Abstract
Background/Objectives:
Psychosocial stress has been proposed to contribute to obesity, particularly abdominal, or central obesity, through chronic activation of the neuroendocrine systems. However, these putative relationships are complex and dependent on country and cultural context. We investigated the association between psychosocial factors and general and abdominal obesity in the Prospective Urban Rural Epidemiologic study.
Subjects/Methods:
This observational, cross-sectional study enrolled 151 966 individuals aged 35–70 years from 628 urban and rural communities in 17 high-, middle- and low-income countries. Data were collected for 125 290 individuals regarding education, anthropometrics, hypertension/diabetes, tobacco/alcohol use, diet and psychosocial factors (self-perceived stress and depression).
Results:
After standardization for age, sex, country income and urban/rural location, the proportion with obesity (body mass index ⩾30 kg m−2) increased from 15.7% in 40 831 individuals with no stress to 20.5% in 7720 individuals with permanent stress, with corresponding proportions for ethnicity- and sex-specific central obesity of 48.6% and 53.5%, respectively (P<0.0001 for both). Associations between stress and hypertension/diabetes tended to be inverse. Estimating the total effect of permanent stress with age, sex, physical activity, education and region as confounders, no relationship between stress and obesity persisted (adjusted prevalence ratio (PR) for obesity 1.04 (95% confidence interval: 0.99–1.10)). There was no relationship between ethnicity- and sex-specific central obesity (adjusted PR 1.00 (0.97–1.02)). Stratification by region yielded inconsistent associations. Depression was weakly but independently linked to obesity (PR 1.08 (1.04–1.12)), and very marginally to abdominal obesity (PR 1.01 (1.00–1.03)).
Conclusions:
Although individuals with permanent stress tended to be slightly more obese, there was no overall independent effect and no evidence that abdominal obesity or its consequences (hypertension, diabetes) increased with higher levels of stress or depression. This study does not support a causal link between psychosocial factors and abdominal obesity.
Similar content being viewed by others
Introduction
Over the past century, rapid urbanization has led to marked changes in nutrition, transportation and psychosocial environment. Although poverty and lack of food persist as major problems in some parts of the world, large segments of the population in many countries of differing economic status have increasing availability of food, particularly energy-dense food, along with reduced energy expenditure. Even though caloric imbalance is likely one of the main driving forces behind the current obesity epidemic, psychosocial stress factors, which are common in modern society, have been hypothesized to contribute to the increased prevalence of obesity, through changes in lifestyle and chronic activation of the neuroendocrine system.1, 2, 3, 4 Obesity (especially abdominal, or central obesity) increases insulin resistance, diabetes, hypertension and dyslipidemia, which in turn increase the risk for cardiovascular disease.5, 6, 7
Psychosocial stress encompasses many dimensions. Support for the link between psychosocial factors, obesity and the metabolic effect of obesity derives from several sources. In the Whitehall study,8 measures of work stress predicted later development of obesity and abdominal obesity, as well as the metabolic syndrome.9 However, meta-analyses on the effects of work stress on obesity have shown weak, or absent effects.10, 11 Nevertheless, these relationships, if any, are likely very complex and dependent on country and cultural context. Most studies have been carried out in Western populations. We set out to investigate a tentative association between psychosocial factors and general and abdominal obesity in a large international cross-sectional study.
