Abstract
Background and objective:
The sequence of prenatal growth restraint and postnatal catch-up growth may lead to hepato-visceral adiposity, insulin resistance and low-grade inflammation before the onset of puberty. In prepubertal children born appropriate for gestational age (AGA) or small for gestational age (SGA), we assessed potential relationships between the aforementioned sequence and liver volume.
Subjects/Methods:
The study population consisted of 86 children (41 AGA and 45 SGA with catch-up growth; age (mean±s.e.m.), 8.5±0.1 years), recruited into two prospective longitudinal studies. Anthropometry, endocrine–metabolic variables and inflammatory and hepatic markers were assessed, along with liver volume, hepatic adiposity and abdominal fat partitioning (by magnetic resonance imaging).
Results:
AGA and SGA children differed in hepato-visceral adiposity, but had similar liver volumes. Boys had larger livers than girls, and higher sex hormone binding globulin and inflammation markers. Liver volume correlated with height Z-score, body mass index Z-score, HOMA-IR (homeostasis model assessment-insulin resistance) and with subcutaneous and visceral fat, but not with birth weight Z-score or with hepatic adiposity. Height, visceral fat, gender and HOMA-IR were major determinants of liver volume, together explaining 61% of its variance.
Conclusions:
The trajectory from prenatal restraint, via postnatal catch-up, to hepato-visceral adiposity and insulin resistance does not appear to be detectably influenced by prepubertal alterations of liver volume. Further follow-up will disclose the potential role of liver volume in the pubertal segment of this trajectory, and whether the augmented fat content and visceral adiposity in SGA subjects is followed by the development of metabolic syndrome and hepatic dysfunction in adulthood.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM . Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced foetal growth. Diabetologia 1993; 36: 62–67.
Ibáñez L, Ong K, Dunger D, de Zegher F . Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational age children. J Clin Endocrinol Metab 2006; 91: 2153–2158.
Ibáñez L, Suárez L, Lopez-Bermejo A, Díaz M, Valls C, de Zegher F . Early development of visceral fat excess after spontaneous catch-up growth in children with low birth weight. J Clin Endocrinol Metab 2008; 93: 2079–2083.
Sebastiani G, Díaz M, Bassols J, Aragonés G, López-Bermejo A, de Zegher F et al. The sequence of prenatal growth restraint and post-natal catch-up growth leads to a thicker intima-media and more pre-peritoneal and hepatic fat by age 3-6 years. Pediatr Obes 2016; 11: 251–257.
Ibáñez L, López-Bermejo A, Díaz M, Marcos MV, Casano P, de Zegher F . Abdominal fat partitioning and high-molecular-weight adiponectin in short children born small for gestational age. J Clin Endocrinol Metab 2009; 94: 1049–1052.
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A . The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS One 2015; 10: e0140908.
Eckel RH, Grundy SM, Zimmet PZ . The metabolic syndrome. Lancet 2005; 365: 1415–1428.
Nobili V, Marcellini M, Marchesini G, Vanni E, Manco M, Villani A et al. Intrauterine growth retardation, insulin resistance, and nonalcoholic fatty liver disease in children. Diabetes Care 2007; 30: 2638–2640.
Faienza MF, Brunetti G, Ventura A, D’Aniello M, Pepe T, Giordano P et al. Nonalcoholic fatty liver disease in prepubertal children born small for gestational age: influence of rapid weight catch-up growth. Horm Res Paediatr 2013; 79: 103–109.
Alisi A, Cianfarani S, Manco M, Agostoni C, Nobili V . Non-alcoholic fatty liver disease and metabolic syndrome in adolescents: pathogenic role of genetic background and intrauterine environment. Ann Med 2012; 44: 29–40.
Fraser A, Ebrahim S, Smith GD, Lawlor DA . The associations between birthweight and adult markers of liver damage and function. Paediatr Perinat Epidemiol 2008; 22: 92–99.
Simpson J, Smith AD, Fraser A, Sattar N, Callaway M, Lindsay RS et al. Cord blood adipokines and lipids and adolescent nonalcoholic fatty liver disease. J Clin Endocrinol Metab 2016; 101: 4661–4668.
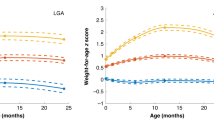
Anderson EL, Howe LD, Fraser A, Callaway MP, Sattar N, Day C et al. Weight trajectories through infancy and childhood and risk of non-alcoholic fatty liver disease in adolescence: The ALSPAC study. J Hepatol 2014; 61: 626–632.
Ayonrinde OT, Olynyk JK, Marsh JA, Beilin LJ, Mori TA, Oddy WH et al. Childhood adiposity trajectories and risk of non-alcoholic fatty liver disease in adolescents. Hepatology 2015; 30: 163–171.
