Abstract
Objective:
To identify factors contributing to the variation in weight loss after Roux-en-Y gastric bypass (RYGB).
Design:
Cross-sectional study of patients with good (excess body mass index lost (EBL) >60%) and poor weight loss response (EBL <50%) >12 months after RYGB and a lean control group matched for age and gender.
Materials and methods:
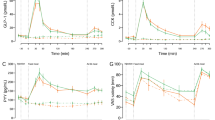
Sixteen patients with good weight loss response, 17 patients with poor weight loss response, and eight control subjects were included in the study. Participants underwent dual energy X-ray absorptiometry scan, indirect calorimetry and a 9 h multiple-meal test with measurements of glucose, insulin, total bile acids (TBA), glucagon-like peptide (GLP)-1, peptide YY3–36 (PYY), cholecystokinin (CCK), ghrelin, neurotensin and pancreatic polypeptide (PP) as well as assessment of early dumping and appetite.
Results:
Suppression of hunger was more pronounced in the good than the poor responders in response to the multiple-meal test (P=0.006). In addition, the good responders had a larger release of GLP-1 (P=0.009) and a greater suppression of ghrelin (P=0.037) during the test, whereas the postprandial secretion of CCK was highest in the poor responders (P=0.005). PYY, neurotensin, PP and TBA release did not differ between the RYGB-operated groups. Compared with control subjects, patients had exaggerated release of GLP-1 (P<0.001), PYY (P=0.008), CCK (P=0.010) and neurotensin (P<0.001). Early dumping was comparable in the good and poor responders, but more pronounced than in controlled subjects. Differences in resting energy expenditure between the three groups were entirely explained by differences in body composition.
Conclusion:
Favorable meal-induced changes in hunger and gut hormone release in patients with good compared with poor weight loss response support the role of gut hormones in the weight loss after RYGB.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752.
Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, Pareja JC . Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg 2008; 18: 648–651.
Christou NV, Look D, Maclean LD . Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg 2006; 244: 734–740.
Bueter M, Ashrafian H, Le Roux CW . Mechanisms of weight loss after gastric bypass and gastric banding. Obesity Facts 2009; 2: 325–331.
Borg CM, Le Roux CW, Ghatei Ma, Bloom SR, Patel a G, Aylwin SJB . Progressive rise in gut hormone levels after Roux-en-Y gastric bypass suggests gut adaptation and explains altered satiety. Br J Surg 2006; 93: 210–215.
Le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A et al. Gut hormones as mediators of appetite and weight loss after roux-en-y gastric bypass. Ann Surg 2007; 246: 780–785.
Olbers T, Björkman S, Lindroos A, Maleckas A, Lönn L, Sjöström L et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg 2006; 244: 715–722.
Halmi KA, Mason E, Falk JR, Stunkard A . Appetitive behavior after gastric bypass for obesity. Int J Obes 1981; 5: 457–464.
Laurenius a, Larsson I, Bueter M, Melanson KJ, Bosaeus I, Forslund HB et al. Changes in eating behaviour and meal pattern following Roux-en-Y gastric bypass. Int J Obes 2012; 36: 348–355.
Van der Kleij FG, Vecht J, Lamers CB, Masclee AA . Diagnostic value of dumping provocation in patients after gastric surgery. Scand J Gastroenterol 1996; 31: 1162–1166.
Sarwer DB, Dilks RJ, West-Smith L . Dietary intake and eating behavior after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis 2011; 7: 644–651.
Miras A, Jackson R . Gastric bypass surgery for obesity decreases the reward value of a sweet-fat stimulus as assessed in a progressive ratio task. Am J Clin Nutr 2012; 96: 467–473.
Burge JC, Schaumburg JZ, Choban PS, DiSilvestro RA, Flancbaum L . Changes in patients’ taste acuity after Roux-en-Y gastric bypass for clinically severe obesity. J Am Diet Assoc 1995; 95: 666–670.
Jacobsen SH, Olesen SC, Dirksen C, Jørgensen NB, Bojsen-Møller KN, Kielgast U et al. Changes in gastrointestinal hormone responses, insulin sensitivity, and beta-cell function within 2 weeks after gastric bypass in non-diabetic subjects. Obes Surg 2012; 22: 1084–1096.
Ochner CN, Gibson C, Shanik M, Goel V, Geliebter A . Changes in neurohormonal gut peptides following bariatric surgery. Int J Obes 2011; 35: 153–166.
Ybarra J, Bobbioni-Harsch E, Chassot G, Huber O, Morel P, Assimacopoulos-Jeannet F et al. Persistent correlation of ghrelin plasma levels with body mass index both in stable weight conditions and during gastric-bypass-induced weight loss. Obes Surg 2009; 19: 327–331.
