Abstract
INTRODUCTION AND OBJECTIVES:
An obese-type human microbiota with an increased Firmicutes:Bacteroidetes ratio has been described that may link the gut microbiome with obesity and metabolic syndrome (MetS) development. Dietary fat and carbohydrate are modifiable risk factors that may impact on MetS by altering the human microbiome composition. We determined the effect of the amount and type of dietary fat and carbohydrate on faecal bacteria and short chain fatty acid (SCFA) concentrations in people ‘at risk’ of MetS.
DESIGN:
A total of 88 subjects at increased MetS risk were fed a high saturated fat diet (HS) for 4 weeks (baseline), then randomised onto one of the five experimental diets for 24 weeks: HS; high monounsaturated fat (MUFA)/high glycemic index (GI) (HM/HGI); high MUFA/low GI (HM/LGI); high carbohydrate (CHO)/high GI (HC/HGI); and high CHO/low GI (HC/LGI). Dietary intakes, MetS biomarkers, faecal bacteriology and SCFA concentrations were monitored.
RESULTS:
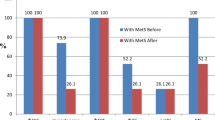
High MUFA diets did not affect individual bacterial population numbers but reduced total bacteria and plasma total and LDL-cholesterol. The low fat, HC diets increased faecal Bifidobacterium (P=0.005, for HC/HGI; P=0.052, for HC/LGI) and reduced fasting glucose and cholesterol compared to baseline. HC/HGI also increased faecal Bacteroides (P=0.038), whereas HC/LGI and HS increased Faecalibacterium prausnitzii (P=0.022 for HC/HGI and P=0.018, for HS). Importantly, changes in faecal Bacteroides numbers correlated inversely with body weight (r=−0.64). A total bacteria reduction was observed for high fat diets HM/HGI and HM/LGI (P=0.023 and P=0.005, respectively) and HS increased faecal SCFA concentrations (P<0.01).
CONCLUSION:
This study provides new evidence from a large-scale dietary intervention study that HC diets, irrespective of GI, can modulate human faecal saccharolytic bacteria, including bacteroides and bifidobacteria. Conversely, high fat diets reduced bacterial numbers, and in the HS diet, increased excretion of SCFA, which may suggest a compensatory mechanism to eliminate excess dietary energy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
The NHS Information Centre, Lifestyles Statistics (10 February 2010). The Health and Social Care Information Centre. Statistics on obesity, physical activity and diet: England, 2010. Available at http://www.ic.nhs.uk/webfiles/publications/opad10/Statistics_on_Obesity_Physical_Activity_and_Diet_England_2010.pdf.
Balkau B, Charles MA, Drivsholm T, Borch-Johnsen K, Wareham N, Yudkin JS et al. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab 2002; 28: 364–376.
Reaven GM . Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
Stern MP . Do non-insulin-dependent diabetes mellitus and cardiovascular disease share common antecedents? Ann Intern Med 1996; 124: 110–116.
Gardner CD, Kraemer HC . Monounsaturated versus polyunsaturated dietary fat and serum lipids. A meta-analysis. Arterioscler Thromb Vasc Biol 1995; 15: 1917–1927.
Laaksonen M, Prättälä R, Karisto A . Patterns of unhealthy behaviour in Finland. Eur J Public Health 2001; 11: 294–300.
Conterno L, Fava F, Viola R, Tuohy KM . Obesity and the gut microbiota: does up-regulating colonic fermentation protect against obesity and metabolic disease? Genes Nutr 2011; 6: 241–260.
Ley RE . Obesity and the human microbiome. Curr Opin Gastroenterol 2010; 26: 5–11.
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007; 56: 1761–1772.
Dumas ME, Barton RH, Toye A, Cloarec O, Blancher C, Rothwell A et al. Metabolic profiling reveals a contribution of gut microbiota to fatty liver phenotype in insulin-resistant mice. Proc Natl Acad Sci USA 2006; 103: 12511–12516.
Murphy EF, Cotter PD, Healy S, Marques TM, O’Sullivan O, Fouhy F et al. Composition and energy harvesting capacity of the gut microbiota: relationship to diet, obesity and time in mouse models. Gut 2010; 59: 1635–1642.
Ley RE, Bäckhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI . Obesity alters gut microbial ecology. Proc Natl Acad Sci USA 2005; 102: 11070–11075.
Waldram A, Holmes E, Wang Y, Rantalainen M, Wilson ID, Tuohy KM et al. Top-down systems biology modeling of host metabotype-microbiome associations in obese rodents. J Proteome Res 2009; 8: 2361–2375.
