Abstract
Objective:
Limited knowledge exists on the long-term implications of maternal gestational weight gain (GWG) on offspring health. Our objective was to examine whether high GWG in normal weight women is associated with adult offspring cardio-metabolic risk factors.
Methods:
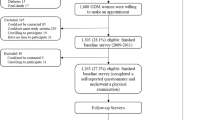
We used a cohort of 308 Danish women who gave birth in 1988–89 and whose offspring participated in a clinical examination at 20 years of age. Main outcome measures were offspring body mass index (BMI), waist circumference, weight-regulating hormones, blood lipids and glucose metabolism. Associations were assessed using multivariable linear and logistic regression models.
Results:
A weak positive association was observed between GWG during the first 30 weeks and offspring anthropometry. Each 1-kg increase in maternal GWG was associated with 0.1-kg m−2 higher (95% confidence interval (CI): 0.01, 0.2) offspring BMI and 10% (95% CI: 0.1%, 20%) higher odds of offspring overweight at the age of 20 years, with similar associations observed in both sexes. However, sex differences were observed for the association between maternal GWG and specific cardio-metabolic risk factors. Hence, a 1-kg increase in GWG was associated with 3.4% (95% CI; 0.8, 6.0%) higher homeostasis model assessment-estimated insulin resistance (HOMA-IR), 3.7% (95% CI: 1.4%, 6.2%) higher insulin and 10.7% (95% CI: 5.7%, 15.9%) higher leptin levels in male offspring. These associations were not observed in females, which may partly be explained by more frequent reports of dieting and physical exercise at follow-up among female offspring.
Conclusions:
In normal-weight women, high GWG may have modest long-term implications on offspring cardio-metabolic risk factors at adult age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gluckman PD, Hanson MA, Cooper C, Thornburg KL . Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 2008; 359: 61–73.
Ravelli AC, van Der Meulen JH, Osmond C, Barker DJ, Bleker OP . Obesity at the age of 50 y in men and women exposed to famine prenatally. Am J Clin Nutr 1999; 70: 811–816.
Drake AJ, Reynolds RM . Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction 2010; 140: 387–398.
Lillycrop KA, Burdge GC . Epigenetic changes in early life and future risk of obesity. Int J Obes (Lond) 2011; 35: 72–83.
Committee to Reexamine IOM Pregnancy Weight Guidelines. In: Institute of medicine, National research Consil. 2010/07/30 ed. National Academies Press: Washington DC, 2009.
Mamun AA, Mannan M, Doi SA . Gestational weight gain in relation to offspring obesity over the life course: a systematic review and bias-adjusted meta-analysis. Obes Rev 2014; 15: 338–347.
Nehring I, Lehmann S, von Kries R . Gestational weight gain in accordance to the IOM/NRC criteria and the risk for childhood overweight: a meta-analysis. Pediatr Obes 2013; 8: 218–224.
Deierlein AL, Siega-Riz AM, Adair LS, Herring AH . Effects of pre-pregnancy body mass index and gestational weight gain on infant anthropometric outcomes. J Pediatr 2011; 158: 221–226.
Whitaker RC . Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 2004; 114: e29–e36.
Gale CR, Javaid MK, Robinson SM, Law CM, Godfrey KM, Cooper C . Maternal size in pregnancy and body composition in children. J Clin Endocrinol Metab 2007; 92: 3904–3911.
Koupil I, Toivanen P . Social and early-life determinants of overweight and obesity in 18-year-old Swedish men. Int J Obes (Lond) 2008; 32: 73–81.
Hochner H, Friedlander Y, Calderon-Margalit R, Meiner V, Sagy Y, Avgil-Tsadok M et al. Associations of maternal prepregnancy body mass index and gestational weight gain with adult offspring cardiometabolic risk factors: the Jerusalem Perinatal Family Follow-up Study. Circulation 2012; 125: 1381–1389.
Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X . Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS One 2013; 8: e61627.
Patro B, Liber A, Zalewski B, Poston L, Szajewska H, Koletzko B . Maternal and paternal body mass index and offspring obesity: a systematic review. Ann Nutr Metab 2013; 63: 32–41.
Mamun AA, O'Callaghan M, Callaway L, Williams G, Najman J, Lawlor DA . Associations of gestational weight gain with offspring body mass index and blood pressure at 21 years of age: evidence from a birth cohort study. Circulation 2009; 119: 1720–1727.
von Kries R, Ensenauer R, Beyerlein A, Amann-Gassner U, Hauner H, Rosario AS . Gestational weight gain and overweight in children: Results from the cross-sectional German KiGGS study. Int J Pediatr Obes 2011; 6: 45–52.
Beyerlein A, Nehring I, Rzehak P, Heinrich J, Muller MJ, Plachta-Danielzik S et al. Gestational weight gain and body mass index in children: results from three german cohort studies. PLoS One 2012; 7: e33205.
