Abstract
Background:
Bariatric surgery remains the most effective treatment for reducing adiposity and eliminating type 2 diabetes; however, the mechanism(s) responsible have remained elusive. Peroxisome proliferator-activated receptors (PPAR) encompass a family of nuclear hormone receptors that upon activation exert control of lipid metabolism, glucose regulation and inflammation. Their role in adipose tissue following bariatric surgery remains undefined.
Materials and Methods:
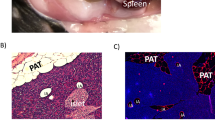
Subcutaneous adipose tissue biopsies and serum were obtained and evaluated from time of surgery and on postoperative day 7 in patients randomized to Roux-en-Y gastric bypass (n=13) or matched caloric restriction (n=14), as well as patients undergoing vertical sleeve gastrectomy (n=33). Fat samples were evaluated for changes in gene expression, protein levels, β-oxidation, lipolysis and cysteine oxidation.
Results:
Within 7 days, bariatric surgery acutely drives a change in the activity and expression of PPARγ and PPARδ in subcutaneous adipose tissue thereby attenuating lipid storage, increasing lipolysis and potentiating lipid oxidation. This unique metabolic alteration leads to changes in downstream PPARγ/δ targets including decreased expression of fatty acid binding protein (FABP) 4 and stearoyl-CoA desaturase-1 (SCD1) with increased expression of carnitine palmitoyl transferase 1 (CPT1) and uncoupling protein 2 (UCP2). Increased expression of UCP2 not only facilitated fatty acid oxidation (increased 15-fold following surgery) but also regulated the subcutaneous adipose tissue redoxome by attenuating protein cysteine oxidation and reducing oxidative stress. The expression of UCP1, a mitochondrial protein responsible for the regulation of fatty acid oxidation and thermogenesis in beige and brown fat, was unaltered following surgery.
Conclusions:
These results suggest that bariatric surgery initiates a novel metabolic shift in subcutaneous adipose tissue to oxidize fatty acids independently from the beiging process through regulation of PPAR isoforms. Further studies are required to understand the contribution of this shift in expression of PPAR isoforms to weight loss following bariatric surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
International Diabetes Federation (IDF) IDF Diabetes Atlas, 7th edn. idf.org, 2015 doi:10.1289/image.ehp.v119.i03.
Statements P. Standards of medical care in diabetes—2012. Diabetes Care 2012; 35: S11–S63.
Ikramuddin S, Korner J, Lee W-J, Connett JE, Inabnet Iii WB, Billington CJ et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: The Diabetes Surgery Study Randomized Clinical Trial. JAMA 2013; 309: 2240–2249.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer Sa, Navaneethan SD et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med 2014; 370: 1–12.
Tilg H, Moschen AR . Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 2006; 6: 772–783.
Chondronikola M, Harris LLS, Klein S . Bariatric surgery and type 2 diabetes: are there weight loss-independent therapeutic effects of upper gastrointestinal bypass? J Intern Med 2016; 280: 476–486.
Chen Y, Corsino L, Shantavasinkul PC, Grant J, Portenier D, Ding L et al. Gastric bypass surgery leads to long-term remission or improvement of type 2 diabetes and significant decrease of microvascular and macrovascular complications. Ann Surg 2016; 263: 1138–1142.
Abraham A, Ikramuddin S, Jahansouz C, Arafat F, Hevelone N, Leslie D . Trends in bariatric surgery: procedure selection, revisional surgeries, and readmissions. Obes Surg 2016; 26: 1371–1377.
Gastaldelli A, Iaconelli A, Gaggini M, Magnone MC, Veneziani A, Rubino F . Short-term effects of laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass. Diabetes Care 2016; 39: 1–7.
Tam C, Berthoud H-R, Bueter M, Chakravarthy M, Geliebter A, Hajnal A et al. Could the mechanisms of bariatric surgery hold the key for novel therapies? A report from the Pennington Scientific Symposium. Obes Rev 2011; 12: 984–994.
Fuentes E, Guzmán-jofre L, Moore-carrasco R, Palomo I . Role of PPARs in inflammatory processes associated with metabolic syndrome. Mol Med Rep 2013; 8: 1611–1616.
