Abstract
Background:
Dairy foods are nutrient dense and may be protective against long-term weight gain.
Objective:
We aimed to examine the longitudinal association between dairy consumption and annualized changes in weight and waist circumference (WC) in adults.
Methods:
Members of the Framingham Heart Study Offspring Cohort who participated in the fifth through eighth study examinations (1991–2008) were included in these analyses (3440 participants with 11 683 observations). At each exam, dietary intake was assessed by a validated food frequency questionnaire, and weight and WC were assessed following standardized procedures. Repeated measures models were used for the longitudinal analyses of annualized weight and waist circumference changes, adjusting for time-varying or invariant covariates.
Results:
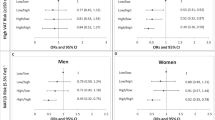
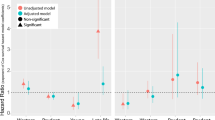
On average, participants gained weight and WC during follow-up. Dairy intake increased across exams. After adjusting for demographic and lifestyle factors (including diet quality), participants who consumed ⩾3 servings per day of total dairy had 0.10 kg (±0.04) smaller annualized increment of weight (Ptrend=0.04) than those consuming <1 serving per day. Higher total dairy intake was also marginally associated with less WC gain (Ptrend=0.05). Similarly, participants who consumed ⩾3 servings per week of yogurt had a 0.10 kg (±0.04) and 0.13 cm (±0.05) smaller annualized increment of weight (Ptrend=0.03) and WC (Ptrend=0.008) than those consuming <1 serving per week, respectively. Skim/low-fat milk, cheese, total high-fat or total low-fat dairy intake were not associated with long-term change in weight or WC.
Conclusion:
Further longitudinal and interventional studies are warranted to confirm the beneficial role of increasing total dairy and yogurt intake, as part of a healthy and calorie-balanced dietary pattern, in the long-term prevention of gain in weight and WC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
World Health Organization. Controlling the Global Obesity Epidemic. www.who.int/nutrition/topics/obesity/en/. Accessed 2012.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL . Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998; 22: 39–47.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of obesity in the United States, 2009–2010. NCHS data brief, no 82. NCHS data brief, no 82 2012. National Center for Health Statistics: Hyattsville, MD, 2012.
Mathieu P, Lemieux I, Despres JP . Obesity, inflammation, and cardiovascular risk. Clin Pharmacol Ther 2010; 87: 407–416.
Despres JP, Arsenault BJ, Cote M, Cartier A, Lemieux I . Abdominal obesity: the cholesterol of the 21st century? Can J Cardiol 2008; 24 (Suppl D): 7D–12D.
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W . Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009; 28: w822–w831.
United States Department of Agriculture. Dietary Guidelines for Americans, 2010 (Policy Document). Released 1/31/11; 2012.
Louie JC, Flood VM, Hector DJ, Rangan AM, Gill TP . Dairy consumption and overweight and obesity: a systematic review of prospective cohort studies. Obes Rev 2011; 12: e582–e592.
Dougkas A, Reynolds CK, Givens ID, Elwood PC, Minihane AM . Associations between dairy consumption and body weight: a review of the evidence and underlying mechanisms. Nutr Res Rev 2011; 24: 72–95.
Chen M, Pan A, Malik VS, Hu FB . Effects of dairy intake on body weight and fat: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2012; 96: 735–747.
Abargouei AS, Janghorbani M, Salehi-Marzijarani M, Esmaillzadeh A . Effect of dairy consumption on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Obes (Lond) 2012; 36: 1485–1493.
Wu T, Gao X, Chen M, van Dam RM . Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev 2009; 10: 313–323.
Curioni CC, Lourenco PM . Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond) 2005; 29: 1168–1174.
Rosell M, Hakansson NN, Wolk A . Association between dairy food consumption and weight change over 9 y in 19,352 perimenopausal women. Am J Clin Nutr 2006; 84: 1481–1488.
Meydani SN, Ha WK . Immunologic effects of yogurt. Am J Clin Nutr 2000; 71: 861–872.
