Abstract
Objective:
To investigate the influence of adiposity on patterns of sex hormones across the menstrual cycle among regularly menstruating women.
Subjects:
The BioCycle Study followed 239 healthy women for 1–2 menstrual cycles, with up to eight visits per cycle timed using fertility monitors.
Methods:
Serum estradiol (E2), progesterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH) and sex hormone-binding globulin (SHBG) were measured at each visit. Adiposity was measured by anthropometry and by dual energy X-ray absorptiometry (DXA). Differences in hormonal patterns by adiposity measures were estimated using nonlinear mixed models, which allow for comparisons in overall mean levels, amplitude (i.e., lowest to highest level within each cycle) and shifts in timing of peaks while adjusting for age, race, energy intake and physical activity.
Results:
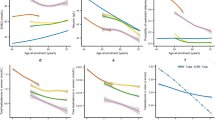
Compared with normal weight women (n=154), obese women (body mass index (BMI) ⩾30 kg m−2, n=25) averaged lower levels of progesterone (−15%, P=0.003), LH (−17%, P=0.01), FSH (−23%, P=0.001) and higher free E2 (+22%, P=0.0001) across the cycle. To lesser magnitudes, overweight women (BMI: 25–30, n=60) also exhibited differences in the same directions for mean levels of free E2, FSH and LH. Obese women experienced greater changes in amplitude of LH (9%, P=0.002) and FSH (8%, P=0.004), but no differences were observed among overweight women. Higher central adiposity by top compared to bottom tertile of trunk-to-leg fat ratio by DXA was associated with lower total E2 (−14%, P=0.005), and FSH (−15%, P=0.001). Peaks in FSH and LH occurred later (∼0.5 day) in the cycle among women with greater central adiposity.
Conclusion:
Greater total and central adiposity were associated with changes in mean hormone levels. The greater amplitudes observed among obese women suggest compensatory mechanisms at work to maintain hormonal homeostasis. Central adiposity may be more important in influencing timing of hormonal peaks than total adiposity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Flegal KM, Carroll MD, Ogden CL, Curtin LR . Prevalence and trends in obesity among US adults, 1999–2008. JAMA 2010; 303: 235–241.
Ziomkiewicz A, Ellison PT, Lipson SF, Thune I, Jasienska G . Body fat, energy balance and estradiol levels: a study based on hormonal profiles from complete menstrual cycles. Hum Reprod 2008; 23: 2555–2563.
Wu F, Ames R, Evans MC, France JT, Reid IR . Determinants of sex hormone-binding globulin in normal postmenopausal women. Clin Endocrinol (Oxf) 2001; 54: 81–87.
Fishman J, Boyar RM, Hellman L . Influence of body weight on estradiol metabolism in young women. J Clin Endocrinol Metab 1975; 41: 989–991.
Dorgan JF, Reichman ME, Judd JT, Brown C, Longcope C, Schatzkin A et al. The relation of body size to plasma levels of estrogens and androgens in premenopausal women (Maryland, United States). Cancer Causes Control 1995; 6: 3–8.
Grenman S, Ronnemaa T, Irjala K, Kaihola HL, Gronroos M . Sex steroid, gonadotropin, cortisol, and prolactin levels in healthy, massively obese women: correlation with abdominal fat cell size and effect of weight reduction. J Clin Endocrinol Metab 1986; 63: 1257–1261.
Randolph Jr JF, Sowers M, Gold EB, Mohr BA, Luborsky J, Santoro N et al. Reproductive hormones in the early menopausal transition: relationship to ethnicity, body size, and menopausal status. J Clin Endocrinol Metab 2003; 88: 1516–1522.
Tworoger SS, Eliassen AH, Missmer SA, Baer H, Rich-Edwards J, Michels KB et al. Birthweight and body size throughout life in relation to sex hormones and prolactin concentrations in premenopausal women. Cancer Epidemiol Biomarkers Prev 2006; 15: 2494–2501.
Bohlke K, Cramer DW, Barbieri RL . Relation of luteinizing hormone levels to body mass index in premenopausal women. Fertil Steril 1998; 69: 500–504.
Jain A, Polotsky AJ, Rochester D, Berga SL, Loucks T, Zeitlian G et al. Pulsatile luteinizing hormone amplitude and progesterone metabolite excretion are reduced in obese women. J Clin Endocrinol Metab 2007; 92: 2468–2473.
