Abstract
Backround/Objectives:
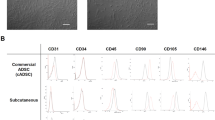
Adipose tissue (AT) is a dynamic organ that expands and contracts rapidly. It is composed of adipocytes and of cell populations among which immune cells and mesenchymal progenitors known as adipose stromal cells (ASCs). The AT cell turnover has been extensively studied. Surprisingly it has only been viewed as the result of both cell proliferation/death and cell infiltration. Nevertheless, both immune cells and ASCs exhibit migration abilities; therefore their egress from AT in response to physiological/pathophysiological stimuli has to be considered. To do so, the aim of the present work was to develop a model allowing the study of cell release from the adipose organ.
Subjects/Methods:
Mesenteric (Mes) ATs were isolated from 9-week-old C57BL/6 male mice and were catheterized via the superior mesenteric artery and were perfused with a saline solution. After an equilibration period, the mesenteric fat pad was perfused with CXCL12 (stromal-derived factor-1, SDF-1) or sphingosine 1-phosphate (S1P) to trigger cell mobilization and perfusates were collected every 30 min for subsequent flow cytometry analyses.
Results:
We report here that CXCL12 induces the specific release of ASCs from MesAT thus demonstrating that ASCs are specifically mobilized from fat depots by a CXCL12-dependent pathway. Moreover, we showed that leukocyte mobilization can be triggered via a S1P-dependent pathway.
Conclusions:
We have developed a microperfusion model of an intact fat depot allowing the study of AT cell release in response to various molecules. The perfusion system described here demonstrates that ASCs and leukocytes can be pharmacologically mobilized from AT. Therefore, AT microperfusion might constitute an appropriate and reliable approach for evaluating the mobilization of different cell populations from AT in various physiological and pathophysiological contexts. Such a model might help in identifying factors and drugs controlling AT cell release, impacting the medical fields of regenerative medicine and of obesity or its associated comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Caspar-Bauguil S, Cousin B, Galinier A, Segafredo C, Nibbelink M, Andre M et al. Adipose tissues as an ancestral immune organ: site-specific change in obesity. FEBS Lett 2005; 579: 3487–3492.
Bourlier V, Zakaroff-Girard A, Miranville A, De Barros S, Maumus M, Sengenes C et al. Remodeling phenotype of human subcutaneous adipose tissue macrophages. Circulation 2008; 117: 806–815.
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 2002; 13: 4279–4295.
Gimble JM, Katz AJ, Bunnell BA . Adipose-derived stem cells for regenerative medicine. Circ Res 2007; 100: 1249–1260.
Bjorntorp P, Sjostrom L . Adipose tissue cellularity. Int J Obes 1979; 3: 181–187.
Hausman DB, DiGirolamo M, Bartness TJ, Hausman GJ, Martin RJ . The biology of white adipocyte proliferation. Obes Rev 2001; 2: 239–254.
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O et al. Dynamics of fat cell turnover in humans. Nature 2008; 453: 783–787.
Maumus M, Sengenes C, Decaunes P, Zakaroff-Girard A, Bourlier V, Lafontan M et al. Evidence of in situ proliferation of adult adipose tissue-derived progenitor cells: influence of fat mass microenvironment and growth. J Clin Endocrinol Metab 2008; 93: 4098–4106.
Rigamonti A, Brennand K, Lau F, Cowan CA . Rapid cellular turnover in adipose tissue. PLoS One 2011; 6: e17637.
Onate B, Vilahur G, Ferrer-Lorente R, Ybarra J, Diez-Caballero A, Ballesta-Lopez C et al. The subcutaneous adipose tissue reservoir of functionally active stem cells is reduced in obese patients. Faseb J 2012; 26: 4327–4336.
Fujiwara K, Hasegawa K, Ohkumo T, Miyoshi H, Tseng YH, Yoshikawa K . Necdin controls proliferation of white adipocyte progenitor cells. PLoS One 2012; 7: e30948.
Miller MJ, Wei SH, Parker I, Cahalan MD . Two-photon imaging of lymphocyte motility and antigen response in intact lymph node. Science 2002; 296: 1869–1873.
