Abstract
Background:
Risk of cardiovascular and metabolic disease is higher in adults who were relatively thin at birth and had subsequent accelerated weight gain. This specific pattern of weight gain may relate to unfavorable cardiometabolic markers already in childhood. We prospectively assessed whether children with different patterns of overweight development from age 3 months to 11 years had distinct levels of cardiometabolic markers at age 12 years.
Subjects/Methods:
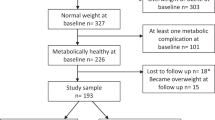
We used data of 1500 children participating in the PIAMA birth cohort that started in 1996/1997. Parents reported height and weight during 10 waves of follow-up from age 3 months to 11 years. Four distinct overweight development patterns were derived using longitudinal latent class analysis; ‘never’; ‘early transient’; ‘gradually developing’ and ‘persistent’ overweight. Cardiometabolic markers (total-to-high-density lipoprotein cholesterol (TC/HDLC) ratio, blood pressure (BP), glycated hemoglobin (HbA1c)) were assessed at age 12 years in 1500 children.
Results:
Children who developed overweight gradually and children with persistent overweight throughout childhood, at age 12 years had a 2–3-fold higher risk of having high (>90th centile) TC/HDLC ratio, systolic and diastolic BP, compared with children who were never overweight. In children who gradually developed overweight, TC/HDLC ratio was 0.75 higher (95% confidence interval (CI) 0.54–0.96); systolic BP 4.90 mmHg higher (95% CI 2.45–7.36) and diastolic BP 1.78 mmHg higher (95% CI 0.07–3.49) than in children who never had overweight. Estimates for children with persistent overweight were similar.
Conclusions:
Children with gradually developing overweight, and those with persistent overweight had unfavorable cholesterol and blood pressure levels already at age 12 years, whereas children with early transient overweight avoided these unfavorable outcomes. Our results support the hypothesis that specific overweight patterns predispose to an adverse cardiometabolic profile, which is already apparent in early adolescence before progressing to adult cardiometabolic disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Barker DJ . The developmental origins of chronic adult disease. Acta Paediatr Suppl 2004; 93: 26–33.
Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG . Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005; 353: 1802–1809.
Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004; 350: 865–875.
Park MH, Sovio U, Viner RM, Hardy RJ, Kinra S . Overweight in childhood, adolescence and adulthood and cardiovascular risk in later life: pooled analysis of three british birth cohorts. PloS One 2013; 8: e70684.
Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011; 364: 1315–1325.
Belfort MB, Gillman MW . Healthy infant growth: what are the trade-offs in the developed world? Nestle Nutr Inst Workshop Ser 2013; 71: 171–184.
Regnault N, Gillman MW . Importance of characterizing growth trajectories. Ann Nutr Metab 2014; 65: 110–113.
Sovio U, Kaakinen M, Tzoulaki I, Das S, Ruokonen A, Pouta A et al. How do changes in body mass index in infancy and childhood associate with cardiometabolic profile in adulthood? Findings from the Northern Finland Birth Cohort 1966 Study. Int J Obes (Lond) 2014; 38: 53–59.
van Rossem L, Wijga AH, Brunekreef B, de Jongste JC, Kerkhof M, Postma DS et al. Overweight in infancy: which pre- and perinatal factors determine overweight persistence or reduction? A birth cohort followed for 11 years. Ann Nutr Metab 2014; 65: 211–219.
Wijga AH, Kerkhof M, Gehring U, de Jongste JC, Postma DS, Aalberse RC et al. Cohort profile: the prevention and incidence of asthma and mite allergy (PIAMA) birth cohort. Int J Epidemiol 2014; 43: 527–535.
Fredriks AM, van Buuren S, Burgmeijer RJ, Meulmeester JF, Beuker RJ, Brugman E et al. Continuing positive secular growth change in the Netherlands 1955-1997. Pediatr Res 2000; 47: 316–323.