Tontonoz P, Hu E, Graves RA, Budavari AI, Spiegelman BM . mPPARγ2: tissue-specific regulator of an adipocyte enhancer. Genes Dev 1994; 8: 1224–1234.
Wang YX, Lee CH, Tiep S, Yu RT, Ham J, Kang H et al. Peroxisome-proliferator-activated receptor delta activates fat metabolism to prevent obesity. Cell 2003; 113: 159–170.
Wagner K, Wagner N . Pharmacology & therapeutics peroxisome proliferator-activated receptor beta/delta (PPAR β/δ) acts as regulator of metabolism linked to multiple cellular functions. Pharmacol Ther 2010; 125: 423–435.
Jahansouz C, Xu H, Hertzel AV, Serrot FJ, Kvalheim N, Cole A et al. Bile acids increase independently from hypocaloric restriction after bariatric surgery. Ann Surg 2016; 264: 1022–1028.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Xu H, Hertzel AV, Steen KA, Wang Q, Suttles J, Bernlohr DA . Uncoupling lipid metabolism from inflammation through FABP-dependent expression of UCP2. Mol Cell Biol 2015; 35: 1055–1065.
Wang T, Zang Y, Ling W, Corkey BE, Guo W . Metabolic partitioning of endogenous fatty acid in adipocytes. Obes Res 2003; 11: 880–887.
Ward M, Prachand V . Surgical treatment of obesity. Gastrointest Endosc 2009; 70: 985–990.
Cock T-A, Houten SM, Auwerx J . Peroxisome proliferator-activated receptor-gamma: too much of a good thing causes harm. EMBO Rep 2004; 5: 142–147.
Miles PDG, Barak Y, He W, Evans RM, Olefsky JM . Improved insulin-sensitivity in mice heterozygous for PPAR-gamma deficiency. J Clin Invest 2000; 105: 287–292.
Yehuda-shnaidman E, Buehrer B, Pi J, Kumar N, Collins S . Acute stimulation of white adipocyte respiration by PKA-induced lipolysis. Diabetes 2010; 59: 2474–2483.
Camastra S, Gastaldelli A, Mari A, Bonuccelli S . Early and longer term effects of gastric bypass surgery on tissue-specific insulin sensitivity and beta cell function in morbidly obese patients with and without type 2 diabetes. Diabetologia 2011; 54: 2093–2102.
Hotamisligil GS, Bernlohr DA . Metabolic functions of FABPs—mechanisms and therapeutic implications. Nat Rev Endocrinol 2015; 11: 592–605.
Scheja L, Makowski L, Uysal KT, Wiesbrock SM, Shimshek DR, Meyers DS et al. Altered insulin secretion associated with reduced lipolytic efficiency in aP2(-/-) mice. Diabetes 1999; 48: 1987–1994.
Cao H, Sekiya M, Ertunc ME, Burak MF, Mayers JR, White A et al. Adipocyte lipid chaperone aP2 Is a secreted adipokine regulating hepatic glucose production. Cell Metab 2013; 17: 768–778.
Armstrong EH, Goswami D, Griffin PR, Noy N, Ortlund EA . Structural basis for ligand regulation of the fatty acid-binding protein 5, peroxisome proliferator-activated receptor β/δ (FABP5-PPARβ/δ) signaling pathway. J Biol Chem 2014; 289: 14941–14954.
Toral M, Romero M, Jiménez R, Robles-vera I, Tamargo J, Carmen M et al. Role of UCP2 in the protective effects of PPAR beta/delta activation on lipopolysaccharide-induced endothelial dysfunction. Biochem Pharmacol 2016; 110–111: 25–36.
Krauss S, Zhang CY, Lowell BB . The mitochondrial uncoupling-protein homologues. Nat Rev Mol Cell Biol 2005; 6: 248–261.
Koutsari C, Ali AH, Mundi MS, Jensen MD . Storage of circulating free fatty acid in adipose tissue of postabsorptive humans: quantitative measures and implications for body fat distribution. Diabetes 2011; 60: 2032–2040.
