Abstract
Objective:
To determine whether sleep timing behaviour is associated with energy intake and diet quality in children and adolescents.
Design:
Cross-sectional analysis of nationally representative survey data.
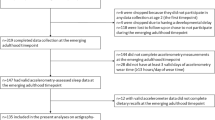
Sample:
A total of 2200 participants of the 2007 Australian National Children’s Nutrition and Physical Activity Survey aged 9–16 years with 2 days of food intake data, 4 days of use of time data and complete anthropometry. Participants were grouped into one of four sleep–wake behaviour categories: early bed–early rise (EE); early bed–late rise (EL); late bed–early rise (LE) and late bed–late rise (LL). The four categories were compared for body mass index (BMI) z-score, energy intake and diet quality assessed using the Dietary Guideline Index for Children and Adolescents. Analyses were adjusted for survey design, sociodemographic characteristics, sleep duration and physical activity level (PAL).
Results:
In adjusted multivariate regression models with sleep timing behaviour group as the independent variable, the ‘LL’ category compared with the ‘EE’ category had a higher BMI z-score (β=0.20, 95% confidence interval (CI) 0.06 to 0.34, P=0.007), and lower diet quality (β=−4.0, 95% CI −5.7 to −2.3, P<0.001). Children and adolescents who went to bed late also had a higher intake of extra foods (that is, energy-dense, nutrient-poor foods) while those whom went to bed early consumed more fruit and vegetables. Energy intake was associated with sleep duration (β=−4.5 kJ, 95% CI −6.7 to −2.4, P<0.001), but not sleep timing behaviour.
Conclusion:
Late bedtimes and late wake up times are associated with poorer diet quality, independent of sleep duration, PAL and child and sociodemographic characteristics.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Patel S, Hu F . Short sleep duration and weight gain: a systematic review. Obesity 2008; 16: 643–653.
Cappuccio F, Taggart F, Kandala N, Currie A, Stranges S, Miller M . Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008; 31: 619–626.
Eisenmann J, Ekkekakis P, Holmes M . Sleep duration and overweight among Australian children and adolescents. Acta Paediatr 2006; 95: 956–963.
Knutson KL . Sex differences in the association between sleep and body mass index in adolescents. J Pediatr 2005; 147: 830–834.
Olds T, Blunden S, Dollman J, Maher C . Day type and the relationship between weight status and sleep duration in children and adolescents. Aust NZJ Public Health 2010; 34: 165–171.
Snell E, Adam E, Duncan G . Sleep and the body mass index and overweight status of children and adolescents. Child Dev 2007; 78: 309–323.
Lumeng J, Somashekar D, Appugliese D, Kaciroti N, Corwyn R, Bradley R . Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 2007; 120: 1020–1029.
Marshall NGN, Grunstein R . Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev 2008; 12: 289–298.
Spiegel K, Leproult R, L’hermite-Balériaux M, Copinschi G, Penev P, Van Cauter E . Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab 2004; 89: 5762–5771.
Spiegel K, Leproult R, Van Cauter E . Impact of sleep debt on metabolic and endocrine function. Lancet 1999; 354: 1435–1439.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141: 846–850.
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD . Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr 2009; 89: 126–133.
Shi Z, McEvoy M, Luu J, Attia J . Dietary fat and sleep duration in Chinese men and women. Int J Obes 2008; 32: 1835–1840.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Iever-Landis C, Redline S . The association of sleep duration with adolescents' fat and carbohydrate consumption. Sleep 2010; 33: 1201–1209.
Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B . A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res 2008; 17: 331–334.
Omisade A, Buxton OM, Rusak B . Impact of acute sleep restriction on cortisol and leptin levels in young women. Physiol Behav 2010; 99: 651–656.
von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B . Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep—a cross-sectional study. Int J Obes 2002; 26: 710–716.
Hitze B, Bosy-Westphal A, Bielfeldt F, Settler U, Plachta-Danielzik S, Pfeuffer M et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr 2009; 63: 739–746.
Fleig D, Randler C . Association between chronotype and diet in adolescents based on food logs. Eat Behav 2009; 10: 115–118.
Horne J . Short sleep is a questionable risk factor for obesity and related disorders: statistical versus clinical significance. Biol Psychol 2008; 77: 266–276.
Horne J . Too weighty a link between short sleep and obesity? Sleep 2008; 31: 595–596.
Calamaro C, Park S, Mason T, Marcus C, Weaver T, Pack A et al. Shortened sleep duration does not predict obesity in adolescents. J Sleep Res 2010; 19: 559–566.
Kathrotia R, Rao P, Paralikar S, Shah C, Oommen E . Late sleeping affects sleep duration and body mass index in adolescents. Iranian J Med Sci 2010; 35: 57–60.
Touchette E, Mongrain V, Petit D, Tremblay R, Montplaisir J . Development of sleep-wake schedules during childhood and relationship with sleep duration. Arch Pediatr Adolesc Med 2008; 162: 343–349.
Olds T, Maher C, Matricciani L . Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep 2011; 34: 1299–1307.
Gaina A, Sekine M, Kanayama H, Takashi Y, Hu L, Sengoku K et al. Morning-Evening preference: sleep pattern spectrum and lifestyle habits among Japanese junior high school pupils. Chronobiol Int 2006; 23: 607–621.
Schubert E, Randler C . Association between chronotype and the constructs of the Three-Factor-Eating-Questionnaire. Appetite 2008; 51: 501–505.
Baron K, Reid K, Kern A, Zee P . Role of sleep timing in caloric intake and BMI. Obesity 2011; 19: 1374–1381.
DoHA. User Guide 2007Australian National Children’s Nutrition and Physical Activity Survey In Canberra, 2010.