Subjects and methods
Setting and population
The Prospective Urban Rural Epidemiologic (PURE) study collected data from 382 341 men and women from 107 599 households in 628 communities (348 urban and 280 rural) in 17 countries on five continents.12 Sites were selected where investigators were committed to collecting high-quality data with a modest budget, and who would attempt to follow-up participants for 10 years or more. To ensure sociopolitical diversity, strict proportionate sampling of any specific country or region was not carried out. From World Bank classifications at the time the PURE study was started, four low-income countries (LICs; Bangladesh, India, Pakistan and Zimbabwe), three lower middle-income countries (China, Colombia and Iran), seven upper middle-income countries (UMICs; Argentina, Brazil, Chile, Malaysia, Poland, South Africa and Turkey) and three high-income countries (HICs; Canada, Sweden and United Arab Emirates) were included. In every country, urban and rural communities at collaborating sites were selected on the basis of previously published guidelines.13 A community was defined as a group of people with certain characteristics in common (culture, socioeconomic status and use of amenities, goods and services), residing in a defined geographical area.12 The aim of PURE was to achieve a representative sample of adults aged 35–70 years within every community, based on representativeness and feasibility of long-term follow-up. Common and standardized approaches were used for the calculation of the number of households, identification of individuals, recruitment procedures and data collection. Households were approached by various methods and were eligible if at least one household member was aged 35–70 years and they intended to live at their current address for a further 4 years. All eligible individuals in a household who provided written informed consent were enrolled.
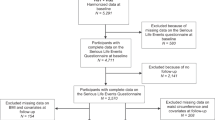
Recruitment started in Karnataka, India in January 2003, with most communities recruited between January 2005 and December 2009. Of the enumerated individuals, 197 332 (52%) were in the prespecified age range, and of these, 153 996 (78%) consented to participate. The response rate was 84% in HIC, 87% in MIC, 82% in LMIC and 55% in LIC. At the analysis stage, some individuals were found to be outside the age criteria, and were excluded, leaving 151 966 that met the age criteria of 35–70 years.14 In total, 125 290 subjects (82.4%) provided data on psychosocial variables and formed the study population for the present investigation.
Procedures
Standardized questionnaires were used to collect data at national, community, household and individual levels. Questions about age, sex, education, smoking status, hypertension and diabetes were identical to those in the INTERHEART15 and INTERSTROKE16 studies. Hypertension was defined as blood pressure (BP) >140/90 mm Hg or self-reported by history, and diabetes as fasting glucose ⩾7.0 mmol l−1 or self-reported. Standard physical measurements of height, weight, waist and hip circumference were performed in duplicate by the same examiner. Waist and hip circumferences were measured with a non-stretchable standard tape measure attached to a spring balance exerting a force of 750 g. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Obesity was defined as BMI ⩾30 kg m−2. To describe the distribution of abdominal obesity across regions, we used sex-specific cutoff points for waist-to-hip ratio (WHR) as determined by World Health Organization (WHO) classification (0.9 for males; 0.85 for females).17 Ethnicity and sex-specific cutoff waist circumference levels as defined by the International Diabetes Federation were used as the dependent variable in the analysis of the effect of psychosocial variables on abdominal obesity (downloaded 11 April 2014 at http://www.idf.org/metabolic-syndrome): Europid, Eastern Mediterranean and Middle East and Sub-Saharan African men ⩾94 cm, women ⩾80 cm; South Asian men ⩾90 cm, women ⩾80 cm; Chinese men ⩾90 cm, women ⩾80 cm. One-week recall of physical activity (PA) and sitting time were assessed using the long-form International Physical Activity Questionnaire,18 with high PA defined as metabolic equivalent task (MET) score ⩾3000, moderate as MET score 600–3000 and low as MET score <600 MET-minutes per week. A diet score was constructed from an adaptation of the alternative healthy eating index approach described by McCullough and Willett.19 Higher scores indicated more frequent healthy food choices such as vegetables and fruits and lower scores indicated higher consumption of unhealthy foods. Each participant’s total score was calculated. Recorded frequencies of consumption and portion sizes were converted to daily intake, and a modified alternative healthy eating index was calculated. The sample was separately stratified into tertiles of modified alternative healthy eating index.
A standard, simple set of questions about psychosocial conditions during the previous 12 months was included (as used in INTERHEART20). Psychological stress was assessed by two single-item questions relating to stress at work and at home. Stress was defined as feeling irritable, filled with anxiety or as having sleeping difficulties as a result of conditions at work or at home. For each question, participants were asked to report how often they had felt stressed, using the following response options: 1, never; 2, some periods; 3, several periods; and 4, permanent stress. These two questions are an adaptation of a single question that has been used in multiple studies in Gothenburg, Sweden since 1970.21, 22 Because stress at work and at home were highly intercorrelated, and because only 60% of participants were currently employed, we created a global stress scale that combined work and/or home stress that was graded as follows: 1, never experienced stress; 2, experienced some periods at home or at work; 3, experienced several periods at home or at work; and 4, experienced permanent stress at home or at work.