Harville EW, Chen W, Bazzano L, Oikonen M, Hutri-Kähönen N, Raitakari O . Indicators of fetal growth and adult liver enzymes: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. J Dev Orig Health Dis 2017; 8: 226–235.
de Zegher F, Sebastiani G, Diaz M, Sánchez-Infantes D, Lopez-Bermejo A, Ibáñez L . Body composition and circulating high-molecular-weight adiponectin and IGF-I in infants born small for gestational age: breast- versus formula-feeding. Diabetes 2012; 61: 1969–1973.
Ferrández-Longas A, Mayayo E, Labarta JI, Bagué L, Puga B, Rueda C et al. Estudio longitudinal de crecimiento y desarrollo. Centro Andrea Prader. Zaragoza 1980-2002. In: Garcia-Dihinx A, Romo A, Ferrandez-Longas A (eds). Patrones de crecimiento y desarrollo en España. Ergon: Madrid, Spain, 2004; pp 61–115.
Tanner JM, Whitehouse RH . Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child 1976; 51: 170–179.
Larrabide I, Omedas P, Martelli Y, Planes X, Nieber M, Moya JA et al. GIMIAS: an open source framework for efficient development of research tools and clinical prototypesIn: Ayache N, Delingette H, Sermesant M (eds) Functional Imaging and Modeling of the Heart, Lecture Notes in Computer Science. Springer: Berlin, Heidelberg, 2009; vol. 5528, pp 7–426.
Beutler E, Demina A, Laubscher K, Garver P, Gelbart T, Balicki D et al. The clinical course of treated and untreated Gaucher disease. A study of 45 patients. Blood Cells Mol Dis 1995; 21: 86–108.
Latini G, De Mitri B, Del Vecchio A, Chitano G, De Felice C, Zetterström R . Foetal growth of kidneys, liver and spleen in intrauterine growth restriction: ‘programming’ causing ‘metabolic syndrome’ in adult age. Acta Paediatr 2004; 93: 1635–1639.
van der Poorten D, Milner KL, Hui J, Hodge A, Trenell MI, Kench JG et al. Visceral fat: a key mediator of steatohepatitis in metabolic liver disease. Hepatology 2008; 48: 449–457.
Gyllenhammer LE, Alderete TL, Toledo-Corral CM, Weigensberg M, Goran MI . Saturation of subcutaneous adipose tissue expansion and accumulation of ectopic fat associated with metabolic dysfunction during late and post-pubertal growth. Int J Obes 2016; 40: 601–606.
Konuş OL, Ozdemir A, Akkaya A, Erbaş G, Celik H, Işik S . Normal liver, spleen, and kidney dimensions in neonates, infants, and children: evaluation with sonography. AJR Am J Roentgenol 1998; 171: 1693–1698.
Busetto L, Tregnaghi A, De Marchi F, Segato G, Foletto M, Sergi G et al. Liver volume and visceral obesity in women with hepatic steatosis undergoing gastric banding. Obes Res 2002; 10: 408–411.
Santini F, Giannetti M, Mazzeo S, Fierabracci P, Scartabelli G, Marsili A et al. Ultrasonographic evaluation of liver volume and the metabolic syndrome in obese women. J Endocrinol Invest 2007; 30: 104–110.
Giannetti M, Piaggi P, Ceccarini G, Mazzeo S, Querci G, Fierabracci P et al. Hepatic left lobe volume is a sensitive index of metabolic improvement in obese women after gastric banding. Int J Obes (Lond) 2012; 36: 336–341.
Edholm D, Kullberg J, Karlsson FA, Haenni A, Ahlström H, Sundbom M . Changes in liver volume and body composition during 4 weeks of low calorie diet before laparoscopic gastric bypass. Surg Obes Relat Dis 2015; 11: 602–606.
Lesmana CR, Hasan I, Budihusodo U, Gani RA, Krisnuhoni E, Akbar N et al. Diagnostic value of a group of biochemical markers of liver fibrosis in patients with non-alcoholic steatohepatitis. J Dig Dis 2009; 10: 201–206.
Crespo J, Cayón A, Fernández-Gil P, Hernandez-Guerra M, Mayorga M, Domínguez-Díez A et al. Gene expression of tumour necrosis factor alpha and TNF-receptors, p55 and p75, in nonalcoholic steatohepatitis patients. Hepatology 2001; 34: 1158–1163.
Valenti L, Fracanzani AL, Dongiovanni P, Santorelli G, Branchi A, Taioli E et al. Tumor necrosis factor alpha promoter polymorphisms and insulin resistance in nonalcoholic fatty liver disease. Gastroenterology 2002; 122: 274–280.
Haukeland JW, Damås JK, Konopski Z, Løberg EM, Haaland T, Goverud I et al. Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J Hepatol 2006; 44: 1167–1174.