Olsen SF, Hansen HS, Sandstrom B, Jensen B . Erythrocyte levels compared with reported dietary intake of marine n-3 fatty acids in pregnant women. Br J Nutr 1995; 73: 387–395.
Olsen SF, Hansen HS, Secher NJ, Jensen B, Sandstrom B . Gestation length and birth weight in relation to intake of marine n-3 fatty acids. Br J Nutr 1995; 73: 397–404.
Halldorsson TI, Rytter D, Haug LS, Bech BH, Danielsen I, Becher G et al. Prenatal exposure to perfluorooctanoate and risk of overweight at 20 years of age: a prospective cohort study. Environ Health Perspect 2012; 120: 668–673.
Christensen AI, Severin M, Holmberg T, Eriksen L, Toftager M, Zachariassen A et al KRAM-undersøgelsen i tal og billeder. Retrieved from http://www.si-folkesundhed.dk/upload/rapporten_kram_2010.pdf.
Fraser A, Tilling K, Macdonald-Wallis C, Sattar N, Brion MJ, Benfield L et al. Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation 2010; 121: 2557–2564.
Venn BJ, Williams SM, Perry T, Richardson S, Cannon A, Mann JI . Age-related differences in postprandial glycaemia and glycaemic index. Age Ageing 2011; 40: 755–758.
Aiken CE, Ozanne SE . Sex differences in developmental programming models. Reproduction 2013; 145: R1–13.
Samuelsson AM, Matthews PA, Argenton M, Christie MR, McConnell JM, Jansen EH et al. Diet-induced obesity in female mice leads to offspring hyperphagia, adiposity, hypertension, and insulin resistance: a novel murine model of developmental programming. Hypertension 2008; 51: 383–392.
Nivoit P, Morens C, Van Assche FA, Jansen E, Poston L, Remacle C et al. Established diet-induced obesity in female rats leads to offspring hyperphagia, adiposity and insulin resistance. Diabetologia 2009; 52: 1133–1142.
Thompson PD, Crouse SF, Goodpaster B, Kelley D, Moyna N, Pescatello L . The acute versus the chronic response to exercise. Med Sci Sports Exerc 2001; 33 (6 Suppl): S438–S445.
Warburton DE, Nicol CW, Bredin SS . Health benefits of physical activity: the evidence. CMAJ 2006; 174: 801–809.
Armitage JA, Taylor PD, Poston L . Experimental models of developmental programming: consequences of exposure to an energy rich diet during development. J Physiol 2005; 565 (Pt 1) 3–8.
Poston L . Gestational weight gain: influences on the long-term health of the child. Curr Opin Clin Nutr Metab Care 2012; 15: 252–257.
Ahima RS, Flier JS . Leptin. Annu Rev Physiol 2000; 62: 413–437.
Geisthovel F, Jochmann N, Widjaja A, Horn R, Brabant G . Serum pattern of circulating free leptin, bound leptin, and soluble leptin receptor in the physiological menstrual cycle. Fertil Steril 2004; 81: 398–402.
Lederman SA, Paxton A . Maternal reporting of prepregnancy weight and birth outcome: consistency and completeness compared with the clinical record. Matern Child Health J 1998; 2: 123–126.
Brunner Huber LR . Validity of self-reported height and weight in women of reproductive age. Matern Child Health J 2007; 11: 137–144.
Acknowledgements
We acknowledge the financial support of the Danish Council for Strategic Research. The present study was supported by the Danish Council for Strategic Research (Grant no.: 09-067124 (Centre for Fetal Programming), 2101-07-0025 (Danish Centre for Obesity Research) and 2101-06-0005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Hrolfsdottir, L., Rytter, D., Olsen, S. et al. Gestational weight gain in normal weight women and offspring cardio-metabolic risk factors at 20 years of age. Int J Obes 39, 671–676 (2015). https://doi.org/10.1038/ijo.2014.179
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.179
This article is cited by
-
The effect of motivational interviewing and/or cognitive behaviour therapy techniques on gestational weight gain – a systematic review and meta-analysis
BMC Public Health (2023)
-
What is an appropriate gestational weight gain for women with gestational diabetes mellitus: based on the adverse pregnancy outcomes of over 12 thousand participants?
Diabetology & Metabolic Syndrome (2022)
-
Exploring women’s thoughts on self-weighing during pregnancy: results of the Self-Weighing in Pregnancy: Experiences (SWIPE) study
BMC Pregnancy and Childbirth (2021)
-
Maternal nutrition and its intergenerational links to non-communicable disease metabolic risk factors: a systematic review and narrative synthesis
Journal of Health, Population and Nutrition (2021)
-
Maternal obesity: focus on offspring cardiometabolic outcomes
International Journal of Obesity Supplements (2020)