Ridley K, Olds TS, Hill A . The Multimedia Activity Recall for Children and Adolescents (MARCA): development and evaluation. Int J Behav Nutr Phys Act 2006; 3, Epub 26 May.
Olds T, Ridley K, Dollman JM, Maher CA . The validity of a computerized use of time recall, the Multimedia Activity Recall for Children and Adolescents. Pediatr Exerc Sci 2010; 22: 34–43.
Johnson RK, Driscoll P, Goran ML . Comparison of multiple-pass 24-hour recall estimatesof energy intake with total energy expenditure determined by the doubly labeled water method in children. J Am Diet Assoc 1996; 96: 1140–1144.
FSANZ. AUSNUT 2007—Australian Food, Supplement and Nutrient Database for Estimation of Population Nutrient Intakes. Date accessed 17th November 2010. In: Canberra 2008.
Smith A, Kellett E, Schmerlaib Y . The Australian Guide to Healthy Eating. Common wealth Department of Health and Family Services: Canberra, 1998.
Marfell-Jones M, Olds T, Stewart A, Carter L . International Standards for Anthropometric Assessment. North-West University: Potchefstroom, RSA, 2006.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Cole TJ, Freeman JV, Preece MA . Body mass index reference curves for the UK, 1990. Arch Dis Child 1995; 73: 25–29.
Golley RK, Hendrie GA, Mc Naughton SA . Scores on the dietary guideline index for children and adolescents are associated with nutrient intake and socio-economic position but not adiposity. J Nutr 2011; 141: 1340–1347.
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 1991; 45: 659–581.
Black AE . Critical evaluation of energy intake using the Goldberg cut-off for energy intake: basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes 2000; 24: 1119–1130.
Nishitani N, Sakakibara H, Akiyama I . Characteristics of short sleeping time and eating behaviors related to obesity. Obes Res Clin Pract 2012; 6 (2): e103–e109.
Nishiura C, Noguchi J, Hashimoto H . Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep 2010; 33: 753–757.
Albertson AM, Anderson GH, Crockett SJ, Goebel MT . Ready-to-eat cereal consumption: its relationship with BMI and nutrient intake of children aged 4 to 12 years. J Am Diet Assoc 2003; 103: 1613–1619.
Gibson SA, O’Sullivan KR . Breakfast cereal consumption patterns and nutrient intakes of British schoolchildren. J R Soc Health 1995; 115: 366–370.
Cho S, Dietrich M, Brown CJ, Clark CA, Block G . The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003; 22: 296–302.
Wolfe WS, Campbell CC, Frongillo E, Haas JD, Melnik T . Overweight schoolchildren in New York State: prevalence and characteristics. Am J Public Health 1994; 84: 807–813.
de Castro JM . The time of day of food intake influences overall intake in humans. J Nutr 2004; 134: 104–111.
de Castro JM . The time of day and the proportions of macronutrients eaten are related to total daily food intake. Br J Nutr 2007; 98: 1077–1083.
Lehto R, Ray C, Lahti-Koski M, Roos E . Meal pattern and BMI in 9-11-year-old children in Finland. Public Health Nutr 2010; 14: 1245–1250.
Taheri S, Lin L, Austin D, Young T, Mignot E . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. Plos Med 2004; 1: e62.
Ridley K . The Multimedia Activity Recall for Children and Adolescents (MARCA): Development and Validation. PhD, University of South Australia: Adelaide, 2005.
Magarey A, Watson J, Golley RK, Burrows T, Sutherland R, Mc Naughton SA et al. Assessing dietary intake in children and adolescents: considerations and recommendations for obesity research. Int J Pediatr Obes 2011; 6: 2–11.
Trost SG, Morgan A, Saunders R, Felton G, Ward D, Pate R . Children’s understanding of the concept of physical activity. Pediatr Exerc Sci 2000; 12: 293–299.
Carskadon MA, Acebo C, Jenni OG . Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci 2004; 1021: 276–291.
Salmon J, Campbell K, Crawford D . Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust 2006; 184: 64–67.
Lewis M, Hill A . Food advertising on British children’s television: a content analysis and experimental study with nine-year olds. Int J Obes Relat Metab Disord 1998; 22: 206–214.
Neville L, Thomas M, Bauman A . Food advertising on Australian television: the extent of children’s exposure. Health Promot Int 2005; 20: 105–112.
Stitt C, Kunkel D . Food advertising during children’s television programming on broadcast and cable channels. Health Commun 2008; 23: 573–584.
Acknowledgements
RKG was supported by a National Health and Medical Research Council Public Health Postdoctoral Fellowship (478115). CAM is supported by an Australian Research Council Postdoctoral Fellowship. The collection of data used in study was supported by the Australian Commonwealth Department of Health and Ageing; the Department of Agriculture, Fisheries and Forestry; and by the Australian Food and Grocery Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Golley, R., Maher, C., Matricciani, L. et al. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes 37, 546–551 (2013). https://doi.org/10.1038/ijo.2012.212
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.212
Keywords
This article is cited by
-
Obesity Heterogeneity by Neighborhood Context in a Largely Latinx Sample
Journal of Racial and Ethnic Health Disparities (2024)
-
Shorter sleep among adolescents is associated with lower fruit and vegetable consumption the following day
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
Is chronotype linked with adherence to the Mediterranean diet among adolescents? The EHDLA study
Pediatric Research (2023)
-
Efficacy of hydrotherapy, spa therapy, and balneotherapy on sleep quality: a systematic review
International Journal of Biometeorology (2023)
-
Impact of the COVID-19 pandemic on children’s sleep habits: an ECHO study
Pediatric Research (2023)