Abstract
The purpose of this study was to compare the outcomes of patients undergoing cardiac transplantation stratified by body mass index (BMI, kg m−2). The Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease registry captured 220 cardiac transplantations in Alberta, Canada from January 2004 to April 2013. All recipients were stratified by BMI into five groups (BMI: <20, 20–24.9, 25–29.9, 30–<34.9 and ⩾35). Patient characteristics were analyzed by analysis of variance and χ2 analyses. Kaplan–Meier was used to examine survival differences. Preoperative characteristics demonstrated significant increases in metabolic syndrome, prior myocardial infarction and prior coronary artery bypass graft in patients with morbid obesity. Intra-operatively, there was an increase in cardiopulmonary bypass time in patients with morbid obesity (P<0.01). Postoperative analysis revealed increased rates of early complications (<30 days), associated with a BMI >35. Long-term survival was also significantly decreased in patients with morbid obesity. Of interest, obesity (BMI, 30–34.9) was not associated with decreased survival. These findings suggest that, post-cardiac transplantation, patients who have a BMI ⩾35 have lower long-term survival compared with all other BMI groups. However, patients with BMI 30–34.9 did not have significantly worse outcomes and should not be excluded for heart transplantation based on BMI.
Similar content being viewed by others
Introduction
Cardiac transplant rates have remained relatively constant over the past 10 years in both Canada1 and the United States.2 Nevertheless, as a result of the obesity epidemic,3 there are an increasing proportion of obese patients being referred for cardiac transplant consideration. Despite the growing prevalence of this patient population, there remains a paucity of randomized trial evidence comparing the outcomes of obese and non-obese cardiac transplant recipients. This lack of evidence has lead to substantial debate as to the optimal management strategy for obese patients with end-stage heart failure.4, 5 Several studies have suggested an increased risk of mortality in obese patients compared with non-obese patients undergoing orthotopic heart transplantation.4, 6, 7, 8 This has supported long-standing consensus statements that have deemed obesity a relative contraindication to heart transplantation.9
Obesity in cardiac transplant patients, as well as the general population, is linked to hypertension, diabetes and dyslipidemia, which constitutes ‘metabolic syndrome’.8, 9, 10, 11, 12, 13, 14 These factors, along with smoking, are directly related to an exponentially elevated mortality risk.4 Some authors have proposed that the metabolic syndrome increases the risk of cardiac allograft vasculopathy and that this accounts for adverse outcomes in cardiac transplant recipients with obesity.6, 7 Other reports showing a neutral effect of obesity on cardiac transplantation outcomes raise the possibility that it is not a relative contraindication to surgery. Therefore, the purpose of this study was to compare the outcomes of patients undergoing cardiac transplantation stratified by body mass index (BMI, kg m−2).
Patients and Methods
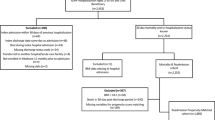
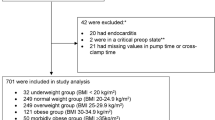
Cardiac transplant patients from 2004–2013 in the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) registry were included in this study. The APPROACH project is a province-wide inception cohort of all adult Alberta residents undergoing cardiac catheterization. The APPROACH registry contains detailed clinical data collected at catheterization, percutaneous coronary intervention, surgery, and one, three and five year follow-up. Finally there is a quarterly merge with the Alberta Bureau of Vital Statistics to provide mortality data. The human research ethics office at the University of Alberta prior to accessing the database granted ethics approval. Patients were grouped based on their preoperative BMI into five groups: BMI<20 (underweight), 20–24.9 (normal weight), 25–29.9 (overweight), 30–34.9 (obese) and >35 (morbidly obese). In order to prevent having too few underweight patients to achieve statistical significance, this study used a BMI <20 for underweight patients.15
Relevant preoperative characteristics were obtained for all patients. Preoperative known risk factors that could impact the outcome of cardiac transplantation were also identified and included. Similarly, the peri-operative variables and risk factors including length of surgery, ischemic time and cross-clamp data, were collected along with postoperative complications. Preoperative categorical variables were compared among the five groups by χ2 test for independence (degree of freedom was 4). Continuous variables (age, list to transplant times) were compared by one-way analysis of variance (ANOVA). Between groups comparison was done using the logistic regression and one-way ANOVA with post hoc Bonferroni correction, for categorical and continuous variables, respectively. Finally, patients were followed-up to 8 years to determine their long-term survival using the Kaplan–Meier statistical methods. Survival curves were generated to graphically present long-term survival. Cox proportional hazard models were used to provide information on independent risk factors for mortality. The proportional hazards assumption was tested.
