Abstract
Background:
Temporal pathways of known associations between overweight and poor health-related quality of life (HRQoL) in adolescents remain poorly documented. This study aims to (1) examine timing and strength of the association between HRQoL and body mass index (BMI) in childhood, and (2) investigate directionality and impact of cumulative burden in any observed HRQoL–BMI associations.
Design, setting and participants:
Participants were 3898 children in the population-based Longitudinal Study of Australian Children (LSAC) assessed at four biennial waves from ages 4–5 (2004) to 10–11 years (2010).
Main measures:
At every wave, parents completed the Pediatric Quality of Life Inventory, and measured BMI (kg m−2) was converted into BMIz and overweight using international norms.
Analyses:
Linear and logistic regressions.
Results:
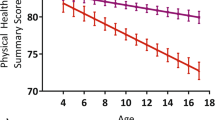
Overweight first became cross-sectionally associated with HRQoL at 6–7 years of age, with linear associations between poorer HRQoL (physical and psychosocial health) and higher BMI developing by 8–9 years and strengthening by 10–11 years. Longitudinal analyses revealed cumulative relationships such that the number of times a child was overweight between the ages 4 and 11 years predicted progressively poorer scores on both physical and psychosocial health at 10–11 years (P-values for trend <0.001). In the weaker reverse associations, children with poor (vs persistently good) physical health at any wave had slightly higher mean BMIz at age 10–11 years, but this difference was small (0.14, 95% confidence interval (CI): 0.04, 0.24) and not cumulative; results for psychosocial health were even weaker, with mixed subscale findings.
Conclusions:
Middle childhood appears to be the critical period in which HRQoL–BMI comorbidities emerge and strengthen, first among children with clinically relevant conditions, that is, overweight or poor HRQoL, and then more generally across the whole range of BMI. Poorer HRQoL seemed predominantly a consequence of higher BMI, rather than a cause, suggesting that effective promotion of healthy weight could benefit multiple aspects of children’s well-being.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Obesity and Overweight, Fact Sheet No. 311. WHO: Geneva, Switzerland, 2011.
Jackson-Leach R, Lobstein T . Estimated burden of paediatric obesity and co-morbidities in Europe. Part 1. The increase in the prevalence of child obesity in Europe is itself increasing. Int J Pediatr Obes 2006; 1: 26–32.
Olds TS, Tomkinson GR, Ferrar KE, Maher CA . Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int J Obes 2010; 34: 57–66.
Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L et al. Health consequences of obesity. Arch Dis Child 2003; 88: 748–752.
Kolotkin RL, Meter K, Williams GR . Quality of life and obesity. Obes Rev 2001; 2: 219–229.
Cameron AJ, Magliano DJ, Dunstan DW, Zimmet PZ, Hesketh K, Peeters A et al. A bi-directional relationship between obesity and health-related quality of life: evidence from the longitudinal AusDiab study. Int J Obes (Lond) 2012; 36: 295–303.
Sach TH, Barton GR, Doherty M, Muir KR, Jenkinson C, Avery AJ . The relationship between body mass index and health-related quality of life: comparing the EQ-5D, EuroQol VAS and SF-6D. Int J Obes (Lond) 2007; 31: 189–196.
Doll HA, Petersen SE, Stewart-Brown SL . Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res 2000; 8: 160–170.
Jia H, Lubetkin EI . The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health 2005; 27: 156–164.
Tsiros MD, Olds T, Buckley JD, Grimshaw P, Brennan L, Walkley J et al. Health-related quality of life in obese children and adolescents. Int J Obes (Lond) 2009; 33: 387–400.
Wood-Dauphinee S . Assessing quality of life in clinical research: from where have we come and where are we going? J Clin Epidemiol 1999; 52: 355–363.
Idler EL, Benyamini Y . Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997; 38: 21–37.
Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F et al. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 2003; 64: 339–349.
Konstam V, Salem D, Pouleur H, Kostis J, Gorkin L, Shumaker S et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. Am J Cardiol 1996; 78: 890–895.
Wake M, Clifford SA, Patton GC, Waters E, Williams J, Canterford L et al. Morbidity patterns among the underweight, overweight and obese between 2 and 18 years: population-based cross-sectional analyses. Int J Obes (Lond) 2013; 37: 86–93.
Williams JW, Canterford L, Hesketh KD, Hardy P, Waters EB, Patton GC et al. Changes in body mass index and health related quality of life from childhood to adolescence. Int J Pediatr Obes 2010; 6: e442–e448.
Kruger J, Bowles HR, Jones DA, Ainsworth BE, Kohl HW 3rd . Health-related quality of life, BMI and physical activity among US adults (>/=18 years): National Physical Activity and Weight Loss Survey, 2002. Int J Obes (Lond) 2007; 31: 321–327.
Markowitz S, Friedman MA, Arent SM . Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clin Psychol Sci Prac 2008; 15: 1–20.
Griffiths LJ, Parsons TJ, Hill AJ . Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes 2010; 5: 282–304.
Wille N, Erhart M, Petersen C, Ravens-Sieberer U . The impact of overweight and obesity on health-related quality of life in childhood—results from an intervention study. BMC Public Health 2008; 8: 421.
Sawyer MG, Harchak T, Wake M, Lynch J . Four-year prospective study of BMI and mental health problems in young children. Pediatrics 2011; 128: 677–684.
Varni JW, Limbers CA, Burwinkle TM . Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007; 5: 2.