Level of financial stress was defined as follows: 1, little/none; 2, moderate; and 3, high/severe. The occurrence of major adverse life events was documented by asking participants whether they had experienced any of a number of specified life events in the past year (marital separation/divorce, loss of job/retirement, loss of crop/business failure, violence, major intrafamily conflict, major personal injury or illness, death/major illness of a close family, death of a spouse, or other major stress).
Depression was assessed by asking whether, during the past 12 months, the participant had felt sad, ‘blue’ or depressed for ⩾2 weeks in a row, and if yes, graded by a set of seven questions with no/yes answers (lose interest in things, feel tired or low on energy, gain or lose weight, trouble falling asleep, trouble concentrating, think of death, feeling worthless), where five or more positive responses were defined as clinical depression. This questionnaire is an adaptation of the short form Diagnostic and Statistical Manual of Mental Disorders-IV Composite International Diagnostic Interview questionnaire for depression.23
Statistical analysis
Continuous variables were summarized with means and standard deviations and categorical variables were summarized with numbers and percentages. Country income, age, sex and rural/urban location standardized means and proportions of risk factors were compared across different categories of global stress and depression status using the whole PURE population as the referent. Tests for trend and heterogeneity were performed for ordinal and nominal variables, respectively.
As the prevalence of obesity was fairly high in this population, the prevalence ratio (PR) was directly estimated using the log binomial regression model.24 The generalized estimating equation was used to account for correlation within communities.
Three models were fitted to assess the effect of psychosocial factors on obesity. First, the model was adjusted for age, sex and PA. Second, the model was further adjusted for education. The final model was adjusted for all the factors included in the previous models and region.
Statistical analyses and figures were generated with SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) and R version 2.12.2 (R Foundation for Statistical Computing, Vienna, Austria). The 95% confidence intervals (CIs) for each psychosocial factor are also reported. All statistical tests for the null hypothesis are two sided. Owing to sparse data in some cells, estimates for Africa could not be provided.
The study was approved by institutional review boards at each participating institution. All participants provided informed consent.
Results
Supplementary Table 1 shows key variables by region for the 125 290 subjects who provided data on psychosocial variables. Mean age was 50.7 (s.d. 9.6) years, 56.8% were women and 45.9% were from rural locations. Mean BMI ranged from 23.3 (s.d. 5.2) kg m−2 in South Asia to 28.2 (s.d. 5.7)kg m−2 in Latin America, with the proportion who were obese (BMI ⩾30%) ranging from 7.1% in China to 30.9% in Latin America. Mean WHR ranged from 0.84 (s.d. 0.09) in Africa to 0.91 (s.d. 0.08) in the Middle East. Approximately two-thirds of participants (66.0%) had experienced at least some stress during the past 12 months, and 19.1% were categorized as depressed.
Characteristics of individuals according to their level of global stress or depression
There was a strong relationship between global stress and country income status (Figure 1). Table 1 shows the characteristics of individuals according to their level of global stress (at work or at home). Only 23.9% of those who had never experienced stress were from HIC/UMIC, compared with 68.1% and 55.5% of those with several periods of stress, or permanent stress, respectively (P<0.0001). The proportion living in rural communities decreased slightly with increasing levels of stress from 47.6 to 38.5% (P<0.0001). Among those with no stress, 35.6% had ⩽8 years of education, compared with 47.3% among those with permanent stress (standardized estimates; P<0.0001).
After standardization for age, sex, country income and rural/urban location, both obesity- and ethnicity-specific central obesity increased moderately with increasing levels of stress. Among those who had never experienced stress, 15.7% were obese compared with 20.5% among those with permanent stress (P<0.0001). Corresponding standardized rates for sex- and ethnicity-specific central obesity were 48.6% and 53.5%, respectively. There were significant but numerically minor inverse relationships between stress and diabetes, and BP, and positive small associations for tobacco and alcohol use. The relation between stress and hypertension was quite flat, although the slightly inverse trend was significant due to the large numbers. People with high levels of stress were more physically active, and consumed slightly fewer calories but made less healthy food choices.
