Abstract
Background/Objectives:
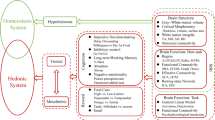
Despite the effectiveness of bariatric surgery, there is still substantial variability in long-term weight outcomes and few factors with predictive power to explain this variability. Neuroimaging may provide a novel biomarker with utility beyond other commonly used variables in bariatric surgery trials to improve prediction of long-term weight-loss outcomes. The purpose of this study was to evaluate the effects of sleeve gastrectomy (SG) on reward and cognitive control circuitry postsurgery and determine the extent to which baseline brain activity predicts weight loss at 12-month postsurgery.
Subjects/Methods:
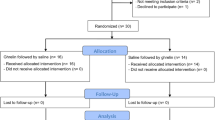
Using a longitudinal design, behavioral, hormone and neuroimaging data (during a desire for palatable food regulation paradigm) were collected from 18 patients undergoing SG at baseline (<1 month prior) and 12-month post-SG.
Results:
SG patients lost an average of 29.0% of their weight (percentage of total weight loss (%TWL)) at 12-month post-SG, with significant variability (range: 16.0–43.5%). Maladaptive eating behaviors (uncontrolled, emotional and externally cued eating) improved (P<0.01), in parallel with reductions in fasting hormones (acyl ghrelin, leptin, glucose, insulin; P<0.05). Brain activity in the nucleus accumbens (NAcc), caudate, pallidum and amygdala during desire for palatable food enhancement vs regulation decreased from baseline to 12 months (P (family-wise error (FWE))<0.05). Dorsolateral and dorsomedial prefrontal cortex activity during desire for palatable food regulation (vs enhancement) increased from baseline to 12 months (P(FWE)<0.05). Baseline activity in the NAcc and hypothalamus during desire for palatable food enhancement was significantly predictive of %TWL at 12 months (P (FWE)<0.05), superior to behavioral and hormone predictors, which did not significantly predict %TWL (P>0.10). Using stepwise linear regression, left NAcc activity accounted for 54% of the explained variance in %TWL at 12 months.
Conclusions:
Consistent with previous obesity studies, reward-related neural circuit activity may serve as an objective, relatively robust predictor of postsurgery weight loss. Replication in larger studies is necessary to determine true effect sizes for outcome prediction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC et al. Health benefits of gastric bypass surgery after 6 years. JAMA 2012; 308: 1122–1131.
Carlin AM, Zeni TM, English WJ, Hawasli AA, Genaw JA, Krause KR et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg 2013; 257: 791–797.
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 2013; 310: 2416–2425.
Ikramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013; 309: 2240–2249.
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012; 366: 1567–1576.
Sjostrom L, Peltonen M, Jacobson P, Sjostrom CD, Karason K, Wedel H et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012; 307: 56–65.
Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 2009; 361: 445–454.
Courcoulas AP, Christian NJ, O'Rourke RW, Dakin G, Patchen Dellinger E, Flum DR et al. Preoperative factors and 3-year weight change in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. Surg Obes Relat Dis 2015; 11: 1109–1118.
Courcoulas AP, Yanovski SZ, Bonds D, Eggerman TL, Horlick M, Staten MA et al. Long-term outcomes of bariatric surgery: a National Institutes of Health symposium. JAMA Surg 2014; 149: 1323–1329.
Gabrieli JD, Ghosh SS, Whitfield-Gabrieli S . Prediction as a humanitarian and pragmatic contribution from human cognitive neuroscience. Neuron 2015; 85: 11–26.
Hall PA . Prevention neuroscience: a new frontier for preventive medicine. Prev Med 2016; 86: 114–116.
Nichols TE, Das S, Eickhoff SB, Evans AC, Glatard T, Hanke M et al. Best practices in data analysis and sharing in neuroimaging using MRI. Nat Neurosci 2017; 20: 299–303.