Sundbom M, Holdstock C, Engström BE, Karlsson FA . Early changes in ghrelin following Roux-en-Y gastric bypass: influence of vagal nerve functionality? Obes Surg 2007; 17: 304–310.
Peterli R, Steinert RE, Woelnerhanssen B, Peters T, Christoffel-Courtin C, Gass M et al. Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial. Obes Surg 2012; 22: 740–748.
Bueter M, Löwenstein C, Olbers T, Wang M, Cluny NL, Bloom SR et al. Gastric bypass increases energy expenditure in rats. Gastroenterology 2010; 138: 1845–1853.
Patti M-E, Houten SM, Bianco AC, Bernier R, Larsen PR, Holst JJ et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring) 2009; 17: 1671–1677.
Pournaras DJ, Glicksman C, Vincent RP, Kuganolipava S, Alaghband-Zadeh J, Mahon D et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology 2012; 153: 3613–3619.
Jørgensen NB, Jacobsen SH, Dirksen C, Bojsen-Møller KN, Naver L, Hvolris L et al. Acute and long-term effects of Roux-en-Y gastric bypass on glucose metabolism in subjects with Type 2 diabetes and normal glucose tolerance. Am J Physiol Endocrinol Metab 2012; 303: E122–E131.
WEIR JBDB . New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 1949; 109: 1–9.
Orskov C, Rabenhøj L, Wettergren A, Kofod H, Holst JJ . Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes 1994; 43: 535–539.
Rehfeld JF . How to measure cholecystokinin in tissue, plasma and cerebrospinal fluid. Regul Pept 1998; 78: 31–39.
Rehfeld JF, Sun G, Christensen T, Hillingsø JG . The predominant cholecystokinin in human plasma and intestine is cholecystokinin-33. J Clin Endocrinol Metab 2001; 86: 251–258.
Wallace TM, Levy JC, Matthews DR . Use and abuse of HOMA modeling. Diabetes Care 2004; 27: 1487–1495.
Morínigo R, Moizé V, Musri M, Lacy AM, Navarro S, Marín JL et al. Glucagon-like peptide-1, peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab 2006; 91: 1735–1740.
Falkén Y, Hellström PM, Holst JJ, Näslund E . Changes in glucose homeostasis after Roux-en-Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab 2011; 96: 2227–2235.
Mechanick JI, Kushner RF, Sugerman HJ, Gonzalez-Campoy JM, Collazo-Clavell ML, Guven S et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic and Bariatric Surgery Medical Guidelines for Clinical Practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric. Obesity (Silver Spring) 2008; 4: S109–S184.
Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL et al. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature 418: 650–654 2002.
Verdich C, Flint A, Gutzwiller JP, Näslund E, Beglinger C, Hellström PM et al. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J Clin Endocrinol Metab 2001; 86: 4382–4389.
De Silva A, Salem V, Long CJ, Makwana A, Newbould RD, Rabiner Ea et al. The gut hormones PYY 3-36 and GLP-1 7-36 amide reduce food intake and modulate brain activity in appetite centers in humans. Cell Metab 2011; 14: 700–706.
Neary NM, Small CJ, Druce MR, Park AJ, Ellis SM, Semjonous NM et al. Peptide YY3-36 and glucagon-like peptide-17-36 inhibit food intake additively. Endocrinology 2005; 146: 5120–5127.
Christ-Crain M, Stoeckli R, Ernst A, Morgenthaler NG, Bilz S, Korbonits M et al. Effect of gastric bypass and gastric banding on proneurotensin levels in morbidly obese patients. J Clin Endocrinol Metab 2006; 91: 3544–3547.
Holdstock C, Zethelius B, Sundbom M, Karlsson Fa, Edén Engström B . Postprandial changes in gut regulatory peptides in gastric bypass patients. Int J Obes 2008; 32: 1640–1646.
Habib AM, Richards P, Cairns LS, Rogers GJ, Bannon CaM, Parker HE et al. Overlap of endocrine hormone expression in the mouse intestine revealed by transcriptional profiling and flow cytometry. Endocrinology 2012; 153: 3054–3065.
Rehfeld JF . Cholecystokinin as satiety signal. Int J Obes 1981; 5: 465–469.
Patterson M, Bloom SR, Gardiner JV . Ghrelin and appetite control in humans—potential application in the treatment of obesity. Peptides 2011; 32: 2290–2294.
Pérez-Romero N, Serra A, Granada ML, Rull M, Alastrué A, Navarro-Díaz M et al. Effects of two variants of Roux-en-Y Gastric bypass on metabolism behaviour: focus on plasma ghrelin concentrations over a 2-year follow-up. Obes Surg 2010; 20: 600–609.
