Abstract
Background/objectives:
Levels of pediatric obesity continue to rise. Previous evidence has linked short sleep duration and/or poor sleep quality to obesity development, although objective data are limited. As adolescents transition through puberty, circadian shifts occur, resulting in sleep loss. However, little is known whether chronotype is associated with body mass index (BMI) or dietary behaviors in adolescents. We hypothesized late chronotype would be positively associated with BMI and poorer dietary behaviors.
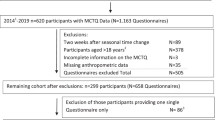
Subjects/methods:
A total of 511 UK young adolescents (11–13 years) from eight secondary schools across the Midlands region (UK) participated in the Midlands Adolescent Schools Sleep Education Study (MASSES), a cross-sectional study to assess potential relationships between chronotype and BMI z-score as well as dietary habits. Height (cm) and weight (kg) were objectively measured for BMI calculation and participants completed a questionnaire to assess dietary habits. A subsample of 236 adolescents wore wrist actigraphy for 7 days to estimate average sleep duration (weekday, weekend and combined) and sleep efficiency.
Results:
Definitely evening chronotype was positively associated with BMI z-score compared to definitely morning chronotypes β=0.51, P<0.01, after adjustment. Higher frequency of consuming unhealthy snacks, night-time caffeine consumption and inadequate daily intake of fruit/vegetables were also associated with later chronotype (all P⩽0.01). Actigraphy estimated sleep duration was an independent predictor of BMI z-score β=−0.36, P<0.001. Sleep efficiency did not predict BMI z-score after adjustment, β=−0.03, P=0.07.
Conclusions:
Later chronotype young adolescents are at risk of increased BMI and poorer dietary behaviors. Although short sleep duration, but not sleep efficiency, was also an independent risk factor for increased BMI, different mechanisms may be driving the late chronotype and shorter sleep duration associations with BMI in this age group. Sleep hygiene education may help adolescents to better understand the impact of sleeping habits on physical health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Haslam DW, James WP . Obesity. Lancet 2005; 366: 1197–1209.
Taheri S, Lin L, Austin D, Young T, Mignot E . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004; 1: e62.
Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ . The association between self-reported sleep quality and overweight in a Chinese population. Obesity (Silver Spring) 2013; 21: 486–492.
Gonnissen HK, Rutters F, Mazuy C, Martens EA, Adam TC, Westerterp-Plantenga MS . Effect of a phase advance and phase delay of the 24-h cycle on energy metabolism, appetite, and related hormones. Am J Clin Nutr 2012; 96: 689–697.
Buxton OM, Cain SW, O'Connor SP, Porter JH, Duffy JF, Wang W et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 2012; 4: 129ra43.
Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL et al. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care 2013; 36: 2523–2529.
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD . Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr 2009; 89: 126–133.
Herichova I . Changes of physiological functions induced by shift work. Endocr Regul 2013; 47: 159–170.
Tarokh L, Raffray T, Van Reen E, Carskadon MA . Physiology of normal sleep in adolescents. Adolesc Med State Art Rev 2010; 21: 401–417 vii.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C . Social jetlag and obesity. Curr Biol 2012; 22: 939–943.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141: 846–850.
Chaput JP, Despres JP, Bouchard C, Tremblay A . Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity (Silver Spring) 2007; 15: 253–261.
Spaeth AM, Dinges DF, Goel N . Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep 2013; 36: 981–990.
Chaput JP, Tremblay A . Does short sleep duration favor abdominal adiposity in children? Int J Pediatr Obes 2007; 2: 188–191.
Guidolin M, Gradisar M . Is shortened sleep duration a risk factor for overweight and obesity during adolescence? A review of the empirical literature. Sleep Med 2012; 13: 779–786.
Culnan E, Kloss JD, Grandner M . A prospective study of weight gain associated with chronotype among college freshmen. Chronobiol Int 2013; 30: 682–690.
Spilsbury JC, Drotar D, Rosen CL, Redline S . The Cleveland adolescent sleepiness questionnaire: a new measure to assess excessive daytime sleepiness in adolescents. J Clin Sleep Med 2007; 3: 603–612.
