Abstract
Background/Objectives:
The Sibutramine Cardiovascular OUTcomes (SCOUT) trial showed a significantly increased relative risk of nonfatal cardiovascular events, but not mortality, in overweight and obese subjects receiving long-term sibutramine treatment with diet and exercise. We examined the relationship between early changes (both increases and decreases) in pulse rate, and the impact of these changes on subsequent cardiovascular outcome events in both the placebo and sibutramine groups.
Subjects/Methods:
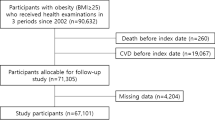
9804 males and females, aged ⩾55 years, with a body mass index of 27–45 kg m−2 were included in this current subanalysis of the SCOUT trial. Subjects were required to have a history of cardiovascular disease and/or type 2 diabetes mellitus with at least one cardiovascular risk factor, to assess cardiovascular outcomes. The primary outcome event (POE) was a composite of nonfatal myocardial infarction, nonfatal stroke, resuscitated cardiac arrest or cardiovascular death. Time-to-event analyses of the POE were performed using Cox regression models.
Results:
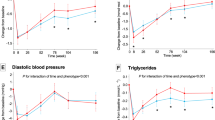
During the initial 6-week sibutramine treatment period, the induced pulse rate increase was related to weight change (1.9±7.7 beats per minute (bpm) with weight increase; 1.4±7.3 bpm, 0–5 kg weight loss; 0.6±7.4 bpm, ⩾5 kg weight loss). Throughout the subsequent treatment period, those continuing on sibutramine showed a consistently higher mean pulse rate than the placebo group. There was no difference in POE rates with either an increase or decrease in pulse rate over the lead-in period, or during lead-in baseline to 12 months post randomization. There was also no relationship between pulse rate at lead-in baseline and subsequent cardiovascular events in subjects with or without a cardiac arrhythmia.
Conclusion:
Baseline pulse rate and changes in pulse rate may not be an important modifier nor a clinically useful predictor of outcome in an individual elderly cardiovascular obese subject exposed to weight management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood pressure 2009; 18: 308–347.
Kannel WB, Sorlie P . Hypertension in Framingham. In: Paul O (ed). Epidemiology and Control of Hypertension. Stratton Intercontinental Medical Book Corp: New York, NY, USA, 1975. pp 553–592.
Diaz A, Bourassa MG, Guertin MC, Tardif JC . Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J 2005; 26: 967–974.
Kolloch R, Legler UF, Champion A, Cooper-Dehoff RM, Handberg E, Zhou Q et al. Impact of resting heart rate on outcomes in hypertensive patients with coronary artery disease: findings from the INternational VErapamil-SR/trandolapril STudy (INVEST). Eur Heart J 2008; 29: 1327–1334.
Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R . Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet 2008; 372: 817–821.
Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R . Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med 2014; 371: 1091–1099.
Swedberg K, Komajda M, Bohm M, Borer JS, Ford I, Dubost-Brama A et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010; 376: 875–885.
Fox K, Komajda M, Ford I, Robertson M, Bohm M, Borer JS et al. Effect of ivabradine in patients with left-ventricular systolic dysfunction: a pooled analysis of individual patient data from the BEAUTIFUL and SHIFT trials. Eur Heart J 2013; 34: 2263–2270.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur Heart J 2007; 28: 2375–2414.
Snow V, Barry P, Fitterman N, Qaseem A, Weiss K . Pharmacologic and surgical management of obesity in primary care: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2005; 142: 525–531.
Lean M, Finer N . ABC of obesity management: part II—drugs. BMJ 2006; 333: 794–797.
Halford JC, Boyland EJ, Cooper SJ, Dovey TM, Huda MS, Dourish CT et al. The effects of sibutramine on the microstructure of eating behaviour and energy expenditure in obese women. J Psychopharmacol 2010; 24: 99–109.
Heusser K, Tank J, Diedrich A, Engeli S, Klaua S, Kruger N et al. Influence of sibutramine treatment on sympathetic vasomotor tone in obese subjects. Clin Pharmacol Ther 2006; 79: 500–508.
Lechin F, van der Dijs B, Hernandez G, Orozco B, Rodriguez S, Baez S . Neurochemical neuroautonomic and neuropharmacological acute effects of sibutramine in healthy subjects. Neurotoxicology 2006; 27: 184–191.
James WP, Caterson ID, Coutinho W, Finer N, Van Gaal LF, Maggioni AP et al. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med 2010; 363: 905–917.
Seimon RV, Espinoza D, Ivers L, Gebski V, Finer N, Legler UF et al. Changes in body weight and blood pressure: paradoxical outcome events in overweight and obese subjects with cardiovascular disease. Int J Obes (Lond) 2014; 38: 1165–1171.
James WPT . The SCOUT study: risk-benefit profile of sibutramine in overweight high-risk cardiovascular patients. Eur Heart J Suppl 2005; 7: L44–L48.
Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J, Izzo JL Jr et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation 2007; 115: 2761–2788.
Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation 2008; 118: 428–464.
Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 2011; 42: 227–276.
Ryden L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 2007; 28: 88–136.
Andrews TC, Fenton T, Toyosaki N, Glasser SP, Young PM, MacCallum G et al. Subsets of ambulatory myocardial ischemia based on heart rate activity. Circadian distribution and response to anti-ischemic medication. Circulation 1993; 88: 92–100.
Cooney MT, Vartiainen E, Laatikainen T, Juolevi A, Dudina A, Graham IM . Elevated resting heart rate is an independent risk factor for cardiovascular disease in healthy men and women. Am Heart J 2010; 159: 612–9 e3.
Fox K, Borer JS, Camm AJ, Danchin N, Ferrari R, Lopez Sendon JL et al. Resting heart rate in cardiovascular disease. J Am Coll Cardiol 2007; 50: 823–830.
Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G . Lower heart rate variability is associated with the development of coronary heart disease in individuals with diabetes: the atherosclerosis risk in communities (ARIC) study. Diabetes 2002; 51: 3524–3531.
Hillebrand S, Gast KB, de Mutsert R, Swenne CA, Jukema JW, Middeldorp S et al. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: meta-analysis and dose-response meta-regression. Europace 2013; 15: 742–749.
Dyer AR, Persky V, Stamler J, Paul O, Shekelle RB, Berkson DM et al. Heart rate as a prognostic factor for coronary heart disease and mortality: findings in three Chicago epidemiologic studies. Am J Epidemiol 1980; 112: 736–749.
Palatini P, Mos L, Santonastaso M, Zanatta N, Mormino P, Saladini F et al. Resting heart rate as a predictor of body weight gain in the early stage of hypertension. Obesity (Silver Spring) 2011; 19: 618–623.
Palatini P, Dorigatti F, Zaetta V, Mormino P, Mazzer A, Bortolazzi A et al. Heart rate as a predictor of development of sustained hypertension in subjects screened for stage 1 hypertension: the HARVEST Study. J Hypertens 2006; 24: 1873–1880.
US Food and Drug Administration. Proceedings of the Endocrinologic and Metabolic Drugs Advisory Committee Meeting. 1995: Silver Spring, MD: US Food and Drug Administration; 1995.
European Medicines Agency. Scientific conclusions and grounds for refusal. Available online http://www.emaeuropaeu/docs/en_GB/document_library/Other/human/002350/WC500147577pdf.
Robinson LE, Holt TA, Rees K, Randeva HS, O'Hare JP . Effects of exenatide and liraglutide on heart rate, blood pressure and body weight: systematic review and meta-analysis. BMJ open 2013; 3: e001986.
Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE maintenance randomized study. Int J Obes (Lond) 2013; 37: 1443–1451.
Astrup A, Carraro R, Finer N, Harper A, Kunesova M, Lean ME et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond) 2012; 36: 843–854.
Myat A, Redwood SR, Gersh BJ, Yellon DM, Marber MS . Diabetes, incretin hormones and cardioprotection. Heart 2014; 100: 1550–1561.
Picatoste B, Ramirez E, Caro-Vadillo A, Iborra C, Ares-Carrasco S, Egido J et al. Sitagliptin reduces cardiac apoptosis, hypertrophy and fibrosis primarily by insulin-dependent mechanisms in experimental type-II diabetes. Potential roles of GLP-1 isoforms. PloS One 2013; 8: e78330.
Wang D, Luo P, Wang Y, Li W, Wang C, Sun D et al. Glucagon-like peptide-1 protects against cardiac microvascular injury in diabetes via a cAMP/PKA/Rho-dependent mechanism. Diabetes 2013; 62: 1697–1708.
Acknowledgements
The original trial was supported and funded by Abbott Laboratories (Abbott Park, IL, USA). The Executive Steering Committee designed the study in cooperation with the sponsor. RVS was supported by a National Health and Medical Research Council of Australia Early Career Research Fellowship (no 1072771). We are also grateful to the Endocrine Society of Australia for a Postdoctoral Award to RVS.
Disclaimer
The authors have full access to all data, determined the analyses, are solely responsible for its interpretation and this manuscript without reference to the original sponsor and took the final decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
NF: member of SCOUT Executive Steering Committee (ESC) received payments from Abbott, as advisor for Novo Nordisk, Merck, sanofi-aventis, GlaxoSmithKline and Shionogi, consultant for Ajinomoto, and provided expert testimony for sanofi-aventis, Vivus, Arena and received a grant from GlaxoSmithKline. WPTJ: Chair of the SCOUT ESC received payment from Abbott; the International Association for the Study of Obesity when he was the President also received a grant from Novo Nordisk. UFL: was an employee of Abbott with equity interest in the Company. WC: member of the SCOUT ESC received payments from Abbott Laboratories, lecture fees and/or travel reimbursement from Abbott, Ache Laboratorios Farmaceuticos S/A, Roche and Novo Nordisk, as advisor for Abbott, Ache Laboratorios Farmaceuticos S/A, GSK, Novo Nordisk, Takeda and Roche, and provided expert testimony for Abbott. AMS: member of the SCOUT ESC received payment from Abbott Laboratories, and as advisor for Abbott, Merck, Arena, Novo Nordisk, sanofi-aventis, GlaxoSmithKline, Boehringer Ingelheim, and NeuroSearch, as consultant for Vivus and Allegan, provided expert testimony for GlaxoSmithKline, received grants from Abbott and Covidian. LVG: Received a research grant from National Research Funds, Belgium; served on the speaker's bureaus of Sanofi-Aventis and Abbott; served as a consultant to Amylin Pharmaceuticals, Sanofi-Aventis, Eli Lilly, and Abbott; member of SCOUT ESC receiving payment from Abbott. IDC: member of SCOUT ESC received payment from Abbott Laboratories, royalties from Wiley-Blackwell as co-editor of an obesity textbook, and the Boden Institute of Obesity, Nutrition and Exercise received grants from Novo Nordisk, sanofi-aventis, Pfizer (Australia), Weight Watchers, Allergan and the Korean Ministry of Agriculture. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Seimon, R., Espinoza, D., Finer, N. et al. Changes in body weight and pulse: outcome events in overweight and obese subjects with cardiovascular disease in the SCOUT trial. Int J Obes 39, 849–857 (2015). https://doi.org/10.1038/ijo.2014.211
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.211
This article is cited by
-
Anti-obesity drug discovery: advances and challenges
Nature Reviews Drug Discovery (2022)