Those with depression were more often from HIC/UMIC (56.6% vs 37.8%) and had fewer years of education; 46.5% of those with depression had ⩽8 years of education, compared with 39.7% among non-depressed (standardized rates; P<0.0001) (Table 2). Depressed people had a slightly higher prevalence of obesity (standardized rate 21.0% vs 17.4%). There was no relationship between depression and hypertension, and a negative relationship between depression and systolic BP. There was a numerically small but significant increase in the prevalence of diabetes among those with depression (10.6% vs 9.8%; P<0.0001). People with depression used alcohol and tobacco more often and had slightly less healthy food choices, but did not have a higher mean caloric intake.
Association between psychosocial factors and general and abdominal obesity in multivariable and region-stratified analyses
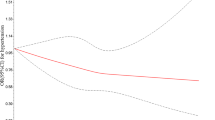
The global stress measure—combining work and home stress—was associated with a slightly higher PR of being obese (PR 1.06; 95% CI: 1.01–1.11 for several periods of stress and PR 1.07; 95% CI: 1.02–1.13 for permanent stress) after adjustment for age, sex and PA (Table 3). Further adjustment for education left estimates essentially unchanged. Adding adjustment for geographical region nullified the association between stress and obesity (PR 1.04; 95% CI: 0.99–1.10 for permanent stress). Depression was associated with higher rates of obesity even after adjustment for education and region (PR 1.08; 95% CI: 1.04–1.12). Because China has a different cutoff for obesity (>28 kg m−2), we repeated the analyses, redefining obesity in Chinese participants. However, estimates for both stress and depression remained unchanged (PR 1.03; 95% CI: 0.98–1.08 for permanent stress and 1.09; 95% CI 1.05–1.12 for depression, after adjustment). Restricting exposure to only work stress did not change estimates (PR 1.02; 95% CI: 0.95–1.09 for permanent stress). Central obesity was not associated with global stress, and only very marginally with depression (1.01; 95% CI: 1.00–1.03).
Figure 2 shows considerable heterogeneity across regions for the association between stress and obesity or central obesity. After adjustment for age, sex and PA, a small independent effect of stress on obesity persisted in Europe/North America (PR 1.13; 95% CI: 1.02–1.25). Conversely, a strong protective effect was found in South Asia, although the estimates were imprecise (PR 0.37; 95% CI: 0.11–1.23). No significant effect of stress on abdominal obesity was found in any region.
Region-specific relationships of depression with obesity and central obesity were also complex (Figure 3). Moderate or weak independent positive associations were found for both obesity and central obesity in Europe/North America, and in Latin America; however, only for general obesity in the latter.
Discussion
Our study did not support a strong independent link between psychosocial factors and obesity in this multiethnic and multicultural population from countries with varying economic development. People who admitted to high levels of stress or who were depressed were more likely to be obese; however, they were also more likely to live in regions with an obesity-promoting lifestyle, and in analyses stratified for region, there was no overall effect, although there were some exceptions, most notably for Europe/North America. Nevertheless, these associations were fairly weak. In general, the relationships with abdominal obesity were weaker than for general obesity, and relationships were weak, inverse or absent with diabetes or hypertension, two of the metabolic aberrations most strongly associated with abdominal obesity.
Findings in the context of the literature
It has been proposed that elements of modern society, with Westernization of diets, sedentary lifestyles and environmental stress, possibly induce obesity through dysregulation of the hypothalamic-pituitary-adrenal axis.2 According to this paradigm, a continuously changing and sometimes threatening external environment could, when the challenge exceeds a threshold, activate central pathways that stimulate the adrenal glands to release glucocorticoids,1, 3 with ensuing effects on fat distribution. However, although some support for this has been derived in studies of humans4 and in animal models,25 findings with respect to stress and obesity in humans have been mixed.