Furey ML, Drevets WC, Hoffman EM, Frankel E, Speer AM, Zarate CA Jr . Potential of pretreatment neural activity in the visual cortex during emotional processing to predict treatment response to scopolamine in major depressive disorder. JAMA Psychiatry 2013; 70: 280–290.
Whitfield-Gabrieli S, Ghosh SS, Nieto-Castanon A, Saygin Z, Doehrmann O, Chai XJ et al. Brain connectomics predict response to treatment in social anxiety disorder. Mol Psychiatry 2016; 21: 680–685.
van Veenendaal TM, IJff DM, Aldenkamp AP, Hofman PA, Vlooswijk MC, Rouhl RP et al. Metabolic and functional MR biomarkers of antiepileptic drug effectiveness: a review. Neurosci Biobehav Rev 2015; 59: 92–99.
Marhe R, Luijten M, van de Wetering BJ, Smits M, Franken IH . Individual differences in anterior cingulate activation associated with attentional bias predict cocaine use after treatment. Neuropsychopharmacology 2013; 38: 1085–1093.
Murdaugh DL, Cox JE, Cook EW 3rd, Weller RE . fMRI reactivity to high-calorie food pictures predicts short- and long-term outcome in a weight-loss program. Neuroimage 2012; 59: 2709–2721.
Heller AS, Johnstone T, Light SN, Peterson MJ, Kolden GG, Kalin NH et al. Relationships between changes in sustained fronto-striatal connectivity and positive affect in major depression resulting from antidepressant treatment. Am J Psychiatry 2013; 170: 197–206.
Ten Kulve JS, Veltman DJ, van Bloemendaal L, Barkhof F, Drent ML, Diamant M et al. Liraglutide reduces CNS activation in response to visual food cues only after short-term treatment in patients with type 2 diabetes. Diabetes Care 2016; 39: 214–221.
Bruce AS, Bruce JM, Ness AR, Lepping RJ, Malley S, Hancock L et al. A comparison of functional brain changes associated with surgical versus behavioral weight loss. Obesity (Silver Spring) 2014; 22: 337–343.
Bruce JM, Hancock L, Bruce A, Lepping RJ, Martin L, Lundgren JD et al. Changes in brain activation to food pictures after adjustable gastric banding. Surg Obes Relat Dis 2012; 8: 602–608.
Faulconbridge LF, Ruparel K, Loughead J, Allison KC, Hesson LA, Fabricatore AN et al. Changes in neural responsivity to highly palatable foods following roux-en-Y gastric bypass, sleeve gastrectomy, or weight stability: an fMRI study. Obesity (Silver Spring) 2016; 24: 1054–1060.
Ochner CN, Kwok Y, Conceicao E, Pantazatos SP, Puma LM, Carnell S et al. Selective reduction in neural responses to high calorie foods following gastric bypass surgery. Ann Surg 2011; 253: 502–507.
Ochner CN, Laferrere B, Afifi L, Atalayer D, Geliebter A, Teixeira J . Neural responsivity to food cues in fasted and fed states pre and post gastric bypass surgery. Neurosci Res 2012; 74: 138–143.
Ochner CN, Stice E, Hutchins E, Afifi L, Geliebter A, Hirsch J et al. Relation between changes in neural responsivity and reductions in desire to eat high-calorie foods following gastric bypass surgery. Neuroscience 2012; 209: 128–135.
Scholtz S, Miras AD, Chhina N, Prechtl CG, Sleeth ML, Daud NM et al. Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding. Gut 2014; 63: 891–902.
Frank S, Heinze JM, Fritsche A, Linder K, von Feilitzsch M, Konigsrainer A et al. Neuronal food reward activity in patients with type 2 diabetes with improved glycemic control after bariatric surgery. Diabetes Care 2016; 39: 1311–1317.
Goldman RL, Canterberry M, Borckardt JJ, Madan A, Byrne TK, George MS et al. Executive control circuitry differentiates degree of success in weight loss following gastric-bypass surgery. Obesity (Silver Spring) 2013; 21: 2189–2196.
