Abstract
Background:
The visceral adiposity index (VAI) and hypertriglyceridemic waist phenotype (the simultaneous presence of waist circumference (WC)⩾90/80 cm for men/women and plasma triglyceride (TG) concentration⩾1.7 mmol l−1 for both genders) have been identified as good indicators of visceral adiposity, which is an independent risk factor for diabetes. The Chinese population is characterized by a predominance of visceral fat accumulation despite having comparatively low weight. These two surrogate markers of visceral adiposity might effectively identify Chinese adults who are at risk of getting diabetes. We aimed to examine the association between VAI and risk of diabetes or between the hypertriglyceridemic waist phenotype and diabetes risk.
Methods:
We conducted a cross-sectional analysis of 7639 Chinese men and women aged ⩾18 years using data from the China Health and Nutrition Survey 2009. Logistic regression was used to evaluate the associations.
Results:
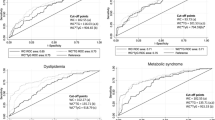
For men, compared with participants in the lowest quartile of VAI scores, the multivariable-adjusted odds ratios (ORs) (with 95% confidence intervals) for diagnosed diabetes were 1.1 (0.7–1.7), 1.9 (1.3–2.8) and 3.6 (2.5–5.3) for those in the second, third, and top quartile of VAI scores, respectively. For women, the corresponding figures were 0.9 (0.5–1.4), 1.7 (1.1–2.6) and 2.8 (1.9–4.2), respectively. The multivariate-adjusted ORs (with 95% confidence intervals) for diabetes in men with the hypertriglyceridemic waist phenotype compared with men with both WC and TG measurements below the defined cut points were 3.7 (2.6–5.4). For women, the corresponding figure was 3.7 (2.4–5.5). For both men and women, the associations between the 4th quartile of VAI scores and risk of diabetes or between the hypertriglyceridemic waist phenotype and risk of diabetes were consistently seen in various subgroups.
Conclusion:
Among Chinese adults, high VAI scores and the hypertriglyceridemic waist phenotype are strongly associated with diabetes risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J et al. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–1101.
Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993-2009. Obes Rev 2012; 13: 287–296.
Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010; 362: 800–811.
Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA 2012; 308: 1150–1159.
Hu D, Xie J, Fu P, Zhou J, Yu D, Whelton PK et al. Central rather than overall obesity is related to diabetes in the Chinese population: the InterASIA study. Obesity (Silver Spring) 2007; 15: 2809–2816.
Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am J Clin Nutr 2012; 96: 714–726.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010; 33: 920–922.
Lemieux I, Pascot A, Couillard C, Lamarche B, Tchernof A, Almeras N et al. Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation 2000; 102: 179–184.
Popkin BM, Du S, Zhai F, Zhang B . Cohort Profile: The China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol 2010; 39: 1435–1440.
Zhou BF . Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002; 15: 83–96.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33: S62–S69.
Bagley SC, White H, Golomb BA . Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol 2001; 54: 979–985.
Abbate LM, Stevens J, Schwartz TA, Renner JB, Helmick CG, Jordan JM . Anthropometric measures, body composition, body fat distribution, and knee osteoarthritis in women. Obesity (Silver Spring) 2006; 14: 1274–1281.
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Charalampidis P, Livadas S et al. Visceral adiposity index is highly associated with adiponectin values and glycaemic disturbances. Eur J Clin Invest 2013; 43: 183–189.
Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH et al. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006; 368: 1681–1688.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003; 289: 76–79.
Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G . Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J Clin Invest 1997; 100: 1166–1173.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med 2008; 168: 1617–1624.
Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med 2008; 168: 1609–1616.
Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes (Lond) 2011; 35: 971–981.
Smith JD, Borel AL, Nazare JA, Haffner SM, Balkau B, Ross R et al. Visceral adipose tissue indicates the severity of cardiometabolic risk in patients with and without type 2 diabetes: results from the INSPIRE ME IAA study. J Clin Endocrinol Metab 2012; 97: 1517–1525.
Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab 2010; 95: 5419–5426.
Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation 2003; 108: 1718–1723.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007; 116: 39–48.
Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L . Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care 2000; 23: 465–471.
