Abstract
Objective:
Epigenetic alterations have been suggested to be associated with obesity and related metabolic disorders. Here we examined the correlation between obesity and insulin resistance with the methylation frequency of the leptin (LEP) and adiponectin (ADIPOQ) promoters in obese adolescents with the aim to identify epigenetic markers that might be used as tools to predict and follow up the physiological alterations associated with the development of the metabolic syndrome.
Subjects:
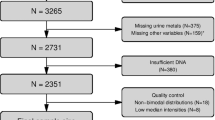
One hundred and six adolescents were recruited and classified according to body mass index and homeostasis model of assessment-insulin resistance index. The circulating concentrations of leptin, adiponectin and of several metabolic markers of obesity and insulin resistance were determined by standard methods. The methylation frequency of the LEP and ADIPOQ promoters was determined by methylation-specific PCR (MS-PCR) in DNA obtained from peripheral blood samples.
Results:
Obese adolescents without insulin resistance showed higher and lower circulating levels of, respectively, leptin and adiponectin along with increased plasmatic concentrations of insulin and triglycerides. They also exhibited the same methylation frequency than lean subjects of the CpG sites located at −51 and −31 nt relative to the transcription start site of the LEP gene. However, the methylation frequency of these nucleotides dropped markedly in obese adolescents with insulin resistance. We found the same inverse relationship between the combined presence of obesity and insulin resistance and the methylation frequency of the CpG site located at −283 nt relative to the start site of the ADIPOQ promoter.
Conclusions:
These observations sustain the hypothesis that epigenetic modifications might underpin the development of obesity and related metabolic disorders. They also validate the use of blood leukocytes and MS-PCR as a reliable and affordable methodology for the identification of epigenetic modifications that could be used as molecular markers to predict and follow up the physiological changes associated with obesity and insulin resistance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Balkau B, Charles MA, Drivsholm T, Borch-Johnsen K, Wareham N, Yudkin JS et al. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab 2002; 28: 364–376.
European Commission. Strategy for Europe on nutrition, overweight and obesity related health issues – Implementation Progress Report 2010. Brussels: European Commission; 2010. http://ec.europa.eu/health/nutrition_physical_activity/docs/implementation_report_en.pdf).
Flegal KM, Carroll MD, Ogden CL, Curtin LR . Prevalence and trends in obesity among us adults, 1999-2008. JAMA 2010; 303: 235–241.
Rivera JA, Barquera S, Campirano F, Campos I, Safdie M, Tovar V . Epidemiological and nutritional transition in Mexico: rapid increase of non-communicable chronic diseases and obesity. Public Health Nutr 2002; 5: 113–122.
Popkin BM, Adair LS, Ng SW . Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012; 70: 3–21.
Zimmet P, Alberti KGMM, Shaw J . Global and societal implications of the diabetes epidemic. Nature 2001; 414: 782–787.
Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 2005; 111: 1999–2012.
Reilly JJ, Kelly J . Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood. Systematic review. Int J Obes (Lond) 2011; 35: 891–898.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH . Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997; 337: 869–873.
Perea-Martinez A, Carbajal RL, Rodriguez HR, Zarco RJ, Barrios FR, Loredo AA . Association of comorbidity with obesity in Mexican children and adolescents. Pediatrics 2008; 121: S149–S150.
Loos RJF, Bouchard C . Obesity-is it a genetic disorder? J Intern Med 2003; 254: 401–425.
Wilborn C, Beckham J, Campbell B, Harvey T, Galbreath M, La Bounty P et al. Obesity: prevalence, theories, medical consequences, management, and research directions. J Int Soc Sports Nutr 2005; 2: 4–31.
Miao F, Gonzalo IG, Lanting L, Natarajan R . In vivo chromatin remodeling events leading to inflammatory gene transcription under diabetic conditions. J Biol Chem 2004; 279: 18091–18097.
Kuehnen P, Mischke M, Wiegand S, Sers C, Horsthemke B, Lau S et al. An Alu element-associated hypermethylation variant of the POMC gene is associated with childhood obesity. PLoS Genet 2012; 8: e1002543.
Zhao J, Goldberg J, Vaccarino V . Promoter methylation of serotonin transporter gene is associated with obesity measures: a monozygotic twin study. Int J Obes (Lond) 2013; 37: 140–145.
Crujeiras AB, Campion J, Díaz-Lagares A, Milagro FI, Goyenechea E, Abete I et al. Association of weight regain with specific methylation levels in the NPY and POMC promoters in leukocytes of obese men: a translational study. Regul Pept 2013; 186: 1–6.
Bouchard L, Rabasa-Lhoret R, Faraj M, Lavoie ME, Mill J, Pérusse L et al. Differential epigenomic and transcriptomic responses in subcutaneous adipose tissue between low and high responders to caloric restriction. Am J Clin Nutr 2010; 91: 309–320.
Moleres A, Campión J, Milagro FI, Marcos A, Campoy C, Garagorri JM et al. Differential DNA methylation patterns between high and low responders to a weight loss intervention in overweight or obese adolescents: the EVASYON study. FASEB J 2013; 27: 2504–2512.
Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1995; 1: 1155–1161.
Considine RV, Considine EL, Williams CJ, Hyde TM, Caro JF . The hypothalamic leptin receptor in humans: identification of incidental sequence polymorphisms and absence of the db/db mouse and fa/fa rat mutations. Diabetes 1996; 45: 992–994.
Schwartz MW, Prigeon RL, Kahn SE, Nicolson M, Moore J, Morawiecki A et al. Evidence that plasma leptin and insulin levels are associated with body adiposity via different mechanisms. Diabetes Care 1997; 20: 1476–1481.