Hesketh K, Wake M, Waters E, Carlin J, Crawford D . Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public Health Nutr 2004; 7: 303–309.
Hopman WM, Berger C, Joseph L, Towheed T, VandenKerkhof E, Anastassiades T et al. The natural progression of health-related quality of life: results of a five-year prospective study of SF-36 scores in a normative population. Qual Life Res 2006; 15: 527–536.
Casey VA, Dwyer JT, Coleman KA, Valadian I . Body mass index from childhood to middle age: a 50-y follow-up. Am J Clin Nutr 1992; 56: 14–18.
Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ . Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008; 9: 474–488.
Wake M, Hardy P, Sawyer MG, Carlin JB . Comorbidities of overweight/obesity in Australian preschoolers: a cross-sectional population study. Arch Dis Child 2008; 93: 502–507.
Australian Government Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA). Growing Up in Australia: the Longitudinal Study of Australian Children: 2010–11 Annual Report, 2012.. Australian Government Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA): Canberra, Australia, 2012.
Varni JW, Burwinkle TM, Seid M, Skarr D . The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003; 3: 329–341.
Varni JW, Limbers CA, Burwinkle TM . Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007; 5: 43.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 2002; 11: 1–190.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Wake M, Hardy P, Canterford L, Sawyer M, Carlin JB . Overweight, obesity and girth of Australian preschoolers: prevalence and socio-economic correlates. Int J Obes (Lond) 2007; 31: 1044–1051.
Blackmore T, Strazdins L, Gibbings J . Measuring family socioeconomic position. Austr Soc Policy J 2009; 8: 121–168.
Daraganova G, Sipthorp M . Wave 4 Weights (LSAC Technical Paper No. 9). Australian Institute of Family Studies: Melbourne, Australia, 2011.
Spratt M, Carpenter J, Sterne JA, Carlin JB, Heron J, Henderson J et al. Strategies for multiple imputation in longitudinal studies. Am J Epidemiol 2010; 172: 478–487.
Little R, Rubin D . Statistical Analysis With Missing Data. Wiley: New York, NY, USA, 1987.
Jansen P, Mensah F, Clifford S, Tiemeier H, Nicholson J, Wake M . Development of mental health problems and overweight between ages 4 and 11 years: a population-based Longitudinal Study of Australian Children. Acad Pediatrics 2013; 13: 159–167.
Heo M, Allison DB, Faith MS, Zhu S, Fontaine KR . Obesity and quality of life: mediating effects of pain and comorbidities. Obes Res 2003; 11: 209–216.
Incledon E, Gerner B, Hay M, Brennan L, Wake M . Psychosocial predictors of 4-year BMI change in overweight and obese children in primary care. Obes 2013; 21: E262–E270.
Bornstein SR, Schuppenies A, Wong ML, Licinio J . Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry 2006; 11: 892–902.
Rapa A, Monzani A, Moia S, Vivenza D, Bellone S, Petri A et al. Subclinical hypothyroidism in children and adolescents: a wide range of clinical, biochemical, and genetic factors involved. J Clin Endocrinol Metab 2009; 94: 2414–2420.
Freedman DS, Sherry B . The validity of BMI as an indicator of body fatness and risk among children. Pediatrics 2009; 124 (Suppl 1): S23–S34.
Jackson R, Marshall R, Kerr A, Riddell T, Wells S . QRISK or Framingham for predicting cardiovascular risk? BMJ 2009; 339: b2673.
Wells S, Kerr A, Eadie S, Wiltshire C, Jackson R . ‘Your Heart Forecast’: a new approach for describing and communicating cardiovascular risk? Heart 2010; 96: 708–713.
Acknowledgements
The Longitudinal Study of Australian Children is conducted in partnership between the Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA), the Australian Institute of Family Studies (AIFS) and the Australian Bureau of Statistics (ABS). The findings and views reported are those of the authors and should not be attributed to FaHCSIA, AIFS or the ABS. We thank all the parents and children for their continuing support and participation in the LSAC. PWJ was supported by the Netherlands Organization for Scientific Research (NWO) and the Marie Cofund Action (Rubicon grant 446-11-010), and by the Ter Meulen Fund of the Royal Netherlands Academy of Arts and Sciences (KNAW). MW was supported by NHMRC Population Health Career Development Award 546405, and FKM by NHMRC Public Health Capacity Building Grant 436914 and NHMRC Early Career Fellowship 1037449. All research at the Murdoch Childrens Research Institute is supported by the Victorian Government’s Operational Infrastructure Program. This work also received support from the ‘Parenting Australia’s Children’ research group at the Parenting Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jansen, P., Mensah, F., Clifford, S. et al. Bidirectional associations between overweight and health-related quality of life from 4–11 years: Longitudinal Study of Australian Children. Int J Obes 37, 1307–1313 (2013). https://doi.org/10.1038/ijo.2013.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.71
Keywords
This article is cited by
-
Child and adolescent obesity
Nature Reviews Disease Primers (2023)
-
Psychometric Evaluation of the PedsQL GCS and CHU9D in Australian Children and Adolescents with Common Chronic Health Conditions
Applied Health Economics and Health Policy (2023)
-
Somatic complaints as a mediator in the association between body mass index and quality of life in children and adolescents
BMC Family Practice (2021)
-
Weight status and health-related quality of life during childhood and adolescence: effects of age and socioeconomic position
International Journal of Obesity (2020)
-
Estimating Age- and Sex-Specific Utility Values from the CHU9D Associated with Child and Adolescent BMI z-Score
PharmacoEconomics (2020)