Abstract
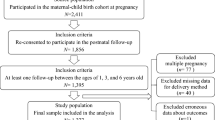
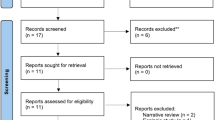
Studies have reported inconsistent results concerning the association of cesarean section with offspring obesity. We performed a systematic review and meta-analysis to examine whether cesarean section increases the risk of later overweight and obesity. Pubmed, Embase and Web of Science were searched using different combinations of two groups of keywords: ‘cesarean’ and ‘overweight/obesity’. Cohort or case–control studies that reported the association of cesarean section with childhood (3–8 years), adolescence (9–18 years) and/or adult (>19 years) overweight/obesity were eligible. Where possible, adjusted risk estimates were pooled using a random effects model; otherwise unadjusted estimates were pooled. Statistical heterogeneity was assessed with I2 statistics; the values of 25%, 50% and 75% were considered to indicate low, medium and high heterogeneity, respectively. We conducted a subgroup analysis to identify the sources of heterogeneity according to study quality defined on the basis of the Newcastle-Ottawa Scale. In total, two case–control and seven cohort studies were identified for the literature review and 15 separate risk estimates were included in the meta-analysis. The overall pooled odds ratio (OR) of overweight/obesity for offspring delivered by cesarean section compared with those born vaginally was 1.33 (95% confidence interval (CI) 1.19, 1.48; I2=63%); the OR was 1.32 (1.15, 1.51) for children, 1.24 (1.00, 1.54) for adolescents and 1.50 (1.02, 2.20) for adults. In subgroup analysis, the overall pooled OR was 1.18 (1.09, 1.27; I2=29%) for high-quality studies and 1.78 (1.43, 2.22; I2=24%) for medium-quality (P for interaction=0.0005); no low-quality studies were identified. The ORs for children, adolescents and adults all tended to be lower for high-quality studies compared with medium-quality studies. Our results indicated that cesarean section was moderately associated with offspring overweight and obesity. This finding has public health implications, given the increase in cesarean births in many countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hyde MJ, Mostyn A, Modi N, Kemp PR . The health implications of birth by caesarean section. Biol Rev Camb Philos Soc 2012; 87: 229–243.
Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F . Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol 2012; 206: 331 e331-331.e319.
World Health Organization. Appropriate technology for birth. Lancet 1985; 2: 436–437.
Zhang J, Liu Y, Meikle S, Zheng J, Sun W, Li Z . Cesarean delivery on maternal request in southeast China. Obstet Gynecol 2008; 111: 1077–1082.
Neu J, Rushing J . Cesarean versus vaginal delivery: long-term infant outcomes and the hygiene hypothesis. Clin Perinatol 2011; 38: 321–331.
Nicholson JK, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W et al. Host-gut microbiota metabolic interactions. Science 2012; 336: 1262–1267.
Thavagnanam S, Fleming J, Bromley A, Shields MD, Cardwell CR . A meta-analysis of the association between Caesarean section and childhood asthma. Clin Exp Allergy 2008; 38: 629–633.
Bager P, Wohlfahrt J, Westergaard T . Caesarean delivery and risk of atopy and allergic disease: meta-analyses. Clin Exp Allergy 2008; 38: 634–642.
Cardwell CR, Stene LC, Joner G, Cinek O, Svensson J, Goldacre MJ et al. Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: a meta-analysis of observational studies. Diabetologia 2008; 51: 726–735.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI . An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006; 444: 1027–1031.
Flintoft L . Human microbiome: a gut feeling for disease. Nat Rev Genet 2010; 11: 237–237.
Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 2004; 101: 15718–15723.
Manco M, Putignani L, Bottazzo GF . Gut microbiota, lipopolysaccharides, and innate immunity in the pathogenesis of obesity and cardiovascular risk. Endocr Rev 2010; 31: 817–844.
Ajslev TA, Andersen CS, Gamborg M, Sorensen TI, Jess T . Childhood overweight after establishment of the gut microbiota: the role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes (Lond) 2011; 35: 522–529.
Barros FC, Matijasevich A, Hallal PC, Horta BL, Barros AJ, Menezes AB et al. Cesarean section and risk of obesity in childhood, adolescence, and early adulthood: evidence from 3 Brazilian birth cohorts. Am J Clin Nutr 2012; 95: 465–470.
Goldani HA, Bettiol H, Barbieri MA, Silva AA, Agranonik M, Morais MB et al. Cesarean delivery is associated with an increased risk of obesity in adulthood in a Brazilian birth cohort study. Am J Clin Nutr 2011; 93: 1344–1347.