Adolfsson O, Meydani SN, Russell RM . Yogurt and gut function. Am J Clin Nutr 2004; 80: 245–256.
Wang H, Livingston KA, Fox CS, Meigs JB, Jacques PF . Yogurt consumption is associated with better diet quality and metabolic profile in American men and women. . Nutr Res 2013; 33: 18–26.
Usinger L, Ibsen H, Jensen LT . Does fermented milk possess antihypertensive effect in humans? J Hypertens 2009; 27: 1115–1120.
Framingham Heart Study. www.framinghamheartstudy.org. Accessed 2012.
Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC . Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 1992; 135: 1114–1126 discussion 1127-36.
Willett WC, Reynolds RD, Cottrell-Hoehner S, Sampson L, Browne ML . Validation of a semi-quantitative food frequency questionnaire: comparison with a 1-year diet record. J Am Diet Assoc 1987; 87: 43–47.
Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989; 18: 858–867.
Willett WC . Food frequency methods. Nutritional Epidemiology.. Oxford University Press: New York pp 74–91 1998.
US Department of Agriculture. National Nutrient Database for Standard Reference, Release 25. www.ars.usda.gov/SP2UserFiles/Place/12354500/Data/SR25/sr25_doc.pdf. Accessed 2012.
Fogli-Cawley JJ, Dwyer JT, Saltzman E, McCullough ML, Troy LM, Jacques PF . The 2005 Dietary Guidelines for Americans Adherence Index: development and application. J Nutr 2006; 136: 2908–2915.
Kannel WB, Sorlie P . Some health benefits of physical activity. The Framingham Study. Arch Intern Med 1979; 139: 857–861.
World Health Organization. WHO Expert Committee on Diabetes Mellitus: Second Report. 1980.
McNamara JR, Schaefer EJ . Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin Chim Acta 1987; 166: 1–8.
Warnick GR, Benderson J, Albers JJ . Dextran sulfate-Mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem 1982; 28: 1379–1388.
Preis SR, Massaro JM, Robins SJ, Hoffmann U, Vasan RS, Irlbeck T et al. Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obesity (Silver Spring) 2010; 18: 2191–2198.
Chau D, Cho LM, Jani P St, Jeor ST . Individualizing recommendations for weight management in the elderly. Curr Opin Clin Nutr Metab Care 2008; 11: 27–31.
Han TS, Tajar A, Lean ME . Obesity and weight management in the elderly. Br Med Bull 2011; 97: 169–196.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763–778.
Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med 1998; 128: 81–88.
Panico S, Palmieri L, Donfrancesco C, Vanuzzo D, Chiodini P, Cesana G et al. Preventive potential of body mass reduction to lower cardiovascular risk: the Italian Progetto CUORE study. Prev Med 2008; 47: 53–60.
Lanou AJ, Barnard ND . Dairy and weight loss hypothesis: an evaluation of the clinical trials. Nutr Rev 2008; 66: 272–279.
Pereira MA, Jacobs DR Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS . Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA 2002; 287: 2081–2089.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB . Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011; 364: 2392–2404.
Vergnaud AC, Peneau S, Chat-Yung S, Kesse E, Czernichow S, Galan P et al. Dairy consumption and 6-y changes in body weight and waist circumference in middle-aged French adults. Am J Clin Nutr 2008; 88: 1248–1255.
Drapeau V, Despres JP, Bouchard C, Allard L, Fournier G, Leblanc C et al. Modifications in food-group consumption are related to long-term body-weight changes. Am J Clin Nutr 2004; 80: 29–37.
Zemel MB . The role of dairy foods in weight management. J Am Coll Nutr 2005; 24: 537S–546SS.
Zemel MB, Thompson W, Milstead A, Morris K, Campbell P . Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res 2004; 12: 582–590.
Zemel MB, Richards J, Milstead A, Campbell P . Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes Res 2005; 13: 1218–1225.
Pfeuffer M, Schrezenmeir J . Milk and the metabolic syndrome. Obes Rev 2007; 8: 109–118.
