Abstract
Objectives:
Obesity and stress are independently associated with decrements in neuromuscular functions. The present study examined the interplay of obesity and stress on neuromuscular fatigue and associated heart rate variability (HRV).
Methods:
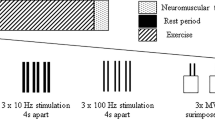
Forty-eight non-obese (18.5<body mass index (BMI)<25 kg m−2) and obese (30⩽BMI) adults performed repetitive handgrip exertions at 30% of their maximum strength until exhaustion in the absence and presence of a mental arithmetic stressor. Dependent measures included gold standard fatigue indicators (endurance time and rate of strength loss), perceived effort and mental demand, heart rate and temporal (RMSSD: root mean square of successive differences between N–N intervals) and spectral (LF/HF: ratio of low to high frequency) indices of HRV.
Results:
Stress negatively affected endurance time (P<0.0001) and rate of strength loss (P=0.029). In addition, significant obesity × stress interactions were found on endurance time (P=0.0073), rate of strength loss (P=0.027) and perceived effort (P=0.026), indicating that stress increased fatigability, particularly in the obese group. Both obesity (P=0.001) and stress (P=0.033) independently lowered RMSSD. Finally, stress increased LF/HF ratio (P=0.028) and the interaction of stress and obesity (P=0.008) indicated that this was augmented in the obese group.
Discussion:
The present study provides the first evidence that stress-related neuromuscular fatigue development is accelerated in obese individuals. In addition, the stress condition resulted in poorer HRV indices, which is indicative of autonomic dysfunction, particularly in the obese group. These findings indicate that workers are more susceptible to fatigue in high-stress work environments, particularly those with higher BMI, which can increase the risk of musculoskeletal injuries as well as cardiovascular diseases in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Flegal KM, Carroll MD, Ogden CL, Curtin LR . Prevalence and trends in obesity among US adults, 1999-2008. Jama 2010; 303: 235–241.
Finkelstein EA, Burgess SM, Hale BC . The costs of obesity in the workplace. J Occup Env Med 2010; 52: 971.
Sartorio A, Proietti M, Marinone P, Agosti F, Adorni F, Lafortuna C . Influence of gender, age and BMI on lower limb muscular power output in a large population of obese men and women. Int J obes 2004; 28: 91–98.
Houston DK, Ding J, Nicklas BJ, Harris TB, Lee JS, Nevitt MC et al. Overweight and Obesity Over the Adult Life Course and Incident Mobility Limitation in Older Adults. The Health, Aging and Body Composition Study. Am J Epidemiol 2009; 169: 927–936.
Mehta RK, Cavuoto LA . The effects of obesity, age, and relative workload levels on handgrip endurance. Appl Ergon; e-pub ahead of print 31 July 2014; doi:10.1016/j.apergo.2014.07.007.
Hilton TN, Tuttle LJ, Bohnert KL, Mueller MJ, Sinacore DR . Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Physical Therapy 2008; 88: 1336–1344.
Maffiuletti NA, Jubeau M, Munzinger U, Bizzini M, Agosti F, De Col A et al. Differences in quadriceps muscle strength and fatigue between lean and obese subjects. Eur J Appl Physiol 2007; 101: 51–59.
Østbye T, Dement JM, Krause KM . Obesity and workers' compensation: results from the Duke Health and Safety Surveillance System. Arch Intern Med 2007; 167: 766–773.
Kern PA, Simsolo RB, Fournier M . Effect of weight loss on muscle fiber type, fiber size, capillarity, and succinate dehydrogenase activity in humans 1. J Clin Endocrinol Metab 1999; 84: 4185–4190.
Tanner CJ, Barakat HA, Dohm GL, Pories WJ, MacDonald KG, Cunningham PRG et al. Muscle fiber type is associated with obesity and weight loss. Am J Physiol EndocrinolMetab 2002; 282: E1191–E1196.
Mehta RK, Shortz A . Obesity-related differences in neural correlates of force control. Eur J Appl Physiol 2014; 114: 197–204.
Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM et al. Work, obesity, and occupational safety and health. Am J Public Health 2007; 97: 428–436.
Nishitani N, Sakakibara H . Relationship of obesity to job stress and eating behavior in male Japanese workers. Int J Obesity 2006; 30: 528–533.
