Abstract
Background:
Because of the high prevalence of overweight and obesity, there is a need to identify cost-effective approaches for weight loss in primary care and community settings.
Objective:
To evaluate the long-term cost effectiveness of a commercial weight loss programme (Weight Watchers) (CP) compared with standard care (SC), as defined by national guidelines.
Methods:
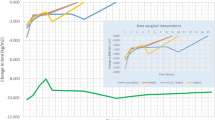
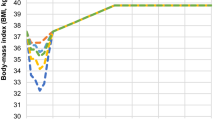
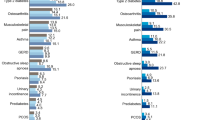
A Markov model was developed to calculate the incremental cost-effectiveness ratio (ICER), expressed as the cost per quality-adjusted life year (QALY) over the lifetime. The probabilities and quality-of-life utilities of outcomes were extrapolated from trial data using estimates from the published literature. A health sector perspective was adopted.
Results:
Over a patient’s lifetime, the CP resulted in an incremental cost saving of AUD 70 per patient, and an incremental 0.03 QALYs gained per patient. As such, the CP was found to be the dominant treatment, being more effective and less costly than SC (95% confidence interval: dominant to 6225 per QALY). Despite the CP delaying the onset of diabetes by ∼10 months, there was no significant difference in the incidence of type 2 diabetes, with the CP achieving <0.1% fewer cases than SC over the lifetime.
Conclusion:
The modelled results suggest that referral to community-based interventions may provide a highly cost-effective approach for those at high risk of weight-related comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
WHO. Obesity: preventing and managing the global epidemic. WHO Technical Report Series 894. World Health Organisation: Geneva, 2000.
Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011; 378: 1485–1492.
Lavin JH, Avery A, Whitehead SM, Rees E, Parsons J, Bagnall T et al. Feasibility and benefits of implementing a Slimming on Referral service in primary care using a commercial weight management partner. Public Health 2006; 120: 872–881.
Ahern AL, Olson AD, Aston LM, Jebb SA . Weight Watchers on prescription: an observational study of weight change among adults referred to Weight Watchers by the NHS. BMC Public Health 2011; 11: 434.
Fuller NR, Colagiuri S, Schofield D, Olson AD, Shrestha R, Holzapfel C et al. A within-trial cost-effectiveness analysis of primary care referral to a commercial provider for weight loss treatment, relative to standard care-an international randomised controlled trial. Int J Obes 2013; 37: 828–834.
Holzapfel C, Cresswell L, Ahern AL, Fuller NR, Eberhard MI, Stoll J et al. The challenge of two year follow-up after intervention for weight loss in primary care. Int J Obes 2013. e-pub ahead of print 13 September 2013; doi:10.1038/ijo.2013.180.
Cobiac L, Vos T, Veerman L . Cost-effectiveness of Weight Watchers and the Lighten Up to a Healthy Lifestyle program. Aust NZ J Public Health 2010; 34: 240–247.
Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL . Methods for the Economic Evaluation of Health Care Programmes 3rd edn. Oxford University Press, 2005.
Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM . Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med 2007; 147: 41–50.
Ara R, Blake L, Gray L, Hernandez M, Crowther M, Dunkley A et al. What is the clinical effectiveness and cost-effectiveness of using drugs in treating obese patients in primary care? A systematic review. Health Technol Assess 2012; 16, iii-xiv, 1–195.
Bray GA, Chatellier A, Duncan C, Greenway FL, Levy E, Ryan DH et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009; 374: 1677–1686.
IDI. Tracking the Accelerating Epidemic: Its Causes and Outcomes, The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) 2005,. Melbourne, 2006.
Keating CL, Dixon JB, Moodie ML, Peeters A, Bulfone L, Maglianno DJ et al. Cost-effectiveness of surgically induced weight loss for the management of type 2 diabetes: modeled lifetime analysis. Diabetes Care 2009; 32: 567–574.
Magliano DJ, Shaw JE, Shortreed SM, Nusselder WJ, Liew D, Barr ELM et al. Lifetime risk and projected population prevalence of diabetes. Diabetologia 2008; 51: 2179–2186.
Kolotkin RL, Crosby RD, Kosloski KD, Williams GR . Development of a brief measure to assess quality of life in obesity. Obes Res 2001; 9: 102–111.
Mueller A, Holzapfel C, Hauner H, Crosby RD, Engel SG, Muhlhans B et al. Psychometric evaluation of the German version of the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) Questionnaire. Exp Clin Endocrinol Diabetes 2011; 119: 69–74.
Brazier JE, Kolotkin RL, Crosby RD, Williams GR . Estimating a preference-based single index for the Impact of Weight on Quality of Life-Lite (IWQOL-lite) instrument from the SF-6D. Value Health 2004; 7: 490–498.
Lee CMY, Colagiuri R, Magliano DJ, Cameron AJ, Shaw J, Zimmet P et al. The cost of diabetes in adults in Australia. Diabetes Res Clin Pract 2013; 99: 385–390.