Mori K, Mitsuki F, Nishi C, Yoshida T, Kawasaki A, Kondon H et al. Usefulness of a Tri-Axis Accelerometer for Sleep-Wake Scoring. World Sleep Meeting 2011. Japan2011.
Cellini N, Buman MP, McDevitt EA, Ricker AA, Mednick SC . Direct comparison of two actigraphy devices with polysomnographically recorded naps in healthy young adults. Chronobiol Int 2013; 30: 691–698.
Horne JA, Ostberg O . A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 1976; 4: 97–110.
Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003; 26: 213–216.
Sun Y, Sekine M, Kagamimori S . Lifestyle and overweight among Japanese adolescents: the Toyama Birth Cohort Study. J Epidemiol 2009; 19: 303–310.
Stea TH, Knutsen T, Torstveit MK . Association between short time in bed, health-risk behaviors and poor academic achievement among Norwegian adolescents. Sleep Med 2014; 15: 666–671.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA . Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 2009; 106: 4453–4458.
Knutson KL, Lauderdale DS . Sleep duration and overweight in adolescents: self-reported sleep hours versus time diaries. Pediatrics 2007; 119: e1056–e1062.
Calamaro CJ, Park S, Mason TB, Marcus CL, Weaver TE, Pack A et al. Shortened sleep duration does not predict obesity in adolescents. J Sleep Res 2010; 19: 559–566.
Gupta NK, Mueller WH, Chan W, Meininger JC . Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol 2002; 14: 762–768.
Chung KF, Cheung MM . Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep 2008; 31: 185–194.
Knutson KL . Sex differences in the association between sleep and body mass index in adolescents. J Pediatr 2005; 147: 830–834.
Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN, Taheri S . The complexity of obesity in UK adolescents: relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatr Obes 2012; 8: 358–366.
St-Onge MP, O'Keeffe M, Roberts AL, RoyChoudhury A, Laferrere B . Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep 2012; 35: 1503–1510.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S . The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep 2010; 33: 1201–1209.
Beebe DW, Simon S, Summer S, Hemmer S, Strotman D, Dolan LM . Dietary intake following experimentally restricted sleep in adolescents. Sleep 2013; 36: 827–834.
Klingenberg L, Chaput JP, Holmback U, Visby T, Jennum P, Nikolic M et al. Acute sleep restriction reduces insulin sensitivity in adolescent boys. Sleep 2013; 36: 1085–1090.
Reilly JJ, Dorosty AR . Epidemic of obesity in UK children. Lancet 1999; 354: 1874–1875.
Acknowledgements
We are grateful to all participating adolescents. We thank Mona Campbell at the Heart of England Foundation Trust for excellent management support. Participating schools were Abbot Beyne School, Bordesley Green Girls School, Bablake School, Droitwich Spa High School, Foremarke Hall School, Hamstead Hall Community Learning Centre, Repton School, Solihull School and Sutton Coldfield Grammar School for Girls. We thank all teaching staff for their support, in particular Denise Gould, Sue Hughes, Louise Yates, Chris Seeley, Ami Hands, Richard Merriman, Ian Clarkson, Denyse Price, Jess Sheridan and Claire Horne. We thank all parents who agreed for their children to participate and students who assisted with the project. Financial support for the study was provided by the children’s charity, Action Medical Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Arora, T., Taheri, S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes 39, 39–44 (2015). https://doi.org/10.1038/ijo.2014.157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.157
This article is cited by
-
Alignment between timing of ‘highest caloric intake’ and chronotype in relation to body composition during adolescence: the DONALD Study
European Journal of Nutrition (2024)
-
Associations between social loneliness trajectories and chronotype among adolescents
European Child & Adolescent Psychiatry (2024)
-
Chronotype is associated with eating behaviors, physical activity and overweight in school-aged children
Nutrition Journal (2023)
-
Shorter sleep among adolescents is associated with lower fruit and vegetable consumption the following day
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
Is chronotype linked with adherence to the Mediterranean diet among adolescents? The EHDLA study
Pediatric Research (2023)