Weber A, Fussler C, O'Hanlon JF, Gierer R, Grandjean E . Psychophysiological effects of repetitive tasks. Ergonomics 1980; 23: 1033–1046.
Kivimäki M, Head J, Ferrie J, Shipley M, Brunner E, Vahtera J et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obesity 2006; 30: 982–987.
Mehta RK, Agnew MJ . Effects of concurrent physical and mental demands for a short duration static task. Int J Ind Ergon 2011; 41: 488–493.
Mehta RK, Agnew MJ . Exertion-dependent effects of physical and mental workload on physiological outcomes and task performance. IIE Trans Occup 2012; 1: 3–15.
Mehta RK, Nussbaum MA, Agnew MJ . Muscle- and task-dependent responses to concurrent physical and mental workload during intermittent static work. Ergonomics 2012; 59: 1166–1179.
Mehta RK, Agnew MJ . Influence of mental workload on muscle endurance, fatigue, and recovery during intermittent static work. Eur J Appl Physiol 2012; 112: 2891–2902.
Marcora SM, Staiano W, Manning V . Mental fatigue impairs physical performance in humans. J Appl Physiol 2009; 106: 857–864.
Melin B, Lundberg U . A biopsychosocial approach to work-stress and musculoskeletal disorders. J Psychophysiol 1997; 11: 238–247.
Kuper H, Singh-Manoux A, Siegrist J, Marmot M . When reciprocity fails: effort–reward imbalance in relation to coronary heart disease and health functioning within the Whitehall II study. Occup Environ Med 2002; 59: 777–784.
Kivimäki M, Virtanen M, Elovainio M, Kouvonen A, Väänänen A, Vahtera J . Work stress in the etiology of coronary heart disease—a meta-analysis. Scand J Work Environ Health 2006; 32: 431–442.
Stanek KM, Grieve SM, Brickman AM, Korgaonkar MS, Paul RH, Cohen RA et al. Obesity Is Associated With Reduced White Matter Integrity in Otherwise Healthy Adults*. Obesity 2011; 19: 500–504.
Gentier I, D’Hondt E, Shultz S, Deforche B, Augustijn M, Hoorne S et al. Fine and gross motor skills differ between healthy-weight and obese children. Res Dev Disab 2013; 34: 4043–4051.
Wolf PA, Beiser A, Elias MF, Au R, Vasan RS, Seshadri S . Relation of obesity to cognitive function: importance of central obesity and synergistic influence of concomitant hypertension. The Framingham Heart Study. Curr Alzheimer Res 2007; 4: 111–116.
Lallukka T, Laaksonen M, Martikainen P, Sarlio-Lähteenkorva S, Lahelma E . Psychosocial working conditions and weight gain among employees. Int J obesity 2005; 29: 909–915.
Kouvonen A, Kivimäki M, Cox SJ, Cox T, Vahtera J . Relationship between work stress and body mass index among 45,810 female and male employees. Psychosom Med 2005; 67: 577–583.
Logue J, Murray HM, Welsh P, Shepherd J, Packard C, Macfarlane P et al. Obesity is associated with fatal coronary heart disease independently of traditional risk factors and deprivation. Heart 2011; 97: 564–568.
Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Eng J Med 2011; 365: 1876–1885.
Karason K, Mølgaard H, Wikstrand J, Sjöström L . Heart rate variability in obesity and the effect of weight loss. Am J Cardiol 1999; 83: 1242–1247.
Steptoe A, Kivimäki M . Stress and cardiovascular disease. Nat Rev Cardiol 2012; 9: 360–370.
Windham BG, Fumagalli S, Ble A, Sollers JJ, Thayer JF, Najjar SS et al. The relationship between heart rate variability and adiposity differs for central and overall adiposity. Journal of obesity 2012; 2012: 149516.
Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M et al. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J 2008; 29: 640–648.
(NIH) NIoH, National Heart L, and Blood Institute (NHLBI), (NAASO) NAAftSoO. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Rockville, MD: National Institutes of Health, 2000.
Fleishman EA . Toward a Taxonomy of Human Performance. Am Psychol 1975; 30: 1127–1149.
Peterson L, Peterson MJ . Short-term retention of individual verbal items. J Exp Psychol 1959; 58: 193–198.
