Abstract
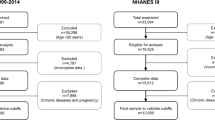
The United States Equal Employment Opportunity Commission has proposed rules allowing employers to penalize employees up to 30% of health insurance costs if they fail to meet ‘health’ criteria, such as reaching a specified body mass index (BMI). Our objective was to examine cardiometabolic health misclassifications given standard BMI categories. Participants (N=40 420) were individuals aged 18+ in the nationally representative 2005–2012 National Health and Nutrition Examination Survey. Using the blood pressure, triglyceride, cholesterol, glucose, insulin resistance and C-reactive protein data, population frequencies/percentages of metabolically healthy versus unhealthy individuals were stratified by BMI. Nearly half of overweight individuals, 29% of obese individuals and even 16% of obesity type 2/3 individuals were metabolically healthy. Moreover, over 30% of normal weight individuals were cardiometabolically unhealthy. There was no significant race-by-BMI interaction, but there was a significant gender-by-BMI interaction, F(4,64)=3.812, P=0.008. Using BMI categories as the main indicator of health, an estimated 74 936 678 US adults are misclassified as cardiometabolically unhealthy or cardiometabolically healthy. Policymakers should consider the unintended consequences of relying solely on BMI, and researchers should seek to improve diagnostic tools related to weight and cardiometabolic health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Catenacci VA, Hill JO, Wyatt HR . The obesity epidemic. Clin Chest Med 2009; 30: 415–444.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH . The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009; 9: 88.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: Prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med 2008; 168: 1617–1624.
Cawley J . The impact of obesity on wages. J Hum Resour 2004; 39: 451–474.
Tannenbaum D, Valasek CJ, Knowles ED, Ditto PH . Incentivizing wellness in the workplace: Sticks (not carrots) send stigmatizing signals. Psychol Sci 2013; 24: 1512–1522.
Hunger JM, Major B, Blodorn A, Miller C . Weighed down by stigma: How weight-based social identity threat influences weight gain and health. Soc Psychol Personal Compass 2015; 9: 255–268.
Harrington M, Gibson S, Cottrell RC . A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev 2009; 22: 93–108.
National Health and Nutrition Examination Survey: Questionnaires, datasets, and related documentation. Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
Task 2: When and how to construct weights when combining survey cycles. Available at: http://www.cdc.gov/nchs/tutorials/nhanes/SurveyDesign/Weighting/Task2.htm.
National Health and Nutrition Examination Survey: Analytic guidelines, 1999–2010. Available at: http://www.cdc.gov/nchs/data/series/sr_02/sr02_161.pdf.
Tomiyama AJ, Finch LE, Belsky ACI, Buss J, Finley C, Schwartz MB et al. Weight bias in 2001 versus 2013: Contradictory attitudes among obesity researchers and health professionals. Obesity (Silver Spring) 2015; 23: 46–53.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M . Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015; 16: 319–326.
Friedemann Smith C, Heneghan C, Ward A . Moving focus from weight to health. What Are the components used in interventions to improve cardiovascular health in children? PLoS One 2015; 10: e0135115.
Hunger JM, Tomiyama AJ . A call to shift the public health focus away from weight. Am J Public Health 2015; 105: e3–e3.
Ross R, Blair S, de Lannoy L, Després J-P, Lavie CJ . Changing the endpoints for determining effective obesity management. Prog Cardiovasc Dis 2015; 57: 330–336.
Ortega FB, Lee D-C, Katzmarzyk PT, Ruiz JR, Sui X, Church TS et al. The intriguing metabolically healthy but obese phenotype: Cardiovascular prognosis and role of fitness. Eur Heart J 2013; 34: 389–397.
Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN . Fitness vs. fatness on all-cause mortality: A meta-analysis. Prog Cardiovasc Dis 2014; 56: 382–390.
Lavie CJ, De Schutter A, Milani RV . Healthy obese versus unhealthy lean: The obesity paradox. Nat Rev Endocrinol 2015; 11: 55–62.
Plourde G, Karelis AD . Current issues in the identification and treatment of metabolically healthy but obese individuals. Nutr Metab Cardiovasc Dis 2014; 24: 455–459.
Must A, Phillips SM, Naumova EN . Occurrence and timing of childhood overweight and mortality: Findings from the Third Harvard Growth Study. J Pediatr 2012; 160: 743–750.
Acknowledgements
AJT was supported by the Hellman Fellows fund. The Hellman Fellows Fund had no further role in the design of the study, in the collection, analysis and interpretation of the data, in writing the report and in deciding to submit the paper for publication. AJT and JMH conceived the study. AJT obtained funding. CW analyzed the data. AJT, JMH, JNC and CW interpreted the analyses and drafted the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Tomiyama, A., Hunger, J., Nguyen-Cuu, J. et al. Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005–2012. Int J Obes 40, 883–886 (2016). https://doi.org/10.1038/ijo.2016.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.17
This article is cited by
-
Association between segmental body composition and bone mineral density in US adults: results from the NHANES (2011–2018)
BMC Endocrine Disorders (2023)
-
Four key questions on the new wave of anti-obesity drugs
Nature (2023)
-
Why BMI is flawed — and how to redefine obesity
Nature (2023)
-
The ‘breakthrough’ obesity drugs that have stunned researchers
Nature (2023)
-
Multiomic signatures of body mass index identify heterogeneous health phenotypes and responses to a lifestyle intervention
Nature Medicine (2023)