The most compelling evidence in favor of the stress obesity theory comes from the UK-based Whitehall study. During 19 years of follow-up of over 10 000 British civil servants, the incidence of obesity was related to the frequency of reports of job stress in a dose–response manner.8 Furthermore, in a previous study, a dose–response association was found to exist between exposure to work stress and the metabolic syndrome.9 Overall, work stress was associated with incident type 2 diabetes mellitus among women, but not among men.26 These effects were modified by the presence of obesity, with a lower risk of type 2 diabetes mellitus associated with stress in non-obese but not in obese men.27 Among women, work stress was associated with increased risk of type 2 diabetes mellitus in obese but not in non-obese individuals. A recent Swedish study of men found midlife stress to predict diabetes over a very extended follow-up into old age.28 Sex, age and body weight status, accordingly, seem to have a critical role in determining the direction of a potential association between psychosocial stress and type 2 diabetes mellitus.26, 27
Taken together, the investigations in the Whitehall studies8, 26, 27 indicate that, in particular, work stress may be implicated in the complex causal chain leading to obesity and to metabolic aberrations secondary to obesity. However, it is important to note these studies, albeit with designs including different social strata, were conducted in a limited cultural setting. A review of the associations between psychological workload and obesity, which summarized findings from 10 cross-sectional studies, all conducted in European or North-American populations, did not find support for any associations between work stress and either general or abdominal obesity.10 In a meta-analysis of 14 prospectively followed cohorts, psychosocial stress was shown to be a risk factor for weight gain, but the effects were very limited.11 In a meta-analysis of work-related stress and cardiovascular disease risk factors, job strain was linked to diabetes and weakly to obesity, but no association was observed between job strain, clinic BP or blood lipids.29 Again, all studies except one were conducted in Western populations. In the PURE study, Western populations showed a small increase in the risk of being obese in those with permanent stress, whereas there was a strong protective effect in South Asia. Although there is no reason to believe that the biological effects of stress differ between these regions, these heterogeneities raise questions on how to best assess stress in different cultural and political settings. However, setting aside the issue of whether stress is linked to obesity overall, there was no indication that stress is linked to abdominal obesity in any of the regions of the world, except possibly—albeit only very weakly—in Europe/North America.
The potential association between depression and obesity has been repeatedly examined, but usually in cross-sectional studies.30, 31, 32 Cross-sectional studies may not provide information on the causal link between depression and obesity,33 as they do not differentiate between depressed individuals being more liable to gain weight, either via unhealthy lifestyles or dysregulated stress systems,34, 35 and obesity causing depression, partly through being socially undesirable. Inflammation, which has a role in both obesity and depression,36, 37 could be another mediator, as could hypothalamic-pituitary-adrenal axis dysregulation,38 with obesity causing this dysregulation, as opposed to the theory where dysregulation caused by psychosocial factors affects body fat distribution. To shed further light on the potential bidirectional associations between depression and obesity, longitudinal studies are needed. In a recent systematic review and meta-analysis of 15 longitudinal studies,33 all conducted in Europe, the United States or New Zealand, it was concluded that depression and obesity interact reciprocally. Obesity at baseline increased the risk of onset of depression, whereas depression increased the odds of developing obesity by a substantial 58%.
In the PURE study, an independent but comparatively weak association persisted between depression and obesity, with the strongest effects in Europe/North America (PR 1.19). However, because this was a cross-sectional analysis, the direction of this association could not be assessed. With the exception of Europe/North America where there was a weak association (PR 1.06), there was no association between abdominal obesity and depression. The contrasting findings between different regions, specifically the findings for Western regions in PURE, are consistent with the conclusions of the meta-analysis,33 and also suggest that the association between depression and obesity is not ubiquitous, but is dependent on the cultural context.