Turnbaugh PJ, Bäckhed F, Fulton L, Gordon JI . Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 2008; 3: 213–223.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI . An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006; 444: 1027–1031.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI . Microbial ecology: human gut microbes associated with obesity. Nature 2006; 444: 1022–1023.
Duncan SH, Belenguer A, Holtrop G, Johnstone AM, Flint HJ, Lobley GE . Reduced dietary intake of carbohydrates by obese subjects results in decreased concentrations of butyrate and butyrate-producing bacteria in feces. Appl Environ Microbiol 2007; 73: 1073–1078.
Brinkworth GD, Noakes M, Clifton PM, Bird AR . Comparative effects of very low-carbohydrate, high-fat and high-carbohydrate, low-fat weight-loss diets on bowel habit and faecal short-chain fatty acids and bacterial populations. Br J Nutr 2009; 101: 1493–1502.
Schwiertz A, Taras D, Schäfer K, Beijer S, Bos NA, Donus C et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity 2010; 18: 190–195.
Jackson KG, Taylor GR, Clohessy AM, Williams CM . The effect of the daily intake of inulin on fasting lipid, insulin and glucose concentrations in middle-aged men and women. Br J Nutr 1999; 82: 23–30.
Balcázar-Muñoz BR, Martínez-Abundis E, González-Ortiz M . Effect of oral inulin administration on lipid profile and insulin sensitivity in subjects with obesity and dyslipidemia. Rev Med Chil 2003; 131: 597–604.
Cani PD, Neyrinck AM, Fava F, Knauf C, Burcelin RG, Tuohy KM et al. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 2007; 50: 2374–2383.
Cani PD, Possemiers S, Van de Wiele T, Guiot Y, Everard A, Rottier O et al. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut 2009; 58: 1091–1103.
Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011; 472: 57–63.
Jebb SA, Lovegrove JA, Griffin BA, Frost GS, Moore CS, Chatfield MD et al. Effect of changing the amount and type of fat and carbohydrate on insulin sensitivity and cardiovascular risk: the RISCK (Reading, Imperial, Surrey, Cambridge, and Kings) trial. Am J Clin Nutr 2010; 92: 748–758.
Moore C, Gitau R, Goff L, Lewis FJ, Griffin MD, Chatfield MD et al. Successful manipulation of the quality and quantity of fat and carbohydrate consumed by free-living individuals using a food exchange model. J Nutr 2009; 139: 1534–1540.
Jebb SA . Dietary determinants of obesity. Obes Rev 2007; 8 (Suppl 1): 93–97.
National Diet and Nutrition Survey (NDNS) 2004. Available from: http://tna.europarchive.org/20110116113217/. http://www.food.gov.uk/science/dietarysurveys/ndnsdocuments/.
National Food Survey (NFS). 1997-2000. Available from: http://tna.europarchive.org/20110116113217/. http://www.food.gov.uk/science/surveillance/.
Tuohy KM, Kolida S, Lustenberger AM, Gibson GR . The prebiotic effects of biscuits containing partially hydrolysed guar gum and fructo-oligosaccharides--a human volunteer study. Br J Nutr 2001; 86: 341–348.
Franks AH, Harmsen HJ, Raangs GC, Jansen GJ, Schut F, Welling GW . Variations of bacterial populations in human feces measured by fluorescent in situ hybridization with group-specific 16S rRNA-targeted oligonucleotide probes. Appl Environ Microbiol 1998; 64: 3336–3345.
Manz W, Amann R, Ludwig W, Vancanneyt M, Schleifer KH . Application of a suite of 16S rRNA-specific oligonucleotide probes designed to investigate bacteria of the phylum cytophaga-flavobacter-bacteroides in the natural environment. Microbiology 1996; 142: 1097–1106.
Hold GL, Schwiertz A, Aminov RI, Blaut M, Flint HJ . Oligonucleotide probes that detect quantitatively significant groups of butyrate-producing bacteria in human feces. Appl Environ Microbiol 2003; 69: 4320–4324.
Langendijk PS, Schut F, Jansen GJ, Raangs GC, Kamphuis GR, Wilkinson MH et al. Quantitative fluorescence in situ hybridization of Bifidobacterium spp. with genus-specific 16S rRNA-targeted probes and its application in fecal samples. Appl Environ Microbiol 1995; 61: 3069–3075.
