Abstract
Background:
It is debatable whether the body mass index (BMI) value that is associated with the lowest all-cause mortality has increased over time. Such an increase might indicate that the WHO BMI categories for normal weight and overweight need to be revised over time. This study assessed whether the BMI associated with the lowest all-cause mortality increased over time among US adults in the National Health Interview Survey.
Methods:
This survey with up to 25 years of follow-up included 901 197 participants, aged 20 to 79 years with baseline BMI between 18.5 and 39.9 kg m−2 and known mortality status between the original survey dates and 31 December 2011. The BMI values associated with the lowest mortality were estimated for different survey time periods: 1986–1989, 1990–1994, 1995–1999, 2000–2004 and 2000–2009.
Results:
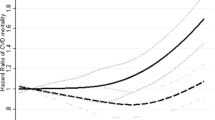
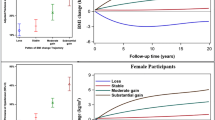
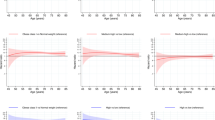
Among 901 197 participants, 130 495 died during over 14.5 million person-years of follow-up. There was a U-shaped BMI–mortality association in all the survey periods. When we used the original follow-up durations, the BMI associated with the lowest mortality increased monotonically from 23.9 kg m−2 in 1986–1989 to 28.6 kg m−2 in 2005–2009. When using a fixed follow-up duration of 5, 10, 15 or 20 years, we found no monotonic increasing pattern in the BMI associated with the lowest mortality. With duration of 15 years, the estimates of BMI associated with lowest mortality appeared to be relatively stable over time among both the general population and never smokers free from cardiovascular disease and cancer at baseline.
Conclusions:
With a fixed long-term follow-up duration, the BMI value associated with the lowest mortality remains relatively stable over time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Afzal S, Tybjaerg-Hansen A, Jensen GB, Nordestgaard BG . Change in body mass index associated with lowest mortality in Denmark, 1976-2013. JAMA 2016; 315: 1989–1996.
Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ 2016; 353: i2156.
Flegal KM, Kit BK, Orpana H, Graubard BI . Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013; 309: 71–82.
Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016; 388: 776–786.
Flegal KM, Graubard BI, Williamson DF, Cooper RS . Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol 2011; 173: 1–9.
Flegal KM, Graubard BI, Williamson DF, Gail MH . Excess deaths associated with underweight, overweight, and obesity. JAMA 2005; 293: 1861–1867.
Flegal KM, Graubard BI, Williamson DF, Gail MH . Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007; 298: 2028–2037.
Greenberg JA . The obesity paradox in the US population. Am J Clin Nutr 2013; 97: 1195–1200.
Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011; 364: 719–729.
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010; 363: 2211–2219.
Prospective Studies C, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–1096.
Wang Z, Liu M, Pan T, Tong S . Lower mortality associated with overweight in the US National Health Interview Survey: is overweight protective? Medicine 2016; 95: e2424.
Wang Z . Body mass index and all-cause mortality. JAMA 2016; 316: 991–992.
Bhupathiraju SN, Willett WC, Hu FB . Body mass index and all-cause mortality. JAMA 2016; 316: 991.
Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L . Design and estimation for the national health interview survey, 2006-2015. Vital Health Stat 2 2014; 165: 1–53.
Botman SL, Moore TF, Moriarity CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995-2004. Vital Health Stat 2 2000; 130: 1–31.
Royston P, Lambert PC . Flexible Parametric Survival Analysis Using Stata : Beyond the Cox Model. Stata Press: College Station, TX, USA, 2011, xxvi, 347p.
StataCorp Stata Statistical Software: Release 14. StataCorp LP: College Station, TX, USA, 2015.
He J . Modeling the dynamic association of BMI and mortality in the Framingham Heart Study. Ann Epidemiol 2011; 21: 517–525.
Brug J, Wammes B, Kremers S, Giskes K, Oenema A . Underestimation and overestimation of personal weight status: associations with socio-demographic characteristics and weight maintenance intentions. J Hum Nutr Diet 2006; 19: 253–262.
Gillum RF, Sempos CT . Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutr J 2005; 4: 27.
Hattori A, Sturm R . The obesity epidemic and changes in self-report biases in BMI. Obesity (Silver Spring) 2013; 21: 856–860.
Jeffery RW . Bias in reported body weight as a function of education, occupation, health and weight concern. Addict Behav 1996; 21: 217–222.
Peter RS, Mayer B, Concin H, Nagel G . The effect of age on the shape of the BMI-mortality relation and BMI associated with minimum all-cause mortality in a large Austrian cohort. Int J Obes (Lond) 2015; 39: 530–534.
Acknowledgements
We gratefully acknowledge the Centers for Disease Control and Prevention, USA, for access to the NHIS public-use data. We thank Drs Katherine Flegal (Stanford University) and Barry Graubard (National Cancer Institute) for their critical comments and suggestions. This work was supported by the National Health and Medical Research Council of Australia (APP1042343, ZW) and a University of Queensland International Scholarship (44078179, YP). These funding sources had no role in the design of this study and did not have any role during its execution, analyses, interpretation of the data or decision to submit results.
Author contributions
ZW conceived and designed the study, acquired the data and drafted the manuscript. ZW and YP obtained the funding. ZW, YP and BD played an important role in interpreting the results and revising the manuscript. All authors have approved the final manuscript for submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, Z., Peng, Y. & Dong, B. Is body mass index associated with lowest mortality increasing over time?. Int J Obes 41, 1171–1175 (2017). https://doi.org/10.1038/ijo.2017.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.107
This article is cited by
-
Optimal cut-off values for anthropometric measures of obesity in screening for cardiometabolic disorders in adults
Scientific Reports (2020)
-
Short-term weight gain is associated with accumulation of multimorbidity in mid-aged women: a 20-year cohort study
International Journal of Obesity (2019)