, RBC and PLt counts was numerically greater in the LW group compared with the HW group (Figures 2a and b); no statistical difference was observed. This observation was not consistent with regard to the WBC count (Figure 2b).
Changes in RBC, HB, WBC, PLt following administration of an i.v. single dose of linezolid (600 mg per 30 min at constant speed) in LW and HW group. (a) RBC and HB. (b) WBC and PLt. HB, hemoglobin; HW, high-weight group; LW, low-weight group; PLt, platelet; RBC, red blood cell; WBC, white blood cell. A full color version of this figure is available at The Journal of Antibiotics journal online.
Safety evaluation
Single doses of linezolid were generally well tolerated throughout the study. Specifically, one participant in the HW group developed fever (highest temperature reached: 38.5 °C) 24 h after administration of linezolid single-dose. The temperature returned to normal at 48 h without treatment. The participant was in good condition and continued the study protocol at 72 h. According to the attending physician, this specific AE was considered as not related to the study drug. No hematological AE was observed. No other AEs occurred during the study. No serious AEs leading to study withdrawals occurred.
Discussion
The main finding of our phase I study is that a significant decrease in the Hb levels and RBC count was observed at the end of administration of an i.v. single dose of linezolid (600 mg) in both groups of HW and LW healthy Chinese male volunteers. Particularly, in the HW group, a significant decrease in the WBC count was observed simultaneously. Five hours following linezolid administration, the Hb levels and RBC count remained significantly decreased in both groups. This observation was consistent at the 7 and 24 h-follow up assessment in the LW group, whereas in the HW group, only RBC count was decreased at the 7 h- follow up assessment.
Forty-eight hours after linezolid administration all evaluated hematological laboratory parameters were normal in both groups. Moreover, the observed decrease in Hb levels, RBC was numerically greater in the LW group compared with the HW group. However, no statistical difference was observed. Notably, no significant decrease in the PLt count was observed at any time during the study in either the compared groups. With regard to the safety profile of linezolid, the only AE reported was a case of fever in a HW-volunteer, which was not considered as related to the study drug.
Linezolid, the first oxazolidinone, was approved by the FDA in 2001 for the treatment of infections caused by Gram-positive bacteria, including multi-drug resistant Staphylococci and Enterococci. As a new class of antimicrobials, studies on the safety and tolerability of linezolid are of particular importance. Among its various AEs, hematologic toxicity including thrombocytopenia, anemia, hematocytopenia merits particular consideration.
A previous phase I study of single- and multiple-dose oral or i.v. linezolid reported no changes in red or white cell parameters, including Hb, hematocrit and RBC count. Only some of the study participants in the highest dose group of multiple doses (625 mg, 14 days of multiple oral dosing twice daily) had decreased platelet counts and percent reticulocytes.11 Additionally, other studies, including phase III and clinical studies after the drug was released to the market, reported toxicity of linezolid in the hematological system.12, 13, 14 Moreover, the above-mentioned studies pointed out that prolonged linezolid treatment (longer than two weeks) and pre-existing myelosuppression are the main factors potentially accounting for the observed hematological AEs. Notably, in the above-mentioned clinical studies, blood testing was performed daily; however, the exact time of testing was not reported.
Our phase I clinical trial is the first, to the best of our knowledge, conducting continuous dynamic monitoring of blood routine tests. Compared with the previous studies, a reduction of Hb and RBC was observed at the end of administration, when the highest plasma concentration of linezolid was achieved. In this regard, we speculate that linezolid-associated hematological toxicity may also occur as an immediate reaction.
Currently, there are two explanations for linezolid-associated hematocytopenia: bone marrow suppression15 and immune-mediated mechanism.5 Taking into account that peripheral blood cells were reduced in such short term (30 min) in our study, we consider as less likely that this is a result of bone marrow suppression. Yet, further research is needed to find the real mechanism. Specific limitations need also to be considered in the interpretation of the findings of this study. Specifically, as the blood volume is correlated to the total body weight, one may consider that the finding that the fall in Hb and RBC when infused over 30 min with 300 ml of fluid was higher in the LW group compared with the HW group is not a surprise. Moreover, one should also consider the inherent limitations the non-comparative design of this study in the interpretation as well as the extrapolation of its findings. Moreover, one may also speculate that as the evaluated hematological indexes could not be fully recovered after a dosage regimen of 600 mg per 12 h, thrombocytopenia, anemia, leukopenia or even pancytopenia may be also observed after multiple-dose of linezolid.