Merlotti C, Ceriani V, Morabito A, Pontiroli AE . Subcutaneous fat loss is greater than visceral fat loss with diet and exercise, weight-loss promoting drugs, and bariatric surgery. A critical review and meta-analysis. Int J Obes 2017; 41: 1–11.
Altshuler D, Hirschhorn JN, Klannemark M, Lindgren CM, Vohl MC, Nemesh J et al. The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 2000; 26: 76–80.
Memisoglu A, Hu FB, Hankinson SE, Manson JE, De Vivo I, Willett WC et al. Interaction between a peroxisome proliferator-activated receptor gamma gene polymorphism and dietary fat intake in relation to body mass. Hum Mol Genet 2003; 12: 2923–2929.
Fonseca V . Effect of thiazolidinediones on body weight in patients with diabetes mellitus. Am J Med 2003; 115: 42–48.
Jaworski K, Ahmadian M, Duncan RE, Sarkadi-nagy E, Varady A, Hellerstein MK et al. AdPLA ablation increases lipolysis and prevents obesity induced by high fat feeding or leptin deficiency. Nat Med 2009; 15: 159–168.
Tansey JT, Sztalryd C, Roush DL, Zee JV, Gavrilova O, Reitman ML et al. Perilipin ablation results in a lean mouse with aberrant adipocyte lipolysis, enhanced leptin production, and resistance to diet-induced obesity. Proc Natl Acad Sci USA 2001; 98: 6494–6499.
Saha PK, Kojima H, Martinez-botas J, Sunehag AL, Chan L . Metabolic adaptations in the absence of perilipin: increased beta-oxidation and decreased hepatic glucose production associated with peripheral insulin resistance but normal glucose tolerance in perilipin-null mice. J Biol Chem 2004; 279: 35150–35158.
Riserus U, Sprecher D, Johnson T, Olson E, Hirschberg S, Liu A et al. Activation of peroxisome proliferator-activated receptor (PPAR)delta promotes reversal of multiple metabolic abnormalities, reduces oxidative stress, and increases fatty acid oxidation in moderately obese men 1142. Diabetes 2008; 57: 332–339.
Hotamisligil GS, Johnson RS, Distel RJ, Ellis R, Papaioannou E, Spiegelman BM . Uncoupling of obesity from insulin resistance through a targeted mutation in aP2, the adipocyte fatty acid binding protein. Science (80-) 1996; 274: 1377–1379.
Kaess BM, Enserro DM, McManus DD, Xanthakis V, Chen MH, Sullivan LM et al. Cardiometabolic correlates and heritability of fetuin-A, retinol-binding protein 4, and fatty-acid binding protein 4 in the framingham heart study. J Clin Endocrinol Metab 2012; 97: E1943–E1947.
Cao H, Gerhold K, Mayers JR, Wiest MM, Steve M, Hotamisligil GS . Identification of a lipokine, a lipid hormone linking adipose tissue to systemic metabolism. Cell 2009; 134: 933–944.
Tuncman G, Erbay E, Hom X, De Vivo I, Campos H, Rimm EB et al. A genetic variant at the fatty acid-binding protein aP2 locus reduces the risk for hypertriglyceridemia, type 2 diabetes, and cardiovascular disease. Proc Natl Acad Sci USA 2006; 103: 6970–6975.
Gan L, Liu Z, Cao W, Zhang Z, Sun C . FABP4 reversed the regulation of leptin on mitochondrial fatty acid oxidation in mice adipocytes. Nat Publ Gr 2015; 5: 1–12.
Zorov DB, Juhaszova M, Sollott SJ . Mitochondrial reactive oxygen species (ros) and ros-induced ros release. Physiol Rev 2014; 94: 909–950.
Xu H, Hertzel AV, Steen KA, Bernlohr DA . Loss of fatty acid binding protein 4/aP2 reduces macrophage inflammation through activation of SIRT3. Mol Endocrinol 2016; 30: 325–334.
Steen KA, Xu H, Bernlohr DA . FABP4/aP2 regulates macrophage redox signaling and inflammasome activation via control of UCP2. Mol Cell Biol 2016; 37: e00282–16.