Results
Baseline demographics
From 1 January 2004 to 31 December 2013, a total of 220 consecutive patients who underwent cardiac transplantation that were stratified by BMI into five categories: underweight (BMI<20, n=17, 7.7%), normal weight (BMI 20–24.9, n=73, 33.2%), overweight (BMI 25–29.9, n=81, 36.8%), obese (BMI 30–34.9, n=39, 17.7%) and morbidly obese (BMI>35, n=10, 4.5%). Baseline demographics and significance are summarized in Table 1. Table 1 demonstrated various preoperative characteristics that were not significantly different among the five groups. Preoperative risk factors that were not significantly different among the five groups included, hyperlipidemia, a history of smoking, type 1 diabetes mellitus, peripheral vascular disease, dialysis dependent renal failure, malignancy, liver disease and gastrointestinal disease (Supplementary Table S1 found in the online supplements). Supplementary Table S1 also shows that, when compared with the normal BMI patients, overweight and obese patients were significantly older, but the extremes of BMI (groups 1 and 5) did not differ significantly in age from the normal BMI group.
As well, Table 1 also reveals that increasing patient BMI has a significantly increased incidence of several preoperative characteristics when compared with patients with a normal preoperative BMI (Supplementary Table S1 found in the online supplements). When compared with normal BMI patients, the odds of hypertension and type 2 diabetes increase with BMI (Supplementary Table S1). As well, obese and morbidly obese patients were found to have increased odds of having a prior myocardial infarction and prior CABG surgery (Supplementary Table S1).
Peri-operative analysis and post-transplant survival
As shown in Table 2, intra-operative donor ischemic time and aortic cross clamp time were similar among the five groups. However, morbid obesity was associated with significantly prolonged cardiopulmonary bypass time. Postoperative patient outcomes are also summarized in Table 2. Interestingly, the incidence of deep sternal wound infection was not significantly different among the five groups. As well, post-op hemorrhage, sepsis, graft rejection, number of days on the ventilator and length of stay in the intensive care unit (ICU) were also similar between the groups. The rate of postoperative infection is significantly higher in obese patients when compared with normal BMI patients (OR 4.38, 1.74–11.03), while underweight, overweight and morbidly obese groups did not differ significantly when compared with normal BMI patients (1.35, 0.33–5.55; 1.55, 0.65–3.68; 1.58, 0.29–8.51; underweight, overweight and morbidly obese groups, respectively). Morbidly obese patients were however, significantly more likely to develop early complications (<30 days).
The mean survival for all groups is shown in Table 2 (P<0.001). The Kaplan–Meier estimates of survival (Supplementary Figure S1 found in the online supplements) identified that groups 1, 2, 3 and 4 had no significant correlation between BMI and decreased survival. That is, obese patients (BMI 30–34.9) had a similar survival rate post-cardiac transplantation as underweight, normal weight and overweight patients. However a BMI>35 was associated with significantly decreased long-term survival (Supplementary Figure S1).