Diamant M, Blaak EE, de Vos WM . Do nutrient-gut-microbiota interactions play a role in human obesity, insulin resistance and type 2 diabetes? Obes Rev 2011; 12: 272–281.
Arora T, Sharma R . Fermentation potential of the gut microbiome: implications for energy homeostasis and weight management. Nutr Rev 2011; 69: 99–106.
Rajpathak SN, Rimm EB, Rosner B, Willett WC, Hu FB . Calcium and dairy intakes in relation to long-term weight gain in US men. Am J Clin Nutr 2006; 83: 559–566.
Sanchez-Villegas A, Bes-Rastrollo M, Martinez-Gonzalez MA, Serra-Majem L . Adherence to a Mediterranean dietary pattern and weight gain in a follow-up study: the SUN cohort. Int J Obes (Lond) 2006; 30: 350–358.
Terpstra AH . Effect of conjugated linoleic acid on body composition and plasma lipids in humans: an overview of the literature. Am J Clin Nutr 2004; 79: 352–361.
Larsen TM, Toubro S, Astrup A . Efficacy and safety of dietary supplements containing CLA for the treatment of obesity: evidence from animal and human studies. J Lipid Res 2003; 44: 2234–2241.
Smedman AE, Gustafsson IB, Berglund LG, Vessby BO . Pentadecanoic acid in serum as a marker for intake of milk fat: relations between intake of milk fat and metabolic risk factors. Am J Clin Nutr 1999; 69: 22–29.
Wang H, Steffen LM, Vessby B, Basu S, Steinberger J, Moran A et al. Obesity modifies the relations between serum markers of dairy fats and inflammation and oxidative stress among adolescents. Obesity (Silver Spring) 2011; 19: 2404–2410.
Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ, Wang Y . Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr 2008; 87: 1914–1925.
Hjartaker A, Lagiou A, Slimani N, Lund E, Chirlaque MD, Vasilopoulou E et al. Consumption of dairy products in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort: data from 35 955 24-hour dietary recalls in 10 European countries. Public Health Nutr 2002; 5: 1259–1271.
Acknowledgements
We thank Kara A Livingston, Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University, for the help with data set management. This work was supported by the National Heart, Lung and Blood Institute of the National Institute of Health (contract number: NO1-HC-25195), US Department of Agriculture Agreement 58–1950–7-707 and research grants from The Dannon Company, Inc., and General Mills Bell Institute of Health and Nutrition.
Author contributions
PFJ and NMM designed the research; PFJ and HW conducted the research; JBM, CSF and GTR provided essential materials; HW and GTR analyzed data or performed statistical analysis; HW and PFJ wrote the paper; PFJ had primary responsibility for final content; and LMT, NMM and CSF did critical review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
PF Jacques and H Wang received support from a grant from The Dannon Company Inc., PF Jacques is a member of the Dannon Yogurt Advisory Board, NM McKeown and LM Troy were funded in part by a grant from General Mills Bell Institute of Health and Nutrition. G Rogers, C Fox and J Meigs declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, H., Troy, L., Rogers, G. et al. Longitudinal association between dairy consumption and changes of body weight and waist circumference: the Framingham Heart Study. Int J Obes 38, 299–305 (2014). https://doi.org/10.1038/ijo.2013.78
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.78
Keywords
This article is cited by
-
Higher abdominal adiposity is associated with higher lean muscle mass but lower muscle quality in middle-aged and older men and women: the Framingham Heart Study
Aging Clinical and Experimental Research (2023)
-
Snacking pattern of college students in Saudi Arabia: a cross-sectional study
BMC Nutrition (2022)
-
Gut microbiota and fermentation-derived branched chain hydroxy acids mediate health benefits of yogurt consumption in obese mice
Nature Communications (2022)
-
Dietary and policy priorities to reduce the global crises of obesity and diabetes
Nature Food (2020)
-
The relationship between yogurt consumption, body weight, and metabolic profiles in youth with a familial predisposition to obesity
European Journal of Clinical Nutrition (2019)