Huh SY, Rifas-Shiman SL, Zera CA, Edwards JW, Oken E, Weiss ST et al. Delivery by caesarean section and risk of obesity in preschool age children: a prospective cohort study. Arch Dis Child 2012; 97: 610–616.
Li H . A national epidemiological survey on obesity of children under 7 years of age in nine cities of China, 2006. Zhonghua Er Ke Za Zhi 2008; 46: 174–178.
Rooney BL, Mathiason MA, Schauberger CW . Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern Child Health J 2011; 15: 1166–1175.
Steur M, Smit HA, Schipper CMA, Scholtens S, Kerkhof M, De Jongste JC et al. Predicting the risk of newborn children to become overweight later in childhood: the PIAMA birth cohort study. Int J Pediatr Obes 2011; 6: e170–e178.
Zhou L, He G, Zhang J, Xie R, Walker M, Wen SW . Risk factors of obesity in preschool children in an urban area in China. Eur J Pediatr 2011; 170: 1401–1406.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283: 2008–2012.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et alThe Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (accessed 1 May 2012, at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp).
Higgins JP, Thompson SG, Deeks JJ, Altman DG . Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560.
Higgins JP, Green S Cochrane Handbook for Systematic Reviews of Interventions (accessed 1 May 2012, at http://www.cochrane-handbook.org/).
Multiple Outcomes or Time-Points within a Study. In: Borenstein M, Hedges LV, Higgins JPT, Rothstein HR . Introduction to Meta-Analysis. John Wiley & Sons, Ltd: Chichester, West Sussex, UK, 2009. pp 225–238.
Begg CB, Mazumdar M . Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Viechtbauer W . Conducting meta-analyses in R with the metafor package. J Stat Softw 2010; 36: 1–48.
Li HT, Ye RW, Pei LJ, Ren A, Zheng XY, Liu JM . Cesarean delivery, cesarean delivery on maternal request and childhood overweight: a Chinese birth cohort study of 181 380 children. Unpublished study.
Gronlund MM, Lehtonen OP, Eerola E, Kero P . Fecal microflora in healthy infants born by different methods of delivery: permanent changes in intestinal flora after cesarean delivery. J Pediatr Gastroenterol Nutr 1999; 28: 19–25.
Kalliomaki M, Collado MC, Salminen S, Isolauri E . Early differences in fecal microbiota composition in children may predict overweight. Am J Clin Nutr 2008; 87: 534–538.
Li HT, Zhou YB, Liu JM . Cesarean section might moderately increase offspring obesity risk. Am J Clin Nutr 2012; 96: 215–216.
Yoshimitsu N, Douchi T, Kamio M, Nagata Y . Differences in umbilical venous and arterial leptin levels by mode of delivery. Obstet Gynecol 2000; 96: 342–345.
Zanardo V, Svegliado G, Cavallin F, Giustardi A, Cosmi E, Litta P et al. Elective cesarean delivery: does it have a negative effect on breastfeeding? Birth 2010; 37: 275–279.
Armstrong J, Reilly JJ . Breastfeeding and lowering the risk of childhood obesity. Lancet 2002; 359: 2003–2004.
Mantzoros CS, Rifas-Shiman SL, Williams CJ, Fargnoli JL, Kelesidis T, Gillman MW . Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics 2009; 123: 682–689.
World Health Organization. Media center: Obesity and overweight (accessed 11 July 2012, at http://www.who.int/mediacentre/factsheets/fs311/en/index.html).
Acknowledgements
We thank Dr Mary K Serdula and Ji Liu for their review and editing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Li, Ht., Zhou, Yb. & Liu, Jm. The impact of cesarean section on offspring overweight and obesity: a systematic review and meta-analysis. Int J Obes 37, 893–899 (2013). https://doi.org/10.1038/ijo.2012.195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.195
Keywords
This article is cited by
-
Impact of cesarean section on metabolic syndrome components in offspring rats
Pediatric Research (2024)
-
Association between Cesarean section and neurodevelopmental disorders in a Japanese birth cohort: the Japan Environment and Children’s Study
BMC Pediatrics (2023)
-
Three Gorges Dam: the changing trend of snail density in the Yangtze River basin between 1990 and 2019
Infectious Diseases of Poverty (2023)
-
Caesarean section and childhood obesity at age 3 years derived from the Japan Environment and Children’s Study
Scientific Reports (2023)
-
Evaluating the association between caesarean delivery and weight status in early childhood in a Japanese birth cohort study
Scientific Reports (2023)