Strengths and weaknesses
Studies with null findings, for example, where a hypothesized association cannot be verified, have to be scrutinized for poor characterization of exposure or outcome, and for poor study design. Our study has a number of limitations. First, stress and other psychosocial factors are difficult concepts, in that there is no consensus with respect to either definition or measurement. In addition, because they are subjective, they are also open to biases and confounding. The size of our study precluded the use of complicated instruments for the assessment of stress and depression. However, several studies, using the same stress questionnaire, have found strong and independent links with coronary heart disease,20, 22 as well as with stroke.16, 21 In the INTERHEART study,20 we found strong links between global stress and depression, and life events as well as financial stress, both of which are factors that may be perceived as external stressors and thus less likely to be influenced by subjective perceptions. Accordingly, although the methods that we used were relatively simple, we believe that they capture important dimensions of psychosocial problems. Second, although we used measured weight, height and waist circumferences to measure obesity, these are indirect measurements, and additionally were only measured at one time-point. However, these measures have been used in a number of studies on adverse health outcomes. Also, as both hypertension and diabetes were largely identified by self-report, there may be issues about how common the measurement of BP and blood glucose is in different countries, making the comparability of case ascertainment in these conditions somewhat doubtful. However, the associations between body weight and waist circumference, with both hypertension and diabetes, as expected, were very strong. Third, there are limitations that are inherent to all cross-sectional studies. Interpretation of cross-sectional studies is problematic because temporal sequence cannot always be determined. In this largely middle-aged sample, we found no or only weak or inconsistent, independent associations between psychosocial factors and obesity, but even so, weight gain could not be assessed. The strengths of the study include a very large sample, and one that is more representative of the global population than prior studies.
In conclusion, features of modern society include abundant availability of food for large segments of the population, along with reduced energy expenditure and more stress. Our study shows that, while there is a link between psychosocial factors and obesity, this is not very strong and is mainly explained by regional variation in both stress levels and obesity. Specifically, we found no evidence that abdominal obesity or its consequences (hypertension and diabetes) are more than at most minimally affected by stress or depression. The ongoing follow-up of the PURE study and other cohorts will provide further insights into the role of psychosocial factors on weight gain.
References
Bjorntorp P . Do stress reactions cause abdominal obesity and comorbidities? Obes Rev 2001; 2: 73–86.
Bose M, Olivan B, Laferrere B . Stress and obesity: the role of the hypothalamic-pituitary-adrenal axis in metabolic disease. Curr Opin Endocrinol Diabetes Obes 2009; 16: 340–346.
Rosmond R . Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology 2005; 30: 1–10.
Rosmond R, Dallman MF, Bjorntorp P . Stress-related cortisol secretion in men: relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab 1998; 83: 1853–1859.
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case–control study. Lancet 2005; 366: 1640–1649.
Mente A, Yusuf S, Islam S, McQueen MJ, Tanomsup S, Onen CL et al. Metabolic syndrome and risk of acute myocardial infarction a case–control study of 26,903 subjects from 52 countries. J Am Coll Cardiol 2010; 55: 2390–2398.
Ford ES . Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 2005; 28: 1769–1778.
Brunner EJ, Chandola T, Marmot MG . Prospective effect of job strain on general and central obesity in the Whitehall II study. Am J Epidemiol 2007; 165: 828–837.
Chandola T, Brunner E, Marmot M . Chronic stress at work and the metabolic syndrome: prospective study. BMJ 2006; 332: 521–525.
Overgaard D, Gyntelberg F, Heitmann BL . Psychological workload and body weight: is there an association? A review of the literature. Occup Med (Lond) 2004; 54: 35–41.
Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A . Stress and adiposity: a meta-analysis of longitudinal studies. Obesity (Silver Spring, MD) 2011; 19: 771–778.
Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet 2011; 378: 1231–1243.
MacQueen KM, McLellan E, Metzger DS, Kegeles S, Strauss RP, Scotti R et al. What is community? An evidence-based definition for participatory public health. Am J Public Health 2001; 91: 1929–1938.
Teo K, Lear S, Islam S, Mony P, Dehghan M, Li W et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: The Prospective Urban Rural Epidemiology (PURE) study. JAMA 2013; 309: 1613–1621.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet 2004; 364: 937–952.