Colagiuri S, Lee CMY, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ et al. The cost of overweight and obesity in Australia. Med J Aust 2010; 192: 260–264.
AIHW. Health expenditure Australia 2010–11: Health and Welfare Expenditure Series no. 47. 2012 (accessed 12 December 2012); available from http://www.aihw.gov.au/publication-detail/?id=10737423009.
Laupacis A, Feeny D, Detsky AS, Tugwell PX . How attractive does a new technology have to be to warrant adoption and utilization - tentative guidelines for using clinical and economic evaulations. Can Med Assoc J 1992; 146: 473–481.
Salem L, Jensen CC, Flum DR . Are bariatric surgical outcomes worth their cost? A systematic review. J Am Coll Surg 2005; 200: 270–278.
George B, Harris A, Mitchell A . Cost effectiveness analysis and the consistency of decision making - evidence from pharmaceutical reimbursement in Australia (1991 to 1996). Pharmacoeconomics 2001; 19: 1103–1109.
Gibbs HD, Broom J, Brown J, Laws RA, Reckless JPD, Noble PA et al. A new evidence-based model for weight management in primary care: the Counterweight Programme. J Hum Nutr Diet 2004; 17: 191–208.
Trueman P, Haynes SM, Lyons GF, McCombie EL, McQuigg MSA, Mongia S et al. Long-term cost-effectiveness of weight management in primary care. Int J Clin Pract 2010; 64: 775–783.
Tsai AG, Wadden TA . Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005; 142: 56–66.
Forster M, Veerman JL, Barendregt JJ, Vos T . Cost-effectiveness of diet and exercise interventions to reduce overweight and obesity. Int J Obes 2011; 35: 1071–1078.
Roux L, Kuntz KM, Donaldson C, Goldie SJ . Economic evaluation of weight loss interventions in overweight and obese women. Obesity 2006; 14: 1093–1106.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess 2009; 13: 1–190.
Clegg A, Colquitt J, Sidhu M, Royle P, Walker A . Clinical and cost effectiveness of surgery for morbid obesity: a systematic review and economic evaluation. Int J Obes 2003; 27: 1167–1177.
DoHA. Medicare Benefits Schedule Book. Department of Health and Ageing, Australian Government; 2010 (cited 18 January 2011); Available from http://www.health.gov.au/internet/mbsonline/publishing.nsf/Content/Downloads-201011.
ATO. Claiming a deduction for car expenses using the cents per kilometre method. Canberra: Australian Taxation Office, Australian Government; 2009-10 (cited 25 February 2011); Available from http://www.ato.gov.au/individuals/content.asp?doc=/content/33874.htm.
Acknowledgements
We acknowledge the assistance of Crystal Lee who provided critical analysis of the draft manuscript; Kirsten Howard who reviewed the Markov model; and Catherine Keating for assistance with data acquisition.
Author contributions
NRF: acquisition of data, development of the Markov model, analysis and interpretation of data and writing of the manuscript; HC, SC and DS: development of the Markov model, interpretation of data, critical review and writing of the manuscript; SAJ and HH: study design and conception, obtained funding and critical review of the manuscript; IDC: study design and conception, obtained funding and writing the manuscript. All authors read and approved the final manuscript.
Trial Registration: This study is registered with the International Standard Register of Clinical Trials, ISRCTN 85485463.
Role of the Funding Source: This study was investigator initiated but funded by Weight Watchers International through a grant to the Medical Research Council (UK). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
NRF and IDC have received research grants for other clinical trials funded by Sanofi-Aventis, Allergan, Eli Lilly and Novo Nordisk. IDC was a board member for the SCOUT trial, is on the EXSCEL Operations Committee and has received payment for lectures from iNova Pharmaceuticals, Pfizer Australia and Servier Laboratories (Australia). SAJ has received research grants for other clinical trials from Sanofi-Aventis and Coca Cola, and is a member of the Tanita Medical Advisory Board and receives a fee for nutrition articles and lectures for Rosemary Conley Enterprises. HH is on the Advisory Board for Weight Watchers International and has received payment for lectures from Sara Lee, Novartis, Sanofi Aventis and Bristol-Myers Squibb.
Rights and permissions
About this article
Cite this article
Fuller, N., Carter, H., Schofield, D. et al. Cost effectiveness of primary care referral to a commercial provider for weight loss treatment, relative to standard care: a modelled lifetime analysis. Int J Obes 38, 1104–1109 (2014). https://doi.org/10.1038/ijo.2013.227
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.227
Keywords
This article is cited by
-
Cost-effectiveness of finerenone in chronic kidney disease associated with type 2 diabetes in The Netherlands
Cardiovascular Diabetology (2023)
-
Utility Decrements Associated with Adult Overweight and Obesity in Australia: A Systematic Review and Meta-Analysis
PharmacoEconomics (2021)