Bekkers MB, Brunekreef B, Scholtens S, Kerkhof M, Smit HA, Wijga AH . Parental reported compared with measured waist circumference in 8-year-old children. Int J Pediatr Obes 2011; 6: e78–e86.
Scholtens S, Brunekreef B, Visscher TL, Smit HA, Kerkhof M, de Jongste JC et al. Reported versus measured body weight and height of 4-year-old children and the prevalence of overweight. Eur J Public Health 2007; 17: 369–374.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 2005; 45: 142–161.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Petersen AC, Crockett L, Richards M, Boxer A . A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc 1988; 17: 117–133.
Ayer J, Charakida M, Deanfield JE, Celermajer DS . Lifetime risk: childhood obesity and cardiovascular risk. Eur Heart J 2015; 36: 1371–1376.
Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation 2009; 119: 628–647.
Jaddoe VW, de Jonge LL, Hofman A, Franco OH, Steegers EA, Gaillard R . First trimester fetal growth restriction and cardiovascular risk factors in school age children: population based cohort study. BMJ 2014; 348: g14.
Drake AJ, Reynolds RM . Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction 2010; 140: 387–398.
Rooney K, Ozanne SE . Maternal over-nutrition and offspring obesity predisposition: targets for preventative interventions. Int J Obes (Lond) 2011; 35: 883–890.
Huang RC, de Klerk NH, Smith A, Kendall GE, Landau LI, Mori TA et al. Lifecourse childhood adiposity trajectories associated with adolescent insulin resistance. Diabetes Care 2011; 34: 1019–1025.
Travers SH, Jeffers BW, Bloch CA, Hill JO, Eckel RH . Gender and Tanner stage differences in body composition and insulin sensitivity in early pubertal children. J Clin Endocrinol Metab 1995; 80: 172–178.
Patton GC, Viner R . Pubertal transitions in health. Lancet 2007; 369: 1130–1139.
Tinggaard J, Mieritz MG, Sorensen K, Mouritsen A, Hagen CP, Aksglaede L et al. The physiology and timing of male puberty. Curr Opin Endocrinol Diabetes Obes 2012; 19: 197–203.
Singhal A, Lucas A . Early origins of cardiovascular disease: is there a unifying hypothesis? Lancet 2004; 363: 1642–1645.
Ziyab AH, Karmaus W, Kurukulaaratchy RJ, Zhang H, Arshad SH . Developmental trajectories of Body Mass Index from infancy to 18 years of age: prenatal determinants and health consequences. J Epidemiol Community Health 2014; 68: 934–941.
Ventura AK, Loken E, Birch LL . Developmental trajectories of girls' BMI across childhood and adolescence. Obesity (Silver Spring) 2009; 17: 2067–2074.
Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PloS One 2011; 6: e27608.
Acknowledgements
We gratefully acknowledge the contribution of all participating children and parents or caregivers of the PIAMA study. We thank Ada Wolse, Marjan Tewis and Marieke Oldenwening for their contribution to the data collection and data management. This work was supported by the National Institute for Public Health and the Environment (grant number S/260306/01/PA). The Prevention and Incidence of Asthma and Mite Allergy Study was funded by grants from the Netherlands Organisation for Health Research and Development; the Netherlands Asthma Foundation; the Netherlands Ministry of Planning, Housing and the Environment; the Netherlands Ministry of Health, Welfare and Sport; and the Institute for Public Health and the Environment. The study sponsors had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author contributions
Ms Berentzen and Dr van Rossem conceptualized and designed the study, carried out the initial analyses, drafted and revised the manuscript, and approved the final manuscript as submitted. Dr Smit and Dr Wijga conceptualized and designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Drs Gehring, Koppelman, Postma and de Jongste critically reviewed the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Berentzen, N., van Rossem, L., Gehring, U. et al. Overweight patterns throughout childhood and cardiometabolic markers in early adolescence. Int J Obes 40, 58–64 (2016). https://doi.org/10.1038/ijo.2015.196
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.196
This article is cited by
-
Tracking of serum lipids in healthy children on a year-to-year basis
BMC Cardiovascular Disorders (2023)