Harmsen HJ, Wildeboer-Veloo AC, Grijpstra J, Knol J, Degener JE, Welling GW . Development of 16S rRNA-based probes for the Coriobacterium group and the Atopobium cluster and their application for enumeration of Coriobacteriaceae in human feces from volunteers of different age groups. Appl Environ Microbiol 2000; 66: 4523–4527.
Harmsen HJM, Elfferich P, Schut F, Welling GW . A 16S rRNA-targeted probe for detection of lactobacilli and enterococci in fecal samples by fluorescent in situ hybridization. Microb Ecol Health Dis 1999; 11: 3–12.
Franks AH, Harmsen HJ, Raangs GC, Jansen GJ, Schut F, Welling GW . Variations of bacterial populations in human feces measured by fluorescent in situ hybridization with group-specific 16S rRNA-targeted oligonucleotide probes. Appl Environ Microbiol 1998; 64: 3336–3345.
Icgen B, Moosa S, Harrison ST . A study of the relative dominance of selected anaerobic sulfate-reducing bacteria in a continuous bioreactor by fluorescence in situ hybridization. Microb Ecol 2007; 53: 43–52.
Ootsubo M, Shimizu T, Tanaka R, Sawabe T, Tajima K, Yoshimizu M et al. Oligonucleotide probe for detecting Enterobacteriaceae by in situ hybridization. J Appl Microbiol 2002; 93: 60–68.
Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI . Host-bacterial mutualism in the human intestine. Science 2005; 307: 1915–1920.
Chapman RW, Sillery JK, Graham MM, Saunders DR . Absorption of starch by healthy ileostomates: effect of transit time and of carbohydrate load. Am J Clin Nutr 1985; 41: 1244–1248.
Kolida S, Saulnier DM, Gibson GR . Gastrointestinal microflora: probiotics. Adv Appl Microbiol 2006; 59: 187–219.
Tuohy KM, Rouzaud GC, Brück WM, Gibson GR . Modulation of the human gut microflora towards improved health using prebiotics--assessment of efficacy. Curr Pharm Des 2005; 11: 75–90.
Vogt JA, Wolever TM . Fecal acetate is inversely related to acetate absorption from the human rectum and distal colon. J Nutr 2003; 133: 3145–3148.
Acknowledgements
We acknowledge the contribution of each RISCK study center member: University of Reading (Julie Lovegrove), Imperial College London (Gary Frost), University of Surrey (Bruce Griffin), MRC Unit of Human Nutrition Research, University of Cambridge (Susan Jebb, Carmel Moore) and Kings College London (Tom Sanders). In particular for the University of Reading: Julie A Lovegrove was the principal investigator for the Reading Centre, Rachel Gitau recruited the volunteers, run the dietary intervention and performed IVGTTs, Katie Newens helped with volunteer recruitment and IVGTTs, Francesca Fava helped with volunteer recruitment and IVGTTs, collected faecal samples, performed faecal microbiota analysis and wrote the manuscript, Kieran M Tuohy and Glenn R Gibson coordinated the faecal microbiota analysis and helped with writing of the manuscript. This study was supported by the UK Food Standards Agency (project NO2031). Foods were supplied by Unilever Food and Health Research Institute (Unilever R&D, Vlaardingen, Netherlands), Cereal Partners UK (Welwyn Garden City, Hertfordshire, UK), Grampian (Banff, UK), Weetabix Ltd (Kettering, UK) and Sainsbury's Supermarkets Ltd (London, UK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fava, F., Gitau, R., Griffin, B. et al. The type and quantity of dietary fat and carbohydrate alter faecal microbiome and short-chain fatty acid excretion in a metabolic syndrome ‘at-risk’ population. Int J Obes 37, 216–223 (2013). https://doi.org/10.1038/ijo.2012.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.33
Keywords
This article is cited by
-
Inflammatory crosstalk between saturated fatty acids and gut microbiota–white adipose tissue axis
European Journal of Nutrition (2023)
-
High-intensity mechanical bowel preparation before curative colorectal surgery is associated with poor long-term prognosis
International Journal of Colorectal Disease (2023)
-
Changes in the Gut Microbiota Composition and Their Relation to Dietary Intake After Bariatric Surgery
Obesity Surgery (2023)
-
Gut Microbiome and Its Impact on Obesity and Obesity-Related Disorders
Current Gastroenterology Reports (2023)
-
Position statement on nutrition therapy for overweight and obesity: nutrition department of the Brazilian association for the study of obesity and metabolic syndrome (ABESO—2022)
Diabetology & Metabolic Syndrome (2023)