In conclusion, the findings of this phase I clinical trial involving healthy volunteers of different body weight suggest that the hematological toxicity of linezolid may also occur shortly after the administration of i.v. linezolid. In this regard, early initiated and continuous monitoring of complete blood counts is suggested for patients with risk factors predisposing for hematological toxicity, as well as for otherwise healthy individuals. Moreover, the degree of linezolid-associated hematological toxicity may differ between patients with different body weight, thus intensifying the need for linezolid dosage adjustment with regard to this parameter. Yet, larger studies with a comparative design are required in order to further enlighten this issue.
References
Falagas, M. E. & Vardakas, K. Z. Benefit-risk assessment of linezolid for serious Gram-positive bacterial infections. Drug Saf. 31, 753–768 (2008).
Minson, Q. & Gentry, C. A. Analysis of linezolid-associated hematologic toxicities in a large veterans affairs medical center. Pharmacotherapy 30, 895–903 (2010).
Pascoalinho, D., Vilas, M. J., Coelho, L. & Moreira, P. Linezolid-related immune-mediated severe thrombocytopenia. Int. J. Antimicrob. Agents 37, 88–89 (2011).
Tsuji, Y. et al. Thrombocytopenia and anemia caused by a persistent high linezolid concentration in patients with renal dysfunction. J. Infect. Chemother. 17, 70–75 (2010).
Bernstein, W. B., Trotta, R. F., Rector, J. T., Tjaden, J. A. & Barile, A. J. Mechanisms for linezolid-induced anemia and thrombocytopenia. Ann. Pharmacother. 37, 517–520 (2003).
Green, S. L., Maddox, J. C. & Huttenbach, E. D. Linezolid and reversible myelosuppression. JAMA 285, 1291 (2001).
Falagas, M. E., Athanasoulia, A. P., Peppas, G. & Karageorgopoulos, D. E. Effect of body mass index on the outcome of infections: a systematic review. Obes. Rev. 10, 280–289 (2009).
Falagas, M. E. & Karageorgopoulos, D. E. Adjustment of dosing of antimicrobial agents for bodyweight in adults. Lancet 375, 248–251 (2010).
Mersfelder, T. L. & Smith, C. L. Linezolid pharmacokinetics in an obese patient. Am. J. Health Syst. Pharm. 62, 464–467 (2005).
Stein, G. E. et al. Pharmacokinetics and pharmacodynamics of linezolid in obese patients with cellulitis. Ann. Pharmacother. 39, 427–432 (2005).
Stalker, D. J., Jungbluth, G. L., Hopkins, N. K. & Batts, D. H. Pharmacokinetics and tolerance of single- and multiple-dose oral or intravenous linezolid, an oxazolidinone antibiotic, in healthy volunteers. J. Antimicrob. Chemother. 51, 1239–1246 (2003).
Soriano, A. et al. Efficacy and tolerability of prolonged linezolid therapy in the treatment of orthopedic implant infections. Eur. J. Clin. Microbiol. Infect. Dis. 26, 353–356 (2007).
Wu, V. C. et al. High frequency of linezolid-associated thrombocytopenia and anemia among patients with end-stage renal disease. Clin. Infect. Dis. 42, 66–72 (2006).
Birmingham, M. C. et al. Linezolid for the treatment of multidrug-resistant, Gram-positive infections: experience from a compassionate-use program. Clin. Infect. Dis. 36, 159–168 (2003).
Lawyer, M. C. & Lawyer, E. Z. Linezolid and reversible myelosuppression. JAMA 286, 1974 (2001).
Acknowledgements
This study was supported by Grant 81000755 from the National Natural Science Foundation of China and 2010B079 from Beijing Science and Technology New Star Program of China. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author contributions: Yun Cai, Dong Chai and Rui Wang contributed in study design, clinical trial and writing of this study. Daihong Guo, Nan Bai and Beibei Liang contributed in the clinical trial. Matthew E Falagas, Evridiki K Vouloumanou and Youning Liu contributed in study design and writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cai, Y., Chai, D., Falagas, M. et al. Immediate hematological toxicity of linezolid in healthy volunteers with different body weight: a phase I clinical trial. J Antibiot 65, 175–178 (2012). https://doi.org/10.1038/ja.2011.142
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2011.142