Abstract
OBJECTIVE:
To examine the relationship between short sleep duration and body mass index (BMI), waist circumference (WC), visceral fat area (VFA) and subcutaneous fat area (SFA) among a working population in Japan.
DESIGN:
Health-center-based, cross-sectional study.
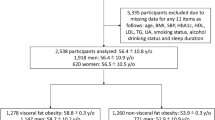
SUBJECTS:
The study subjects included 5400 men and 642 women aged 30 to 75 years who underwent an abdominal computed tomography (CT) scanning examination in a comprehensive health checkup.
MEASUREMENTS:
Height and weight were measured, and BMI was calculated. WC, VFA and SFA were measured using a CT scanner. Sleep duration was self-reported. Analysis of covariance was used to estimate adjusted means of BMI, WC, VFA and SFA across categories of sleep duration with adjustments for potential confounders. Trend of the association was assessed using multiple linear regression analysis.
RESULTS:
In men, the mean values of BMI, WC and SFA decreased with increasing sleep duration after adjustment for age, physical activity, smoking and drinking (P-value for trend <0.001). Additional adjustment for physical illnesses did not attenuate the explanatory power of the models (P-value for trend <0.001). In addition, the association between sleep duration and SFA did not change after controlling for VFA (P-value for trend <0.001). The mean values of SFA for subjects sleeping ‘<5 h’, ‘5 to <6 h’, ‘6 to <7 h’ and ‘⩾7 h’ per day were 145.8±67.4 cm2, 138.7±61.5 cm2, 134.7±60.4 cm2 and 132.5±49.2 cm2, respectively. Sleep duration was not appreciably associated with VFA. In women, no significant association was detected in any models.
CONCLUSION:
Shorter sleep duration is associated with higher BMI, WC and SFA in men. Further research is needed to explicate the biological mechanisms behind these relationships and to see whether interventions addressing inadequate sleep could treat or prevent obesity by taking gender differences into consideration.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic. Report on a WHO Consultation on Obesity, Geneva, 2000.
Nielsen LS, Danielsen KV, Sorensen TIA . Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev 2011; 12: 78–92.
Keith SW, Redden DT, Katzmarzyk PT, Boggiano MM, Hanlon EC, Benca RM et al. Putative contributors to the secular increase in obesity: exploring the roads less travelled. Int J Obes 2006; 30: 1585–1594.
Ministry of Health, Labor, and Welfare.. The National Health and Nutrition Survey in Japan. Ministry of Health, Labor, and Welfare, 2006.
NHK Broadcasting Culture Research Institute. Nihonjin no seikatsu jikan 2005: NHK kokumin seikatsu jikan chosa (Japanese Time Use 2005: The NHK National Time Use Survey). NHK Broadcasting Culture Research Institute, 2006.
Kohyama J . Sleep, serotonin, and suicide in Japan. J Phys Anthropol 2011; 30: 1–8.
Cappuccio FP, Taggart FM, Kandala N-B, Currie A, Peile E, Stranges S et al. Meta-analysis of short sleep duration and obesity in children, adolescents, and adults. Sleep 2008; 31: 619–626.
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA . Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010; 33: 585–592.
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA . Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010; 33: 414–420.
Gangwisch JE, Heymsfield SB, Bolden-Albala B, Buijs RM, Kreier F, Pickering TG et al. Short sleep duration as a risk factor for hypertension: analysis of the first National Health and Nutrition Examination Survey. Hypertension 2006; 47: 833–839.
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA . Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011; 32: 1484–1492.
Marshall NS, Glozier N, Grunstein RR . Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev 2008; 12: 289–298.
Knutson KL, Turek FW . The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep 2006; 29: 878–879.
Youngstedt SD, Kripke DF . Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev 2004; 8: 159–174.
Taheri S . Sleep and metabolism: bringing pieces of the jigsaw together. Sleep Med Rev 2007; 11: 159–162.
Patel SR, Hu FB . Short sleep duration and weight gain: a systematic review. Obesity 2008; 16: 643–653.
Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y et al. Sleep duration and mortality in Japan: the Joshi Medical School Cohort Study. J Epidemiol 2004; 14: 124–128.
Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hully SB, Sydney S et al. Objective measured sleep characteristics among early-middle-aged adults. The CARDIA Study. Am J Epidemiol 2006; 164: 5–16.
Watanabe M, Kikuchi H, Tanaka K, Takahashi M . Association of short sleep duration with weight gain and obesity at 1-year follow-up: a large-scale prospective study. Sleep 2010; 33: 161–167.
Lopez-Garzia E, Faubel R, Leon-Munoz L, Zuluaga MC, Banegas JR, Rodrigez-Artalejo F . Sleep duration, general and abdominal obesity, and weight change among the older adults population of Spain. Am J Clin Nutr 2008; 87: 310–316.
Thomas A, Schüssler MN, Fischer JE, Terris DD . Employees’ sleep duration and body mass index: potential confounders. Prev Med 2009; 48: 467–470.
International Diabetes Federation. A new worldwide definition of the metabolic syndrome [online article]. International Diabetes Federation 2006. http://www.idf.org/metabolic-syndrome (Accessed 12 April 2011).
Matsushita Y, Nakagawa T, Yamamoto S, Takahashi Y, Yokohama T, Noda M et al. Associations of visceral and subcutaneous fat area with the prevalence of metabolic risk factor clustering in 6292 Japanese individuals. Diabetes Care 2010; 33: 2117–2119.
Matsushita Y, Nakagawa T, Yamamoto S, Takahashi Y, Noda M, Mizoue T . Associations of smoking cessation with visceral fat area and prevalence of metabolic syndrome in men: the Hitachi Health Study. Obesity 2011; 19: 647–651.
Yamamoto S, Nakagawa T, Matsushita Y, Kusano S, Hayashi T, Irokawa M et al. Visceral fat area and markers of insulin resistance in relation to colorectal neoplasia. Diabetes Care 2010; 33: 184–189.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163.
Genta PR, Lorenzi-Filho G . Sleep apnea in Asians and Caucasians: comparing apples and oranges. Eur Respir J 2011; 37: 1537–1538.
Littman AJ, Vitiello MV, Foster-Schubert K, Ulrich CM, Tworoger SS, Potter JD et al. Sleep, ghrelin, leptin, and changes in body weight during a 1-year moderate-intensity physical activity intervention. Int J Obes 2007; 31: 466–475.
Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep 2004; 27: 661–666.
Van Cauter E, Spiegel K, Tasali E, Leproult R . Metabolic consequences of sleep and sleep loss. Sleep Med 2008; 9 (Suppl 1): S23–S28.
Sivak M . Sleeping more as a way to lose weight. Obes Rev 2006; 7: 295–296.
Stamatakis KA, Brownson RC . Sleep duration and obesity-related risk factors in rural Midwest. Prev Med 2008; 46: 439–444.
Miller MA, Cappuccio FP . Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol 2007; 5: 93–102.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB . Association between reduced sleep and weight gain in women. Am J Epidemiol 2006; 164: 947–954.
Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hiller TA et al. The association between sleep duration and obesity in older adults. Int J Obes 2008; 32: 1825–1834.
Pillar G, Shehadeh N . Abnormal fat and apnea: the chicken or the egg? Diabetes Care 2008; 31 (Suppl 2): S303–S309.
Li KK, Powell NB, Kushida C . Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope 2000; 100: 1937–1940.
Acknowledgements
Financial support for this study was provided by a grant from the Ministry of Health, Labor, and Welfare of Japan. We are grateful to the study participants for their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yi, S., Nakagawa, T., Yamamoto, S. et al. Short sleep duration in association with CT-scanned abdominal fat areas: the Hitachi Health Study. Int J Obes 37, 129–134 (2013). https://doi.org/10.1038/ijo.2012.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.17
Keywords
This article is cited by
-
Gender differences in the association between sleep duration and body mass index, percentage of body fat and visceral fat area among chinese adults: a cross-sectional study
BMC Endocrine Disorders (2021)
-
Acute sleep deprivation delays the glucagon-like peptide 1 peak response to breakfast in healthy men
Nutrition & Diabetes (2013)