Girard JP, Moussion C, Forster R . HEVs lymphatics and homeostatic immune cell trafficking in lymph nodes. Nat Rev Immunol 2012; 12: 762–773.
Khakoo AY, Pati S, Anderson SA, Reid W, Elshal MF, Rovira II et al. Human mesenchymal stem cells exert potent antitumorigenic effects in a model of Kaposi's sarcoma. J Exp Med 2006; 203: 1235–1247.
Kucerova L, Altanerova V, Matuskova M, Tyciakova S, Altaner C . Adipose tissue-derived human mesenchymal stem cells mediated prodrug cancer gene therapy. Cancer Res 2007; 67: 6304–6313.
Zhang Y, Daquinag A, Traktuev DO, Amaya-Manzanares F, Simmons PJ, March KL et al. White adipose tissue cells are recruited by experimental tumors and promote cancer progression in mouse models. Cancer Res 2009; 69: 5259–5266.
Gil-Ortega M, Garidou L, Barreau C, Maumus M, Breasson L, Tavernier G et al. Native adipose stromal cells egress from adipose tissue in vivo: evidence during lymph node activation. Stem Cells 2013; 31: 1309–1320.
Galvez B, de Castro J, Herold D, Dubrovska G, Arribas S, Gonzalez MC et al. Perivascular adipose tissue and mesenteric vascular function in spontaneously hypertensive rats. Arterioscler Thromb Vasc Biol 2006; 26: 1297–1302.
Gil-Ortega M, Stucchi P, Guzman-Ruiz R, Cano V, Arribas S, Gonzalez MC et al. Adaptative nitric oxide overproduction in perivascular adipose tissue during early diet-induced obesity. Endocrinology 2010; 151: 3299–3306.
Cinamon G, Matloubian M, Lesneski MJ, Xu Y, Low C, Lu T et al. Sphingosine 1-phosphate receptor 1 promotes B cell localization in the splenic marginal zone. Nature Immunol 2004; 5: 713–720.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr . Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003; 112: 1796–1808.
Nishimura S, Manabe I, Nagasaki M, Eto K, Yamashita H, Ohsugi M et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat Med 2009; 15: 914–920.
Crossno JT Jr, Majka SM, Grazia T, Gill RG, Klemm DJ . Rosiglitazone promotes development of a novel adipocyte population from bone marrow-derived circulating progenitor cells. J Clin Invest 2006; 116: 3220–3228.
Puissant B, Barreau C, Bourin P, Clavel C, Corre J, Bousquet C et al. Immunomodulatory effect of human adipose tissue-derived adult stem cells: comparison with bone marrow mesenchymal stem cells. Br J Haematol 2005; 129: 118–129.
Yanez R, Lamana ML, Garcia-Castro J, Colmenero I, Ramirez M, Bueren JA . Adipose tissue-derived mesenchymal stem cells have in vivo immunosuppressive properties applicable for the control of the graft-versus-host disease. Stem Cells 2006; 24: 2582–2591.
Salem HK, Thiemermann C . Mesenchymal stromal cells: current understanding and clinical status. Stem Cells 2010; 28: 585–596.
Lazennec G, Jorgensen C . Concise review: adult multipotent stromal cells and cancer: risk or benefit? Stem Cells 2008; 26: 1387–1394.
Fernandez M, Simon V, Herrera G, Cao C, Del Favero H, Minguell JJ . Detection of stromal cells in peripheral blood progenitor cell collections from breast cancer patients. Bone Marrow Transplant 1997; 20: 265–271.
Wang Y, Johnsen HE, Mortensen S, Bindslev L, Ripa RS, Haack-Sorensen M et al. Changes in circulating mesenchymal stem cells, stem cell homing factor, and vascular growth factors in patients with acute ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Heart 2006; 92: 768–774.
Mansilla E, Marin GH, Drago H, Sturla F, Salas E, Gardiner C et al. Bloodstream cells phenotypically identical to human mesenchymal bone marrow stem cells circulate in large amounts under the influence of acute large skin damage: new evidence for their use in regenerative medicine. Transplant Proc 2006; 38: 967–969.