Schisterman EF, Gaskins AJ, Mumford SL, Browne RW, Yeung E, Trevisan M et al. Influence of endogenous reproductive hormones on F2-isoprostane levels in premenopausal women: the BioCycle Study. Am J Epidemiol 2010; 172: 430–439.
Wactawski-Wende J, Schisterman EF, Hovey KM, Howards PP, Browne RW, Hediger M et al. BioCycle study: design of the longitudinal study of the oxidative stress and hormone variation during the menstrual cycle. Paediatr Perinat Epidemiol 2009; 23: 171–184.
Howards PP, Schisterman EF, Wactawski-Wende J, Reschke JE, Frazer AA, Hovey KM . Timing clinic visits to phases of the menstrual cycle by using a fertility monitor: the BioCycle Study. Am J Epidemiol 2009; 169: 105–112.
Mumford SL, Schisterman EF, Gaskins AJ, Pollack AZ, Perkins NJ, Whitcomb BW et al. Realignment and multiple imputation of longitudinal data: an application to menstrual cycle data. Paediatr Perinat Epidemiol 2011; 25: 448–459.
Lohman TG, Roche AF, Martorell R (eds). Anthropometric Standardization Reference Manual. Human Kinetics Books: Champaign, IL: 1988.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395.
Wallace TM, Levy JC, Matthews DR . Use and abuse of HOMA modeling. Diabetes Care 2004; 27: 1487–1495.
Sodergard R, Backstrom T, Shanbhag V, Carstensen H . Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem 1982; 16: 801–810.
Albert PS, Hunsberger S . On analyzing circadian rhythms data using nonlinear mixed models with harmonic terms. Biometrics 2005; 61: 1115–1120.
Gaskins AJ, Mumford SL, Zhang C, Wactawski-Wende J, Hovey KM, Whitcomb BW et al. Effect of daily fiber intake on reproductive function: the BioCycle Study. Am J Clin Nutr 2009; 90: 1061–1069.
Hall J . Neuroendocrine control of the menstrual cycle. In: Strauss III J, Barbieri R (eds) Yen and Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Saunders: Philadelphia, 2004. pp 195–211.
Moschos S, Chan JL, Mantzoros CS . Leptin and reproduction: a review. Fertil Steril 2002; 77: 433–444.
Hutchison JS, Zeleznik AJ . The corpus luteum of the primate menstrual cycle is capable of recovering from a transient withdrawal of pituitary gonadotropin support. Endocrinology 1985; 117: 1043–1049.
Strauss III J, Williams C . The ovarian life cycle. In: Strauss III J, Barbieri R (eds) Yen and Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Saunders: Philadelphia, 2004. pp 213–253.
Santoro N, Lasley B, McConnell D, Allsworth J, Crawford S, Gold EB et al. Body size and ethnicity are associated with menstrual cycle alterations in women in the early menopausal transition: The Study of Women's Health across the Nation (SWAN) Daily Hormone Study. J Clin Endocrinol Metab 2004; 89: 2622–2631.
Williams AE, Maskarinec G, Franke AA, Stanczyk FZ . The temporal reliability of serum estrogens, progesterone, gonadotropins, SHBG and urinary estrogen and progesterone metabolites in premenopausal women. BMC Womens Health 2002; 2: 13.
Lovejoy JC, Sainsbury A . Sex differences in obesity and the regulation of energy homeostasis. Obes Rev 2009; 10: 154–167.
Clegg DJ, Brown LM, Woods SC, Benoit SC . Gonadal hormones determine sensitivity to central leptin and insulin. Diabetes 2006; 55: 978–987.
Acknowledgements
This work was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health. We thank the BioCycle working group for comments and feedback on this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Yeung, E., Zhang, C., Albert, P. et al. Adiposity and sex hormones across the menstrual cycle: the BioCycle Study. Int J Obes 37, 237–243 (2013). https://doi.org/10.1038/ijo.2012.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.9
Keywords
This article is cited by
-
Obesity: sex and sympathetics
Biology of Sex Differences (2020)
-
Sex hormone-binding globulin provides a novel entry pathway for estradiol and influences subsequent signaling in lymphocytes via membrane receptor
Scientific Reports (2019)
-
Maternal Pre-pregnancy BMI and Reproductive Health of Daughters in Young Adulthood
Maternal and Child Health Journal (2016)