Kadowaki T, Yamauchi Y, Kubota N, Hara K, Ueki K, Tobe K . Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 2006; 116: 1784–1792.
Stefan N, Bunt JC, Salbe AD, Funahashi T, Matsuzawa Y, Tataranni PA . Plasma adiponectin concentrations in children: relationships with obesity and insulinemia. J Clin Endocrinol Metab 2002; 87: 4652–4656.
Gilardini L, McTernana PG, Girola A, da Silva NF, Alberti L, Kumar S et al. Adiponectin is a candidate marker of metabolic syndrome in obese children and adolescents. Atherosclerosis 2006; 189: 401–407.
García-Cuartero B, García-Lacalle C, Jiménez-Lobo C, González-Vergaz A, Calvo-Rey C, Alcázar-Villar MJ et al. Índice HOMA y QUICKI, insulina y peptido C en niños sanos. Puntos de corte de riesgo cardiovascular. An Pediatr (Barc) 2007; 66: 481–490.
Melzner I, Scott V, Dorsch K, Fischer P, Wabitsch M, Brüderlein S et al. Leptin gene expression in human preadipocytes is switched on by maturation-induced demethylation of distinct CpGs in its proximal promoter. J Biol Chem 2002; 277: 45420–45427.
Stöger R . In vivo methylation patterns of the leptin promoter in human and mouse. Epigenetics 2006; 1: 155–162.
Noer A, Boquest AC, Collas P . Dynamics of adipogenic promoter DNA methylation during clonal culture of human adipose stem cells to senescence. BMC Cell Biol 2007; 8: 18.
Sorensen AL, Jacobsen BM, Reiner AH, Andersen IS, Collas P . Promoter DNA methylation patterns of differentiated cells are largely programmed at the progenitor stage. Mol Biol Cell 2010; 21: 2066–2077.
Marchi M, Lisi S, Curcio M, Barbuti S, Piaggi P, Ceccarini G et al. Human leptin tissue distribution, but not weight loss-dependent change in expression, is associated with methylation of its promoter. Epigenetics 2011; 6: 1198–1206.
Naveh-Many T, Cedar H . Active gene sequences are undermethylated. Proc Natl Acad Sci USA 1981; 78: 4246–4250.
Bouchard L, Hivert MF, Guay SP, St-Pierre J, Perron P, Brisson D . Placental adiponectin gene DNA methylation levels are associated with mother'blood glucose concentration. Diabetes 2012; 61: 1272–1280.
Lavon I, Refael M, Zelikovitch B, Shalom E, Siegal T . Serum DNA can define tumor-specific genetic and epigenetic markers in gliomas of various grades. Neuro Oncol 2010; 12: 173–180.
Ally MS, Al-Ghnaniem R, Pufulete M . The relationship between gene-specific DNA methylation in leukocytes and normal colorectal mucosa in subjects with and without colorectal tumors. Cancer Epidemiol Biomarkers Prev 2009; 18: 922–928.
Pack SC, Kim HR, Lim SW, Kim HY, Ko JY, Lee KS et al. Usefulness of plasma epigenetic changes of five major genes involved in the pathogenesis of colorectal cancer. Int J Colorectal Dis 2013; 28: 139–147.
Cortese R, Kwan A, Lalonde E, Bryzgunova O, Bondar A, Wu Y et al. Epigenetic markers of prostate cancer in plasma circulating DNA. Hum Mol Genet 2012; 21: 3619–3631.
Yamagishi SI, Edelstein D, Du XL, Kaneda Y, Guzmán M, Brownlee M . Leptin induces mitochondrial superoxide production and monocyte chemoattractant protein-1 expression in aortic endothelial cells by increasing fatty acid oxidation via protein kinase A. J Biol Chem 2001; 276: 25096–25100.
Bouloumie A, Marumo T, Lafontan M, Busse R . Leptin induces oxidative stress in human endothelial cells. FASEB J 1999; 13: 1231–1238.
Rahmouni K . Leptin-induced sympathetic nerve activation: signaling mechanisms and cardiovascular consequences in obesity. Curr Hypertens Rev 2010; 6: 104–209.
Acknowledgements
The authors thank the Mexican adolescents and their parents for their participation in the study. We also thank José Alfredo Pérez Ontiveros, Emma Guadalupe Gazcón Morales, Daniel Chavez Vazquez and Sergio Arturo Mavil Cortes for their help with blood sample collection and laboratory measures. We thank Dr. Alfonso Reyes López for his help in analysis. This work was supported by ICyT-DF, SIP-IPN, COFAA-IPN, HIM/2012/002, and CONACyT, Mexico.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
García-Cardona, M., Huang, F., García-Vivas, J. et al. DNA methylation of leptin and adiponectin promoters in children is reduced by the combined presence of obesity and insulin resistance. Int J Obes 38, 1457–1465 (2014). https://doi.org/10.1038/ijo.2014.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.30
Keywords
This article is cited by
-
Circulating adiponectin levels, expression of adiponectin receptors, and methylation of adiponectin gene promoter in relation to Alzheimer’s disease
BMC Medical Genomics (2022)
-
Methylation of the LEP gene promoter in blood at 12 months and BMI at 4 years of age—a population-based cohort study
International Journal of Obesity (2020)
-
Oleic acid influences the adipogenesis of 3T3-L1 cells via DNA Methylation and may predispose to obesity and obesity-related disorders
Lipids in Health and Disease (2019)
-
Epigenome-wide association study in peripheral white blood cells involving insulin resistance
Scientific Reports (2019)
-
Maternal corticotropin-releasing hormone is associated with LEP DNA methylation at birth and in childhood: an epigenome-wide study in Project Viva
International Journal of Obesity (2019)