Discussion
While previous studies have established that recipient preoperative BMI>35 is an independent risk factor for mortality5 after cardiac transplantation, we have extended this evidence based on three main ways. First we have shown that obese patients (BMI 30–34.9) do not experience decreased long-term survival post-cardiac transplantation. The body of evidence surrounding this particular patient population remains conflicted8, 16, 17, 18 and we have added evidence to support continued cardiac transplantation of the obese patient. Survival results are not significantly influenced by era bias, as there were similar numbers of patients in each category throughout the study since 2004. Second, we have demonstrated that a BMI>35 significantly increases intra-operative cardiopulmonary bypass time. Third, we have demonstrated that patients with a BMI>35 undergoing cardiac transplantation are more likely to develop early complications when compared with other BMI groups. Interestingly, a BMI>35 did not predispose patients to prolonged ventilator times and ICU length of stay.
Our results are consistent with several observational studies in patients undergoing cardiac transplantation. Russo et al.5 showed that obese (BMI 30–34.99, n=3005) had a similar survival rate post-cardiac transplant when compared with normal weight (BMI 18.5–24.99, n=7883) patients 47.5%, CI 42.6–52.2% and 52%, CI 49.4–54.5%, respectively. Moreover, they also demonstrated that morbidly obese patients (BMI>35, n=684) undergoing cardiac transplantation had a decreased survival at 10 years (41.6%, CI 29.8–52.3%) when compared with normal weight patients. Kobashigawa et al.19 also reported that patients with a preoperative BMI>33 tended to have an increased risk of death post-cardiac transplantation at one and five years. This study challenges the previous long-standing notion that preoperative obesity (BMI 30–34.9) is associated with an increased risk of death post-cardiac transplantation.8, 16
Although we used data collected prospectively on adults undergoing cardiac transplantation in one quaternary care institution with 100% follow-up through linkage to electronic mortality records (thereby minimizing recall or ascertainment bias) within a Canadian province with universal health care access, there are several limitations to our study. First, the present study is an observational evaluation. Therefore, we can only explore associations and not causation. Second, we do not have, post-cardiac transplant, patient BMI, which has also been described as a risk factor after transplant.12, 15, 16, 20 However, the purpose of this study was to aid clinicians caring for obese patients with appropriate decision making, surrounding advanced heart failure therapy referrals.
Conclusions
We have shown the morbid obesity in association with the reduced survival post-cardiac transplantation, and this should be considered when assessing patient risk. However, obese patients (BMI 30–34.9) do not experience decreased long-term survival compared with patients with BMI<30, and should therefore not be excluded from consideration of cardiac transplantation.
References
AnonymousCORR Report 2012: CST Annual General Meeting. Available at http://www.cihi.ca/CIHI-ext-portal/pptx/internet/corr_report_20120612_02ccf_en.
AnonymousServices UD of H and H. OPTN/SRTR Annual Data Report. Available at http://srtr.transplant.hrsa.gov/annual_reports/2011/default.aspx.
AnonymousGlobal Health Observatory (GHO) data - Obesity. Available at http://www.who.int/gho/ncd/risk_factors/obesity_text/en/.
Kilic A, Conte JV, Shah AS, Yuh DD . Orthotopic heart transplantation in patients with metabolic risk factors. Ann Thorac Surg 2012; 93: 718–724.
Russo MJ, Hong KN, Davies RR, Chen JM, Mancini DM, Oz MC et al. The effect of body mass index on survival following heart transplantation: do outcomes support consensus guidelines? Ann Surg 2010; 251: 144–152.
Valantine H . Cardiac allograft vasculopathy after heart transplantation: risk factors and management. J Heart Lung Transplant 2004; 23: S187–S193.
Marti V, Romeo I, Aymat R, Garcia J, Guiteras P, Ballester M et al. Coronary endothelial dysfunction as a predictor of intimal thickening in the long term after heart transplantation. J Thorac Cardiovasc Surg 2001; 122: 1174–1180.