Zhang Y, Bellows CF, Kolonin MG . Adipose tissue-derived progenitor cells and cancer. World J Stem Cells 2010; 2: 103–113.
Zhang Y, Daquinag AC, Amaya-Manzanares F, Sirin O, Tseng C, Kolonin MG . Stromal progenitor cells from endogenous adipose tissue contribute to pericytes and adipocytes that populate the tumor microenvironment. Cancer Res 2012; 72: 5198–5208.
Goeden N, Bonnin A . Ex vivo perfusion of mid-to-late-gestation mouse placenta for maternal-fetal interaction studies during pregnancy. Nature Protoc 2013; 8: 66–74.
Magnon C, Lucas D, Frenette PS . Trafficking of stem cells. Methods Mol Biol 2011; 750: 3–24.
Mazo IB, Massberg S, von Andrian UH . Hematopoietic stem and progenitor cell trafficking. Trends Immunol 2011; 32: 493–503.
Nagasawa T, Hirota S, Tachibana K, Takakura N, Nishikawa S, Kitamura Y et al. Defects of B-cell lymphopoiesis and bone-marrow myelopoiesis in mice lacking the CXC chemokine PBSF/SDF-1. Nature 1996; 382: 635–638.
Zou YR, Kottmann AH, Kuroda M, Taniuchi I, Littman DR . Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature 1998; 393: 595–599.
Lapidot T, Kollet O . The essential roles of the chemokine SDF-1 and its receptor CXCR4 in human stem cell homing and repopulation of transplanted immune-deficient NOD/SCID and NOD/SCID/B2m(null) mice. Leukemia 2002; 16: 1992–2003.
Wynn RF, Hart CA, Corradi-Perini C, O'Neill L, Evans CA, Wraith JE et al. A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood 2004; 104: 2643–2645.
Maijenburg MW, van der Schoot CE, Voermans C . Mesenchymal stromal cell migration: possibilities to improve cellular therapy. Stem Cells Dev 2012; 21: 19–29.
Sengenes C, Miranville A, Maumus M, de Barros S, Busse R, Bouloumie A . Chemotaxis and differentiation of human adipose tissue CD34+/CD31- progenitor cells: role of stromal derived factor-1 released by adipose tissue capillary endothelial cells. Stem Cells 2007; 25: 2269–2276.
Martin C, Burdon PC, Bridger G, Gutierrez-Ramos JC, Williams TJ, Rankin SM . Chemokines acting via CXCR2 and CXCR4 control the release of neutrophils from the bone marrow and their return following senescence. Immunity 2003; 19: 583–593.
Levesque JP, Hendy J, Takamatsu Y, Simmons PJ, Bendall LJ . Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induced by GCSF or cyclophosphamide. J Clin Invest 2003; 111: 187–196.
Miranville A, Heeschen C, Sengenes C, Curat CA, Busse R, Bouloumie A . Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation 2004; 110: 349–355.
Acknowledgements
This work was supported by Inserm, ‘La ligue nationale contre le cancer’, the Association Française d’étude et de recherches sur l’obésité (Afero) and Roche (2007). We would like to thank Christophe Guissard for his invaluable technical assistance. We are grateful to the ‘Institut des Technologies Avancées en sciences du Vivant’ (ITAV) UMS 3039 and Dr J Rouquette for adipose tissue imaging.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Gil-Ortega, M., Fernández-Alfonso, M., Somoza, B. et al. Ex vivo microperfusion system of the adipose organ: a new approach to studying the mobilization of adipose cell populations. Int J Obes 38, 1255–1262 (2014). https://doi.org/10.1038/ijo.2013.243
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.243
Keywords
This article is cited by
-
Adipose tissue is a source of regenerative cells that augment the repair of skeletal muscle after injury
Nature Communications (2023)
-
Putative circulating adipose tissue-derived stem cells, obesity, and metabolic syndrome features
Journal of Endocrinological Investigation (2023)
-
Role of VEGFs in metabolic disorders
Angiogenesis (2020)