O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case–control study. Lancet 2010; 376: 112–123.
World Health Organization. Definition, Diagnosis, and Classification of Diabetes Mellitus and its Complications: Report of a WHO Consultation. Part I: Diagnosis and Classification of Diabetes Mellitus. World Health Organization: Geneva, Switzerland, 1999.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395.
McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002; 76: 1261–1271.
Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case–control study. Lancet 2004; 364: 953–962.
Harmsen P, Rosengren A, Tsipogianni A, Wilhelmsen L . Risk factors for stroke in middle-aged men in Goteborg, Sweden. Stroke 1990; 21: 223–229.
Rosengren A, Tibblin G, Wilhelmsen L . Self-perceived psychological stress and incidence of coronary artery disease in middle-aged men. Am J Cardiol 1991; 68: 1171–1175.
Patten SB . Performance of the Composite International Diagnostic Interview Short Form for major depression in community and clinical samples. Chronic Dis Can 1997; 18: 109–112.
Wacholder S . Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol 1986; 123: 174–184.
Shively CA, Clarkson TB . Regional obesity and coronary artery atherosclerosis in females: a non-human primate model. Acta Med Scand Suppl 1988; 723: 71–78.
Heraclides A, Chandola T, Witte DR, Brunner EJ . Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes Care 2009; 32: 2230–2235.
Heraclides AM, Chandola T, Witte DR, Brunner EJ . Work stress, obesity and the risk of type 2 diabetes: gender-specific bidirectional effect in the Whitehall II study. Obesity (Silver Spring) 2012; 20: 428–433.
Novak M, Bjorck L, Giang KW, Heden-Stahl C, Wilhelmsen L, Rosengren A . Perceived stress and incidence of type 2 diabetes: a 35-year follow-up study of middle-aged Swedish men. Diabet Med 2013; 30: e8–e16.
Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, Casini A, Clays E et al. Job strain and cardiovascular disease risk factors: meta-analysis of individual-participant data from 47 000 men and women. PLoS One 2013; 8: e67323.
de Wit LM, van Straten A, van Herten M, Penninx BW, Cuijpers P . Depression and body mass index, a u-shaped association. BMC Public Health 2009; 9: 14.
Faith MS, Matz PE, Jorge MA . Obesity-depression associations in the population. J Psychosom Res 2002; 53: 935–942.
Scott KM, McGee MA, Wells JE, Oakley Browne MA . Obesity and mental disorders in the adult general population. J Psychosom Res 2008; 64: 97–105.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010; 67: 220–229.
Stunkard AJ, Faith MS, Allison KC . Depression and obesity. Biol Psychiatry 2003; 54: 330–337.
Bornstein SR, Schuppenies A, Wong ML, Licinio J . Approaching the shared biology of obesity and depression: the stress axis as the locus of gene–environment interactions. Mol Psychiatry 2006; 11: 892–902.
Bremmer MA, Beekman AT, Deeg DJ, Penninx BW, Dik MG, Hack CE et al. Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord 2008; 106: 249–255.
Shoelson SE, Herrero L, Naaz A . Obesity, inflammation, and insulin resistance. Gastroenterology 2007; 132: 2169–2180.
Holsboer F . The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology 2000; 23: 477–501.
Acknowledgements
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Rosengren, A., Teo, K., Rangarajan, S. et al. Psychosocial factors and obesity in 17 high-, middle- and low-income countries: the Prospective Urban Rural Epidemiologic study. Int J Obes 39, 1217–1223 (2015). https://doi.org/10.1038/ijo.2015.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.48
This article is cited by
-
The multiple roles of life stress in metabolic disorders
Nature Reviews Endocrinology (2023)
-
The perceived role of food and eating among Turkish women with obesity: A qualitative analysis
Current Psychology (2022)
-
Beyond weight: examining the association of obesity with cardiometabolic related inpatient costs among Canadian adults using linked population based survey and hospital administrative data
BMC Health Services Research (2021)
-
Work Stress as a Risk Factor for Cardiovascular Disease
Current Cardiology Reports (2015)