Buchwald H, Oien DM . Metabolic/bariatric surgery worldwide 2011. Obes Surg 2013; 23: 427–436.
Nguyen NT, Nguyen B, Gebhart A, Hohmann S . Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg 2013; 216: 252–257.
Hollmann M, Hellrung L, Pleger B, Schlogl H, Kabisch S, Stumvoll M et al. Neural correlates of the volitional regulation of the desire for food. Int J Obes (Lond) 2012; 36: 648–655.
Kober H, Mende-Siedlecki P, Kross EF, Weber J, Mischel W, Hart CL et al. Prefrontal-striatal pathway underlies cognitive regulation of craving. Proc Natl Acad Sci USA 2010; 107: 14811–14816.
Siep N, Roefs A, Roebroeck A, Havermans R, Bonte M, Jansen A . Fighting food temptations: the modulating effects of short-term cognitive reappraisal, suppression and up-regulation on mesocorticolimbic activity related to appetitive motivation. Neuroimage 2012; 60: 213–220.
Yokum S, Stice E . Cognitive regulation of food craving: effects of three cognitive reappraisal strategies on neural response to palatable foods. Int J Obes (Lond) 2013; 37: 1565–1570.
Val-Laillet D, Aarts E, Weber B, Ferrari M, Quaresima V, Stoeckel LE et al. Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. Neuroimage Clin 2015; 8: 1–31.
Zijlstra H, van Middendorp H, Devaere L, Larsen JK, van Ramshorst B, Geenen R . Emotion processing and regulation in women with morbid obesity who apply for bariatric surgery. Psychol Health 2012; 27: 1375–1387.
Handley JD, Williams DM, Caplin S, Stephens JW, Barry J . Changes in cognitive function following bariatric surgery: a systematic review. Obes Surg 2016; 26: 2530–2537.
Gross JJ, John OP . Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003; 85: 348–362.
van Strien T, Frijters JER, Bergers GPA, Defares PB . The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord 1986; 5: 295–315.
Stunkard AJ, Messick S . The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985; 29: 71–83.
Lowe MR, Butryn ML, Didie ER, Annunziato RA, Thomas JG, Crerand CE et al. The Power of Food Scale. A new measure of the psychological influence of the food environment. Appetite 2009; 53: 114–118.
Beck AT, Steer RA, Brown GK . Manual for the Beck Depression Inventory-II. Psychological Corporation: San Antonio, TX, USA, 1996.
Spielberger CD, Gorsuch RL, Lushene RE . Manual for the State-Trait Anxiety Inventory. Consultin Psychologists Press: Palo Alto, CA, USA, 1970.
Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH . An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 2003; 19: 1233–1239.
Whitfield-Gabrieli S . Region of Interest Extraction (REX) Toolbox. Gabrieli Lab, MIT Department of Brain and Cognitive Sciences: Cambridge, MA, USA, 2009.
Faul F, Erdfelder E, Lang AG, Buchner A . G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175–191.
Sczepaniak JP, Owens ML, Shukla H, Perlegos J, Garner W . Comparability of weight loss reporting after gastric bypass and sleeve gastrectomy using BOLD data 2008-2011. Obes Surg 2015; 25: 788–795.
Rieber N, Giel KE, Meile T, Enck P, Zipfel S, Teufel M . Psychological dimensions after laparoscopic sleeve gastrectomy: reduced mental burden, improved eating behavior, and ongoing need for cognitive eating control. Surg Obes Relat Dis 2013; 9: 569–573.
Chao A, Grilo CM, White MA, Sinha R . Food cravings, food intake, and weight status in a community-based sample. Eat Behav 2014; 15: 478–482.
Buscemi J, Rybak TM, Berlin KS, Murphy JG, Raynor HA . Impact of food craving and calorie intake on body mass index (BMI) changes during an 18-month behavioral weight loss trial. J Behav Med 2017; 40: 565–573.