Matzko ME, Argyropoulos G, Wood GC, Chu X, McCarter RJM, Still CD et al. Association of ghrelin receptor promoter polymorphisms with weight loss following Roux-en-Y gastric bypass surgery. Obes Surg 2012; 22: 783–790.
Le Roux CW, Patterson M, Vincent RP, Hunt C, Ghatei Ma, Bloom SR . Postprandial plasma ghrelin is suppressed proportional to meal calorie content in normal-weight but not obese subjects. J Clin Endocrinol Metab 2005; 90: 1068–1071.
Engström BE, Ohrvall M, Sundbom M, Lind L, Karlsson Fa . Meal suppression of circulating ghrelin is normalized in obese individuals following gastric bypass surgery. Int J Obes 2007; 31: 476–480.
Korner J, Inabnet W, Conwell IM, Taveras C, Daud A, Olivero-Rivera L et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity (Silver Spring) 2006; 14: 1553–1561.
Schwartz TW, Rehfeld JF, Stadil F, Larson LI, Chance RE, Moon N . Pancreatic-polypeptide response to food in duodenal-ulcer patients before and after vagotomy. Lancet 1976; 1: 1102–1105.
Prawitt J, Caron S, Staels B . Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diab Rep 2011; 11: 160–166.
Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, Rizzo G et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 2009; 10: 167–177.
Goldfine a B, Mun EC, Devine E, Bernier R, Baz-Hecht M, Jones DB et al. Patients with neuroglycopenia after gastric bypass surgery have exaggerated incretin and insulin secretory responses to a mixed meal. J Clin Endocrinol Metab 2007; 92: 4678–4685.
Tamboli Ra, Hossain HA, Marks Pa, Eckhauser AW, Rathmacher Ja, Phillips SE et al. Body composition and energy metabolism following Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 2010; 18: 1718–1724.
Das SK, Roberts SB, McCrory Ma, Hsu LKG, Shikora Sa, Kehayias JJ et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr 2003; 78: 22–30.
Kahn SE . The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 2003; 46: 3–19.
Acknowledgements
The authors are grateful for technical assistance to Alis Andersen and Dorthe Baunbjerg (Department of Endocrinolgy, Hvidovre Hospital, Denmark), Lene Albak and Sofie Pilgaard (Department of Biomedical Sciences, the Panum Institute, University of Copenhagen, Denmark), Rikke Kröncke (Department of Clinical Biochemistry, Rigshospitalet, Denmark) and Gitte Kølander Hansen (Diabetes and Obesity Biology, Novo Nordisk, Denmark). The present study was carried out as a part of UNIK: Food, Fitness and Pharma for Health and Disease at the University of Copenhagen (www.foodfitnesspharma.ku.dk). The UNIK project is funded by the Danish Ministry of Science, Technology and Innovation. Further funding was received from the Strategic Research Council for the Capital Area and Hvidovre Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Carsten Dirksen, Kirstine N Bojsen-Møller, Nils B Jørgensen, Siv H Jacobsen, Bolette Hartmann and Jens J Holst are affiliated with the Novo Nordisk Foundation Centre for Basic Metabolic Research, which is funded by the Novo Nordisk Foundation. Nils B Jørgensen and Siv H Jacobsen have one-third of their PhD scholarship funded by Novo Nordisk A/S. Trine R Clausen is employed by Novo Nordisk A/S and owns stock in Novo Nordisk A/S and Zealand Pharma A/S. Urd Kielgast, Dorte Worm, Jens F Rehfeld, Morten Damgaard, Jan L Madsen, Sten Madsbad and Dorte L Hansen declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dirksen, C., Jørgensen, N., Bojsen-Møller, K. et al. Gut hormones, early dumping and resting energy expenditure in patients with good and poor weight loss response after Roux-en-Y gastric bypass. Int J Obes 37, 1452–1459 (2013). https://doi.org/10.1038/ijo.2013.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.15
Keywords
This article is cited by
-
Post metabolic bariatric surgery weight regain: the importance of GLP-1 levels
International Journal of Obesity (2024)
-
Food preferences after bariatric surgery: a review update
Internal and Emergency Medicine (2023)
-
Primary weight loss failure after Roux-en-Y gastric bypass is characterized by impaired gut-hormone mediated regulation of food intake
International Journal of Obesity (2023)
-
Early effects of Roux-en-Y gastric bypass on dietary fatty acid absorption and metabolism in people with obesity and normal glucose tolerance
International Journal of Obesity (2022)
-
Appetite Changes in Weight Regain and Weight Maintenance After Roux-en-Y Gastric Bypass
Obesity Surgery (2022)