Lietz K, John R, Burke EA, Ankersmit JH, McCue JD, Naka Y et al. Pretransplant cachexia and morbid obesity are predictors of increased mortality after heart transplantation. Transplantation 2001; 72: 277–283.
Cimato TR, Jessup M . Recipient selection in cardiac transplantation: contraindications and risk factors for mortality. J Heart Lung Transplant 2002; 21: 1161–1173.
Weiss ES, Allen JG, Russell SD, Shah AS, Conte JV . Impact of recipient body mass index on organ allocation and mortality in orthotopic heart transplantation. J Heart Lung Transplant 2009; 28: 1150–1157.
Cordero Fort A, Gavira JJ, Alegria-Barrero E, Castano S, Martin A, Ubilla M et al. Prevalence of metabolic syndrome in heart transplant patients: role of previous cardiopathy and years since the procedure—the TRACA study. J Heart Lung Transplant 2006; 25: 1192–1198.
Grady KL, Naftel D, Pamboukian SV, Frazier OH, Hauptman P, Herre J et al. Post-operative obesity and cachexia are risk factors for morbidity and mortality after heart transplant: multi-institutional study of post-operative weight change. J Heart Lung Transplant 2005; 24: 1424–1430.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763–778.
Grundy SM . Multifactorial causation of obesity: implications for prevention. Am J Clin Nutr 1998; 67: 563S–572SS.
Habedank D, Anker SD . Post-operative obesity and cachexia after heart transplantation. J Heart Lung Transplant 2006; 25: 368.
Grady KL, White-Williams C, Naftel D, Costanzo MR, Pitts D, Rayburn B et al. Are preoperative obesity and cachexia risk factors for post heart transplant morbidity and mortality: a multi-institutional study of preoperative weight-height indices. Cardiac Transplant Research Database (CTRD) Group. J Heart Lung Transplant 1999; 18: 750–763.
Taylor DO, Edwards LB, Boucek MM, Trulock EP, Keck BM, Hertz MI . The registry of the International Society for Heart and Lung Transplantation: twenty-first official adult heart transplant report—2004. J Heart Lung Transplant 2004; 23: 796–803.
Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC Jr . Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA 2009; 301: 831–841.
Kobashigawa JA, Starling RC, Mehra MR, Kormos RL, Bhat G, Barr ML et al. Multicenter retrospective analysis of cardiovascular risk factors affecting long-term outcome of de novo cardiac transplant recipients. J Heart Lung Transplant 2006; 25: 1063–1069.
Winters GL, Kendall TJ, Radio SJ, Wilson JE, Costanzo-Nordin MR, Switzer BL et al. Post-transplant obesity and hyperlipidemia: major predictors of severity of coronary arteriopathy in failed human heart allografts. J Heart Transplant 1990; 9: 364–371.
Acknowledgements
The APPROACH registry is supported by donations from the Mazankowski Alberta Heart Institute, Libin Cardiovascular Institute, Alberta Health Services and industry sponsors (Merck Frost Canada Inc, Roche Canada, Eli Lilly Canada Inc, Bristol-Myers Squibb and Philips Medical Systems Canada). Dr Jayan Nagendran is supported by grants from the Mazankowski Alberta Heart Institute, University of Alberta Hospital Foundation and the Canadian Institute of Health Research—Canadian National Transplant Research Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Nagendran, J., Moore, M., Norris, C. et al. The varying effects of obesity and morbid obesity on outcomes following cardiac transplantation. Int J Obes 40, 721–724 (2016). https://doi.org/10.1038/ijo.2016.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.20
This article is cited by
-
Validation of days alive and out of hospital as a new patient-centered outcome to quantify life impact after heart transplantation
Scientific Reports (2022)
-
The effects of body mass index on long-term outcomes and cardiac remodeling following mitral valve repair surgery
International Journal of Obesity (2021)
-
Morbid Obesity as a Therapeutic Target for Heart Failure
Current Treatment Options in Cardiovascular Medicine (2019)