Meule A, Richard A, Platte P . Food cravings prospectively predict decreases in perceived self-regulatory success in dieting. Eat Behav 2017; 24: 34–38.
Mans E, Serra-Prat M, Palomera E, Sunol X, Clave P . Sleeve gastrectomy effects on hunger, satiation, and gastrointestinal hormone and motility responses after a liquid meal test. Am J Clin Nutr 2015; 102: 540–547.
van der Plasse G, van Zessen R, Luijendijk MC, Erkan H, Stuber GD, Ramakers GM et al. Modulation of cue-induced firing of ventral tegmental area dopamine neurons by leptin and ghrelin. Int J Obes (Lond) 2015; 39: 1742–1749.
Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H et al. Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex 2014; 24: 2981–2990.
Staudinger MR, Erk S, Walter H . Dorsolateral prefrontal cortex modulates striatal reward encoding during reappraisal of reward anticipation. Cereb Cortex 2011; 21: 2578–2588.
Kolata G . After weight-loss surgery, a year of joys and disappointments. New York Times, 27 December 2016.
Goldstein-Piekarski AN, Korgaonkar MS, Green E, Suppes T, Schatzberg AF, Hastie T et al. Human amygdala engagement moderated by early life stress exposure is a biobehavioral target for predicting recovery on antidepressants. Proc Natl Acad Sci USA 2016; 113: 11955–11960.
Stice E, Yokum S, Burger K, Rohde P, Shaw H, Gau JM . A pilot randomized trial of a cognitive reappraisal obesity prevention program. Physiol Behav 2015; 138: 124–132.
Gluck ME, Alonso-Alonso M, Piaggi P, Weise CM, Jumpertz-von Schwartzenberg R, Reinhardt M et al. Neuromodulation targeted to the prefrontal cortex induces changes in energy intake and weight loss in obesity. Obesity (Silver Spring) 2015; 23: 2149–2156.
Hall PA, Vincent CM, Burhan AM . Non-invasive brain stimulation for food cravings, consumption, and disorders of eating: a review of methods, findingss and controversies. Appetite 2017. epub ahead of print 11 March 2017 doi:10.1016/j.appet.2017.03.006.
Hanlon CA, Dowdle LT, Austelle CW, DeVries W, Mithoefer O, Badran BW et al. What goes up, can come down: novel brain stimulation paradigms may attenuate craving and craving-related neural circuitry in substance dependent individuals. Brain Res 2015; 1628 (Pt A): 199–209.
Acknowledgements
We thank the study participants for volunteering their time; Vanessa Calderon, Mark Gorman and Noreen Harrington for coordinating subject recruitment and Max Curran for programming the fMRI paradigm. This work was funded by the Harvard Nutrition Obesity Research Center (P30 DK040561), Global Foundation for Eating Disorders and the Harvard Catalyst/The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and affiliated academic health-care centers). Support for a portion of LMH’s time was provided by NIMH K01 HD019222 and BWH BRI Fund for Research Excellence.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Holsen, L., Davidson, P., Cerit, H. et al. Neural predictors of 12-month weight loss outcomes following bariatric surgery. Int J Obes 42, 785–793 (2018). https://doi.org/10.1038/ijo.2017.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.190
This article is cited by
-
Brain functional and structural magnetic resonance imaging of obesity and weight loss interventions
Molecular Psychiatry (2023)
-
Neural activation of regions involved in food reward and cognitive control in young females with anorexia nervosa and atypical anorexia nervosa versus healthy controls
Translational Psychiatry (2023)
-
Novel Insights into the Physiology of Nutrient Sensing and Gut-Brain Communication in Surgical and Experimental Obesity Therapy
Obesity Surgery (2023)
-
Towards precision medicine in bariatric surgery prescription
Reviews in Endocrine and Metabolic Disorders (2023)
-
Cognitive Control and Weight Loss After Bariatric Surgery: the BARICO Study
Obesity Surgery (2023)