Hajer GR, van Haeften TW, Visseren FL . Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J 2008; 29: 2959–2971.
Reaven GM . The kidney: an unwilling accomplice in syndrome X. Am J Kidney Dis 1997; 30: 928–931.
Gastaldelli A, Miyazaki Y, Pettiti M, Matsuda M, Mahankali S, Santini E et al. Metabolic effects of visceral fat accumulation in type 2 diabetes. J Clin Endocrinol Metab 2002; 87: 5098–5103.
Zhang X, Shu XO, Li H, Yang G, Xiang YB, Cai Q et al. Visceral adiposity and risk of coronary heart disease in relatively lean Chinese adults. Int J Cardiol 2013 e-pub ahead of print 2013 doi:10.1016/j.ijcard.2013.01.275.
Oh JY, Sung YA, Lee HJ . The visceral adiposity index as a predictor of insulin resistance in young women with polycystic ovary syndrome. Obesity (Silver Spring) 2012; 21: 1690–1694.
Tanko LB, Bagger YZ, Qin G, Alexandersen P, Larsen PJ, Christiansen C . Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 2005; 111: 1883–1890.
Sam S, Haffner S, Davidson MH, D'Agostino RB Sr., Feinstein S, Kondos G et al. Hypertriglyceridemic waist phenotype predicts increased visceral fat in subjects with type 2 diabetes. Diabetes Care 2009; 32: 1916–1920.
Czernichow S, Bruckert E, Bertrais S, Galan P, Hercberg S, Oppert JM . Hypertriglyceridemic waist and 7.5-year prospective risk of cardiovascular disease in asymptomatic middle-aged men. Int J Obes (Lond) 2007; 31: 791–796.
Arsenault BJ, Lemieux I, Despres JP, Wareham NJ, Kastelein JJ, Khaw KT et al. The hypertriglyceridemic-waist phenotype and the risk of coronary artery disease: results from the EPIC-Norfolk prospective population study. CMAJ 2010; 182: 1427–1432.
Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ et al. Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: a report from the Women's Ischemia Syndrome Evaluation (WISE) study. Circulation 2004; 109: 706–713.
Katzmarzyk PT, Janssen I, Ross R, Church TS, Blair SN . The importance of waist circumference in the definition of metabolic syndrome: prospective analyses of mortality in men. Diabetes Care 2006; 29: 404–409.
Kahn HS, Cheng YJ . Longitudinal changes in BMI and in an index estimating excess lipids among white and black adults in the United States. Int J Obes (Lond) 2008; 32: 136–143.
Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D'Agostino RB Sr. . Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med 2007; 167: 1068–1074.
Sattar N, Gaw A, Scherbakova O, Ford I, O'Reilly DS, Haffner SM et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 2003; 108: 414–419.
Acknowledgements
We thank the China Health and Nutrition Survey, supported by the NIH (R01-HD30880, DK056350 and R01-HD38700), and the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, Carolina Population Center, the University of North Carolina at Chapel Hill and the Fogarty International Center for providing the data used here. We also thank the China-Japan Friendship Hospital and the Ministry of Health for support for the CHNS 2009 survey. The study was supported by National Natural Science Foundation of China 30772207.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Du, T., Sun, X., Huo, R. et al. Visceral adiposity index, hypertriglyceridemic waist and risk of diabetes: the China Health and Nutrition Survey 2009. Int J Obes 38, 840–847 (2014). https://doi.org/10.1038/ijo.2013.181
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.181
Keywords
This article is cited by
-
Role of interventional radiology in upper abdominal cancer pain management
Egyptian Journal of Radiology and Nuclear Medicine (2023)
-
Assessing temporal differences in the predictive power of baseline TyG-related parameters for future diabetes: an analysis using time-dependent receiver operating characteristics
Journal of Translational Medicine (2023)
-
Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou Heart Study
Cardiovascular Diabetology (2022)
-
Creatinine index as a predictive marker of sarcopenia in patients under hemodialysis
International Urology and Nephrology (2022)
-
Association of “hypertriglyceridemic waist” with increased 5-year risk of subclinical atherosclerosis in a multi-ethnic population: a prospective cohort study
BMC Cardiovascular Disorders (2021)