Yu X, Wieczorek S, Franke A, Yin H, Pierer M, Sina C et al. Association of UCP2–866 G/A polymorphism with chronic inflammatory diseases. Genes Immun 2009; 10: 601–605.
Esterbauer H, Schneitler C, Oberkofler H, Ebenbichler C, Paulweber B, Sandhofer F et al. A common polymorphism in the promoter of UCP2 is associated with decreased risk of obesity in middle-aged humans. Nat Genet 2001; 28: 178–183.
Vogler S, Goedde R, Miterski B, Gold R, Kroner A, Koczan D et al. Association of a common polymorphism in the promoter of UCP2 with susceptibility to multiple sclerosis. J Mol Med 2005; 83: 806–811.
de Oliveira B, de Souza Pinhel M, Nicoletti C, de Oliveira C, Quinhoneiro D, Noronha N et al. UCP2 and PLIN1 expression affects the resting metabolic rate and weight loss on obese patients. Obes Surg 2017; 27: 343–348.
Simón I, Escoté X, Vilarrasa N, Gómez J, Fernández-Real JM, Megía A et al. Adipocyte fatty acid-binding protein as a determinant of insulin sensitivity in morbid-obese women. Obesity (Silver Spring) 2009; 17: 1124–1128.
Terra X, Quintero Y, Auguet T, Porras JA, Hernandez M, Sabench F et al. FABP 4 is associated with inflammatory markers and metabolic syndrome in morbidly obese women. Eur J Endocrinol 2011; 164: 539–547.
Engl J, Ciardi C, Tatarczyk T, Kaser S, Laimer M, Laimer E et al. A-FABP—a biomarker associated with the metabolic syndrome and/or an indicator of weight change? Obesity (Silver Spring) 2008; 16: 1838–1842.
Acknowledgements
We thank the members of the Bernlohr laboratory, the University of Minnesota Department of Surgery Division of Gastrointestinal and Bariatric Surgery, the University of Minnesota Bionet Department, and the CentraCare Bariatric Center (St. Cloud, MN, USA) for their assistance during the preparation of this manuscript. This study was done using computing resources at the University of Minnesota Supercomputing Institute. This work was supported by the American Diabetes Association (ADA 7-11-ST-01), NIH DK053189 to DAB and the Minnesota Obesity Center (NIH P30DK050456).
Author contributions
CJ, HX, AVH, SI and DAB performed all experiments and data interpretation, and conceived the study design. GL, DBL and SI performed all surgeries and participated in all facets of serum and tissue collection. KE conceived dietary plan and ensured subject compliance. NK, FJS, SSK, HX and CJ collected and stored all specimens. NK, FJS, SSK and CJ performed all qRT–PCR analysis. AVH and HX performed adipose tissue fractionation, western blot, fatty acid oxidation, fatty acid and glycerol measurements. KAS measured cysteine oxidation in SAT. RF and HX measured sera FABP4. CJ, HX, AVH, SSK, SI and DAB wrote the paper.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Jahansouz, C., Xu, H., Hertzel, A. et al. Partitioning of adipose lipid metabolism by altered expression and function of PPAR isoforms after bariatric surgery. Int J Obes 42, 139–146 (2018). https://doi.org/10.1038/ijo.2017.197
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.197
This article is cited by
-
Effect of oesophagectomy on lipid profiles in patients with oesophageal cancer combined with hyperlipidaemia: a retrospective study
Lipids in Health and Disease (2024)
-
Bariatric surgery can acutely modulate ER-stress and inflammation on subcutaneous adipose tissue in non-diabetic patients with obesity
Diabetology & Metabolic Syndrome (2021)
-
Serum FABP1 Levels Correlate Positively with Obesity in Chinese Patients After Laparoscopic Sleeve Gastrectomy: a 12-Month Follow-up Study
Obesity Surgery (2020)
-
Inflammatory responses to dietary and surgical weight loss in male and female mice
Biology of Sex Differences (2019)
-
Effect of Sleeve Gastrectomy on Angiogenesis and Adipose Tissue Health in an Obese Animal Model of Type 2 Diabetes
Obesity Surgery (2019)