Abstract
Background:
Reduced sleep duration has been increasingly reported to predict obesity. However, timing and regularity of sleep may also be important. In this study, the cross-sectional association between objectively measured sleep patterns and obesity was assessed in two large cohorts of older individuals.
Methods:
Wrist actigraphy was performed in 3053 men (mean age: 76.4 years) participating in the Osteoporotic Fractures in Men Study and 2985 women (mean age: 83.5 years) participating in the Study of Osteoporotic Fractures. Timing and regularity of sleep patterns were assessed across nights, as well as daytime napping.
Results:
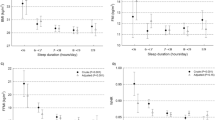
Greater night-to-night variability in sleep duration and daytime napping were associated with obesity independent of mean nocturnal sleep duration in both men and women. Each 1 h increase in the standard deviation of nocturnal sleep duration increased the odds of obesity 1.63-fold (95% confidence interval: 1.31–2.02) among men and 1.22-fold (95% confidence interval: 1.01–1.47) among women. Each 1 h increase in napping increased the odds of obesity 1.23-fold (95% confidence interval: 1.12–1.37) in men and 1.29-fold (95% confidence interval: 1.17–1.41) in women. In contrast, associations between later sleep timing and night-to-night variability in sleep timing with obesity were less consistent.
Conclusions:
In both older men and women, variability in nightly sleep duration and daytime napping were associated with obesity, independent of mean sleep duration. These findings suggest that characteristics of sleep beyond mean sleep duration may have a role in weight homeostasis, highlighting the complex relationship between sleep and metabolism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Flegal KM, Carroll MD, Kit BK, Ogden CL . Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012; 307: 491–497.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL . Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998; 22: 39–47.
Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA et al. The association between sleep duration and obesity in older adults. Int J Obes 2008; 32: 1825–1834.
Baron KG, Reid KJ, Kern AS, Zee PC . Role of sleep timing in caloric intake and BMI. Obesity 2011; 19: 1374–1381.
Spruyt K, Molfese DL, Gozal D . Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics 2011; 127: e345–e352.
Stone KL, Ewing SK, Ancoli-Israel S, Ensrud KE, Redline S, Bauer DC et al. Self-reported sleep and nap habits and risk of mortality in a large cohort of older women. J Am Geriatr Soc 2009; 57: 604–611.
Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA 1990; 263: 665–668.
Blank JB, Cawthon PM, Carrion-Petersen ML, Harper L, Johnson JP, Mitson E et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp Clin Trials 2005; 26: 557–568.
Orwoll E, Blank JB, Barrett-Connor E, Cauley J, Cummings S, Ensrud K et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials 2005; 26: 569–585.
Blackwell T, Redline S, Ancoli-Israel S, Schneider JL, Surovec S, Johnson NL et al. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep 2008; 31: 283–291.
Blackwell T, Ancoli-Israel S, Redline S, Stone KL . Factors that may influence the classification of sleep-wake by wrist actigraphy: the MrOS Sleep Study. J Clin Sleep Med 2011; 7: 357–367.
Action-W User's Guide, Version 2.0. Ardsley, NY, USA: Ambulatory Monitoring Inc.
Girardin JL, Kripke DF, Mason WJ, Elliot JA, Youngstedt SD . Sleep estimation from wrist movement quantified by different actigraphic modalities. J Neurosci Methods 2001; 105: 185–191.
Blackwell T, Ancoli-Israel S, Gehrman PR, Schneider JL, Pedula KL, Stone KL . Actigraphy scoring reliability in the study of osteoporotic fractures. Sleep 2005; 28: 1599–1605.
Martin SK, Eastman CI . Sleep logs of young adults with self-selected sleep times predict the dim light melatonin onset. Chronobiol Int 2002; 19: 695–707.
Barone JJ, Roberts HR . Caffeine consumption. Food Chem Toxicol 1996; 34: 119–129.
Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P . Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 1994; 10: 405–411.
Sheikh JI, Yesavage JA . Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986; 5: 165–173.
Washburn RA, Smith KW, Jette AM, Janney CA . The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993; 46: 153–162.
Teng EL, Chui HC . The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry 1987; 48: 314–318.
Folstein MF, Robins LN, Helzer JE . The Mini-Mental State Examination. Arch Gen Psychiatry 1983; 40: 812.
Ware JE, Kosinski M, Keller SD . SF-12: How to score the SF-12 Physical and Mental Health Summary Scores. 3rd edn. QualityMetric Incorporated: Lincoln, RI, USA, 1998.
Rechtschaffen A, Kales A . A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. US Government Printing Office: Washington, DC, USA, 1968.
Carter PJ, Taylor BJ, Williams SM, Taylor RW . Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ 2011; 342: d2712.
Spiegel K, Tasali E, Leproult R, Van Cauter E . Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol 2009; 5: 253–261.
Patel SR, Hu FB . Short sleep duration and weight gain: a systematic review. Obesity 2008; 16: 643–653.
Wing YK, Li SX, Li AM, Zhang J, Kong AP . The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics 2009; 124: e994–e1000.