Westerbacka J, Kolak M, Kiviluoto T, Arkkila P, Sirén J, Hamsten A et al. Genes involved in fatty acid partitioning and binding, lipolysis, monocyte/macrophage recruitment, and inflammation are overexpressed in the human fatty liver of insulin-resistant subjects. Diabetes 2007; 56: 2759–2765.
Moran JR, Ghishan FK, Halter SA, Greene HL . Steatohepatitis in obese children: a cause of chronic liver dysfunction. Am J Gastroenterol 1983; 78: 374–377.
Baldridge AD, Perez-Atayde AR, Graeme-Cook F, Higgins L, Lavine JE . Idiopathic steatohepatitis in childhood: a multicenter retrospective study. J Pediatr 1995; 127: 700–704.
Manton ND, Lipsett J, Moore DJ, Davidson GP, Bourne AJ, Couper RT . Non-alcoholic steatohepatitis in children and adolescents. Med J Aust 2000; 173: 476–479.
Rashid M, Roberts EA . Nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr 2000; 30: 48–53.
Schwimmer JB, Deutsch R, Rauch JB, Behling C, Newbury R, Lavine JE . Obesity, insulin resistance, and other clinicopathological correlates of pediatric nonalcoholic fatty liver disease. J Pediatr 2003; 143: 500–505.
Schwimmer JB, McGreal N, Deutsch R, Finegold MJ, Lavine JE . Influence of gender, race, and ethnicity on suspected fatty liver in obese adolescents. Pediatrics 2005; 115: e561–e565.
Sabir N, Sermez Y, Kazil S, Zencir M . Correlation of abdominal fat accumulation and liver steatosis: importance of ultrasonographic and anthropometric measurements. Eur J Ultrasound 2001; 14: 121–128.
Nguyen-Duy TB, Nichaman MZ, Church TS, Blair SN, Ross R . Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Am J Physiol Endocrinol Metab 2003; 284: E1065–E1071.
Stranges S, Dorn JM, Muti P, Freudenheim JL, Farinaro E, Russell M et al. Body fat distribution, relative weight, and liver enzyme levels: a population-based study. Hepatology 2004; 39: 754–763.
Donnelly KI, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ . Sources of fatty acids stored in the liver and secreted with lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest 2005; 115: 1343–1351.
Hamdy O, Porramatikul S, Al-Ozairi E . Metabolic obesity: the paradox between visceral and subcutaneous fat. Curr Diabetes Rev 2006; 2: 367–373.
Sorensen K, Andesson AM, Skakkebaek NE, Juul A . Serum sex hormone-binding globulin levels in healthy children and girls with precocious puberty before and during gonatropin-releasing hormone agonist treatment. J Clin Endocrinol Metab 2007; 92: 3189–3196.
Persson I, Ahlsson F, Ewald U, Tuvemo T, Qingyuan M, von Rosen D et al. Influence of perinatal factors on the onset of puberty in boys and girls: implications for interpretation of link with risk of long term diseases. Am J Epidemiol 1999; 150: 747–755.
Permutt Z, Le TA, Peterson MR, Seki E, Brenner DA, Sirlin C et al. Correlation between liver histology and novel magnetic resonance imaging in adult patients with non-alcoholic fatty liver disease - MRI accurately quantifies hepatic steatosis in NAFLD. Aliment Pharmacol Ther 2012; 36: 22–29.
Dulai PS, Sirlin CB, Loomba R . MRI and MRE for non-invasive quantitative assessment of hepatic steatosis and fibrosis in NAFLD and NASH: clinical trials to clinical practice. J Hepatol 2016; 65: 1006–1016.
Lin SC, Heba E, Bettencourt R, Lin GY, Valasek MA, Lunde O . Assessment of treatment response in non-alcoholic steatohepatitis using advanced magnetic resonance imaging. Aliment Pharmacol Ther 2017; 45: 844–854.
Acknowledgements
LI, RM and MD are investigators of CIBERDEM (www.ciberdem.org). AL-B is an investigator of the I3 Fund for Scientific research (Ministry of Education and Science, Spain). JB is an investigator of the Miguel Servet Fund from Carlos III National Institute of Health, Spain (MS12/03239).
Author contributions
LI and AL-B had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Malpique, R., Bassols, J., López-Bermejo, A. et al. Liver volume and hepatic adiposity in childhood: relations to body growth and visceral fat. Int J Obes 42, 65–71 (2018). https://doi.org/10.1038/ijo.2017.198
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.198
This article is cited by
-
Catch-up growth in juvenile rats, fat expansion, and dysregulation of visceral adipose tissue
Pediatric Research (2022)
-
Brown adipose tissue in prepubertal children: associations with sex, birthweight, and metabolic profile
International Journal of Obesity (2019)