Schleifer LM, Spalding TW, Kerick SE, Cram JR, Ley R, Hatfield BD . Mental stress and trapezius muscle activation under psychomotor challenge: A focus on EMG gaps during computer work. Psychophysiology 2008; 45: 356–365.
Allen M, Crowell M . Patterns of autonomic response during laboratory stressors. Psychophysiology 1989; 26: 603–614.
Vøllestad NK . Measurement of human muscle fatigue. J Neurosci Methods 1997; 74: 219–227.
Borg G . Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health 1990; 16: 55.
Hart SG, Staveland LE . Development of NASA-TLX (Task Load Index): Results of empirical and theoretical research. Adv Psychology 1988; 52: 139–183.
Taylor JL, Gandevia SC . A comparison of central aspects of fatigue in submaximal and maximal voluntary contractions. J Appl Physiol 2008; 104: 542–550.
Malik M, Bigger J, Camm A, Kleiger R, Malliani A, Moss A et al. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 1996; 93: 1043.
Hulens M, Vansant G, Lysens R, Claessens AL, Muls E . Assessment of isokinetic muscle strength in women who are obese. J Orthop Sport Phys Ther 2002; 32: 347.
Lafortuna C, Agosti F, Marinone P, Marazzi N, Sartorio A . The relationship between body composition and muscle power output in men and women with obesity. J Endocrinol Invest 2004; 27: 854.
Eksioglu M . Endurance time of grip-force as a function of grip-span, posture and anthropometric variables. Int J Ind Ergon 2011; 41: 401–409.
Cavuoto L, Nussbaum M . Obesity-related differences in muscular capacity during sustained isometric exertions. Appl Ergon 2013; 44: 254–260.
Hjortskov N, Rissen D, Blangsted AK, Fallentin N, Lundberg U, Søgaard K . The effect of mental stress on heart rate variability and blood pressure during computer work. Eur J Appl Physiol 2004; 92: 84–89.
Lundberg Forsman M, Zachau G, Ekloèf M, Palmerud G, Melin B et al. Effects of experimentally induced mental and physical stress on motor unit recruitment in the trapezius muscle. Work Stress 2002; 16: 166–178.
Marras WS, Davis KG, Heaney CA, Maronitis AB, Allread WG . The Influence of psychosocial stress, gender, and personality on mechanical loading of the lumbar spine. Spine 2000; 25: 3045–3054.
Mehta RK, Parasuraman R . The effect of mental fatigue on the development of physical fatigue: a neuroergonomic approach. Human Factors 2014; 56: 645–656.
Mandrick K, Derosiere G, Dray G, Coulon D, Micallef J-P, Perrey S . Prefrontal cortex activity during motor tasks with additional mental load requiring attentional demand: a near-infrared spectroscopy study. Neurosci Res 2013; 76: 156–162.
Thayer JF, Yamamoto SS, Brosschot JF . The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol 2010; 141: 122–131.
Martini G, Riva P, Rabbia F, Molini V, Ferrero GB, Cerutti F et al. Heart rate variability in childhood obesity. Clin Auton Res 2001; 11: 87–91.
Villareal DT, Banks M, Siener C, Sinacore DR, Klein S . Physical frailty and body composition in obese elderly men and women. Obesity Res 2004; 12: 913–920.
Acknowledgements
Funding for this project was provided by Grant No. 5T42OH008421 from the National Institute for Occupational and Environmental Health (NIOSH)/Centers for Disease Control and Prevention to the Southwest Center for Occupational and Environmental Health (SWCOEH), a NIOSH Education and Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Mehta, R. Impacts of obesity and stress on neuromuscular fatigue development and associated heart rate variability. Int J Obes 39, 208–213 (2015). https://doi.org/10.1038/ijo.2014.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.127
This article is cited by
-
Heart failure-type symptom scores in chronic kidney disease: The importance of body mass index
International Journal of Obesity (2022)
-
Obesity and Poststroke Fatigue: A 2-Year Longitudinal Study
Neurology and Therapy (2021)
-
Fusion of heart rate variability and salivary cortisol for stress response identification based on adverse childhood experience
Medical & Biological Engineering & Computing (2019)
-
Anthropometric variables as predictors of aspects of quality of life in persons with central obesity
BMC Research Notes (2018)
-
Task-relevant cognitive and motor functions are prioritized during prolonged speed–accuracy motor task performance
Experimental Brain Research (2018)