Abstract
Objectives:
Obesity and depression have become prevalent pregnancy complications, individually associated with adverse perinatal health outcomes. Despite the co-prevalence of these two risk factors, their combined effects on maternal health are yet to be studied. The objective of this study was to examine the combined associations of overweight/obesity and depression with maternal and delivery complications.
Methods:
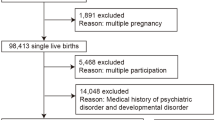
A retrospective cohort study of women with singleton gestations at >20 weeks, in Ontario, Canada (April 2007 to March 2010), was conducted. Our primary outcomes were a composite of maternal complications (for example, gestational hypertension, pre-eclampsia, preterm premature rupture of membranes and so on), and a composite of delivery complications (for example, caesarean delivery, shoulder dystocia, postpartum haemorrhage and so on).
Results:
The study population consisted of 70 605 women, of whom 50.3% were overweight/obese. Depression was reported in 5.0% of normal-weight women and 6.2% of overweight/obese women. The proportion of women with maternal complications was the highest among the overweight/obese depressed pregnant women (16% of normal-weight non-depressed, 22% of normal-weight depressed, 22% of overweight/obese non-depressed and 29% of overweight/obese depressed, P<0.001), as was the proportion of women with delivery complications (44%, 49%, 50% and 53%, respectively, P<0.001). Overweight/obese depressed pregnant women also experienced the highest odds of the composite of maternal complications and the composite of delivery complications (adjusted odds ratio (OR): 1.55, 95% confidence interval (CI): 1.35–1.77 and OR: 1.27, 95% CI: 1.13–1.42, respectively) after adjustment for potential confounders.
Conclusions:
The combined associations of excess weight and depression with adverse pregnancy outcomes are important to recognize in order to focus counselling and care, both before and during pregnancy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Health Canada. Prenatal Nutrition Guidelines for Health Professionals: Gestational Weight Gain (Internet). 2014 (updated 29 December 2014; cited 25 May 2015). Available from http://www.hc-sc.gc.ca/fn-an/nutrition/prenatal/ewba-mbsa-eng.php.
Public Health Agency of Canada. Depression in Pregnancy (Internet). 2012 (updated 3 May 2012; cited 25 May 2015). Available from http://www.phac-aspc.gc.ca/mh-sm/preg_dep-eng.php.
Chu SY, Callaghan WM, Kim SY, Schmid CH, Lau J, England LJ et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care 2007; 30: 2070–2076.
O'Brien TE, Ray JG, Chan WS . Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology 2003; 14: 368–374.
Poobalan AS, Aucott LS, Gurung T, Smith WC, Bhattacharya S . Obesity as an independent risk factor for elective and emergency caesarean delivery in nulliparous women—systematic review and meta-analysis of cohort studies. Obes Rev 2009; 10: 28–35.
Bhattacharya S, Campbell DM, Liston WA, Bhattacharya S . Effect of body mass index on pregnancy outcomes in nulliparous women delivering singleton babies. BMC Public Health 2007; 7: 168.
Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O . Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol 2000; 95: 487–490.
McDonald SD, McKinney B, Foster G, Taylor V, Lutsiv O, Pullenayegum E . The combined effects of high maternal weight and depression on neonatal outcomes: a retrospective cohort study. Int J Obes (Lond) e-pub ahead of print 30 March 2015; doi:10.1038/ijo.2015.44.
Bodnar LM, Wisner KL, Moses-Kolko E, Sit DK, Hanusa BH . Prepregnancy body mass index, gestational weight gain, and the likelihood of major depressive disorder during pregnancy. J Clin Psychiatry 2009; 70: 1290–1296.
von EE, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–1457.
BORN Ontario. Better Outcomes Registry and Network (BORN) Ontario (Internet). 2011. Available from https://www.bornontario.ca (last accessed 25 July 2011).
Perinatal Partnership Program of Eastern and Southeastern Ontario (PPPESO). Annual Perinatal Statistical Report 2006-07 [Internet]. 2007. Available from https://www.nidaydatabase.com/info/pdf/200607AnnualReportFinal.pdf (last accessed 11 July 2011).
Dunn S, Bottomley J, Ali A, Walker M . 2008 Niday Perinatal Database quality audit: report of a quality assurance project. Chronic Dis Inj Can 2011; 32: 32–42.
Statistics Canada. Postal Code Conversion File (PCCF) 2006 Reference Guide (Internet). 2007 (updated 30 Jan 2007; cited 5 July 2011). Available from http://www.statcan.gc.ca/pub/92f0153g/92f0153g2007001-eng.pdf.
Rubin DB . Multiple Imputation for Nonresponse in Surveys. Wiley: New York, 1987.
Little RJA, Rubin DB . Statistical Analysis with Missing Data. 2nd edn. Wiley: New York, 2002.
Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH et al. Obesity, obstetric complications and cesarean delivery rate—a population-based screening study. Am J Obstet Gynecol 2004; 190: 1091–1097.