Stone MR, Stevens D, Faulkner GE . Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Prev Med 2013; 56: 112–117.
Sierra-Johnson J, Unden AL, Linestrand M, Rosell M, Sjogren P, Kolak M et al. Eating meals irregularly: a novel environmental risk factor for the metabolic syndrome. Obesity 2008; 16: 1302–1307.
Timlin MT, Pereira MA, Story M, Neumark-Sztainer D . Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008; 121: e638–e645.
van der Heijden AA, Hu FB, Rimm EB, van Dam RM . A prospective study of breakfast consumption and weight gain among U.S. men. Obesity 2007; 15: 2463–2469.
Woo J, Cheung B, Ho S, Sham A, Lam TH . Influence of dietary pattern on the development of overweight in a Chinese population. Eur J Clin Nutr 2008; 62: 480–487.
Coakley EH, Rimm EB, Colditz G, Kawachi I, Willett W . Predictors of weight change in men: results from the Health Professionals Follow-up Study. Int J Obes Relat Metab Disord 1998; 22: 89–96.
Shi SQ, Ansari TS, McGuinness OP, Wasserman DH, Johnson CH . Circadian disruption leads to insulin resistance and obesity. Curr Biol 2013; 23: 372–381.
Barclay JL, Husse J, Bode B, Naujokat N, Meyer-Kovac J, Schmid SM et al. Circadian desynchrony promotes metabolic disruption in a mouse model of shiftwork. PLoS One 2012; 7: e37150.
Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science 2005; 308: 1043–1045.
Di Lorenzo L, De Pergola G, Zocchetti C, L'Abbate N, Basso A, Pannacciulli N et al. Effect of shift work on body mass index: results of a study performed in 319 glucose-tolerant men working in a Southern Italian industry. Int J Obes Relat Metab Disord 2003; 27: 1353–1358.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C . Social jetlag and obesity. Curr Biol 2012; 22: 939–943.
Wittmann M, Dinich J, Merrow M, Roenneberg T . Social jetlag: misalignment of biological and social time. Chronobiol Int 2006; 23: 497–509.
Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL et al. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care 2013; 36: 2523–2529.
Harb A, Levandovski R, Oliveira C, Caumo W, Allison KC, Stunkard A et al. Night eating patterns and chronotypes: a correlation with binge eating behaviors. Psychiatry Res 2012; 200: 489–493.
Colles SL, Dixon JB, O'Brien PE . Night eating syndrome and nocturnal snacking: association with obesity, binge eating and psychological distress. Int J Obes 2007; 31: 1722–1730.
Guan Z, Vgontzas AN, Bixler EO, Fang J . Sleep is increased by weight gain and decreased by weight loss in mice. Sleep 2008; 31: 627–633.
Vgontzas AN, Bixler EO, Tan TL, Kantner D, Martin LF, Kales A . Obesity without sleep apnea is associated with daytime sleepiness. Arch Intern Med 1998; 158: 1333–1337.
McDonald RJ, Zelinski EL, Keeley RJ, Sutherland D, Fehr L, Hong NS . Multiple effects of circadian dysfunction induced by photoperiod shifts: Alterations in context memory and food metabolism in the same subjects. Physiol Behav 2013; 118: 14–24.
Acknowledgements
This work was supported by National Institutes of Health grant HL098297. The Osteoporotic Fractures in Men (MrOS) Study was supported by National Institutes of Health funding. The following institutes provided support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR) and NIH Roadmap for Medical Research under the following grant numbers: U01 AR045580, U01 AR045614, U01 AR045632, U01 AR045647, U01 AR045654, U01 AR045583, U01 AG018197, U01 AG027810 and UL1 TR000128. The National Heart, Lung, and Blood Institute (NHLBI) provided funding for the MrOS Sleep ancillary study ‘Outcomes of Sleep Disorders in Older Men’ under the following grant numbers: HL071194, HL070848, HL070847, HL070842, HL070841, HL070837, HL070838 and HL070839. The SOF was supported by National Institutes of Health funding. The National Institute on Aging (NIA) provided support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574 and R01 AG027576.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Patel, S., Hayes, A., Blackwell, T. et al. The association between sleep patterns and obesity in older adults. Int J Obes 38, 1159–1164 (2014). https://doi.org/10.1038/ijo.2014.13
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.13
Keywords
This article is cited by
-
Bedtime regularity predicts positive affect among veterans with posttraumatic stress disorder: an ecological momentary assessment study
BMC Psychiatry (2023)
-
The relationship between daytime napping and obesity: a systematic review and meta-analysis
Scientific Reports (2023)
-
Obesity indicators as mediators of association between daytime napping and type 2 diabetes mellitus: the Guangzhou Biobank Cohort Study
BMC Public Health (2022)
-
Association between irregular daily routine and risk of incident stroke and coronary heart disease in a large Japanese population
Scientific Reports (2022)
-
Profiling of Sleep Models Based on Voluntary and Involuntary Sleep in Adults with Type 2 Diabetes
Sleep and Vigilance (2022)