Baeten JM, Bukusi EA, Lambe M . Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health 2001; 91: 436–440.
Lu GC, Rouse DJ, DuBard M, Cliver S, Kimberlin D, Hauth JC . The effect of the increasing prevalence of maternal obesity on perinatal morbidity. Am J Obstet Gynecol 2001; 185: 845–849.
Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord 2001; 25: 1175–1182.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ . A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010; 67: 1012–1024.
Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT . Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med 2001; 63: 830–834.
Huttunen R, Syrjanen J . Obesity and the risk and outcome of infection. Int J Obes (Lond) 2013; 37: 333–340.
Denison FC, Roberts KA, Barr SM, Norman JE . Obesity, pregnancy, inflammation, and vascular function. Reproduction 2010; 140: 373–385.
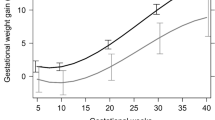
Nohr EA, Bech BH, Vaeth M, Rasmussen KM, Henriksen TB, Olsen J . Obesity, gestational weight gain and preterm birth: a study within the Danish National Birth Cohort. Paediatr Perinat Epidemiol 2007; 21: 5–14.
Goldenberg RL, Hauth JC, Andrews WW . Intrauterine infection and preterm delivery. N Engl J Med 2000; 342: 1500–1507.
Wolf M, Kettyle E, Sandler L, Ecker JL, Roberts J, Thadhani R . Obesity and preeclampsia: the potential role of inflammation. Obstet Gynecol 2001; 98: 757–762.
Madan JC, Davis JM, Craig WY, Collins M, Allan W, Quinn R et al. Maternal obesity and markers of inflammation in pregnancy. Cytokine 2009; 47: 61–64.
Zhang J, Bricker L, Wray S, Quenby S . Poor uterine contractility in obese women. BJOG 2007; 114: 343–348.
Teixeira JM, Fisk NM, Glover V . Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based study. BMJ 1999; 318: 153–157.
Orpana AK, Avela K, Ranta V, Viinikka L, Ylikorkala O . The calcium-dependent nitric oxide production of human vascular endothelial cells in preeclampsia. Am J Obstet Gynecol 1996; 174: 1056–1060.
Bosio PM, McKenna PJ, Conroy R, O'Herlihy C . Maternal central hemodynamics in hypertensive disorders of pregnancy. Obstet Gynecol 1999; 94: 978–984.
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK et al. A meta-analysis of cytokines in major depression. Biol Psychiatry 2010; 67: 446–457.
Walker JJ . Antioxidants and inflammatory cell response in preeclampsia. Semin Reprod Endocrinol 1998; 16: 47–55.
Sandman CA, Wadhwa PD, Chicz-DeMet A, Dunkel-Schetter C, Porto M . Maternal stress, HPA activity, and fetal/infant outcome. Ann N Y Acad Sci 1997; 814: 266–275.
Nagahawatte NT, Goldenberg RL . Poverty, maternal health, and adverse pregnancy outcomes. Ann N Y Acad Sci 2008; 1136: 80–85.
Norbeck JS, Tilden VP . Life stress, social support, and emotional disequilibrium in complications of pregnancy: a prospective, multivariate study. J Health Soc Behav 1983; 24: 30–46.
Chochinov HM, Wilson KG, Enns M, Lander S . ‘Are you depressed?’ Screening for depression in the terminally ill. Am J Psychiatry 1997; 154: 674–676.
Whooley MA, Avins AL, Miranda J, Browner WS . Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med 1997; 12: 439–445.
Gosse MA . How accurate is self-reported BMI? Nutr Bull 2014; 39: 105–114.
Acknowledgements
This work was supported by a Regional Medical Association (RMA) grant and SDM is supported by the Canadian Institutes of Health Research (CIHR) New Investigator Award CNI 95357. RMA and CIHR had no role in the design and conduct of the study, collection, management, analysis and interpretation of the data, and preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lutsiv, O., McKinney, B., Foster, G. et al. Pregnancy complications associated with the co-prevalence of excess maternal weight and depression. Int J Obes 39, 1710–1716 (2015). https://doi.org/10.1038/ijo.2015.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.119
This article is cited by
-
The effect of antenatal depression on birth weight among newborns in South Gondar zone, Northwest Ethiopia: a population-based prospective cohort study
Archives of Public Health (2021)
-
Making therapies culturally relevant: translation, cultural adaptation and field-testing of the Thinking Healthy Programme for perinatal depression in China
BMC Pregnancy and Childbirth (2020)
-
Provider volume and maternal complications after Caesarean section: results from a population-based study
BMC Pregnancy and Childbirth (2020)
-
Antenatal predictors of incident and persistent postnatal depressive symptoms in rural Ethiopia: a population-based prospective study
Reproductive Health (2019)
-
Maternal body mass index moderates antenatal depression effects on infant birthweight
Scientific Reports (2019)