Abstract
BACKGROUND:
Nonalcoholic fatty liver disease is a common finding in obese subjects. Increasing evidence has been provided suggesting that it represents the hepatic component of the metabolic syndrome.
OBJECTIVE:
Aim of this longitudinal study was to evaluate the relationships between several anthropometric measures, including the hepatic left lobe volume (HLLV), and various indicators of the metabolic syndrome in a cohort of severely obese women before and after laparoscopic adjustable gastric banding (LAGB).
STUDY DESIGN AND RESULTS:
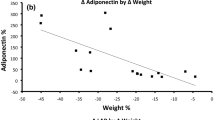
Seventy-five obese women (mean age 45±10 years and body mass index (BMI) 42.5±4.8 kg m−2) underwent LAGB and completed an average (±s.d.) post-surgical follow-up of 24±6 months. Determination of HLLV, subcutaneous and intra-abdominal fat (IAF) was based on ultrasound. The principal component statistical analysis applied to pre-operative measurements, highlighted HLLV as a parameter that clustered with serum insulin, IAF, serum glucose and uric acid, along with triglycerides (TGs), alkaline phosphatase and high-density lipoprotein cholesterol. After LAGB, the average reduction of BMI was 23%, 12% for subcutaneous fat (SCF), 42% for HLLV and 40% for visceral fat. Among body weight, BMI, SCF, IAF and HLLV, reduction of the latter was an independent predictor of reduction of serum transaminases and γ-Glutamyltransferase, glucose, insulin and TGs.
CONCLUSIONS:
In severely obese women: (i) HLLV is a sensitive indicator of ectopic fat deposition, clustering with parameters defining the metabolic syndrome; (ii) weight loss achieved by LAGB is associated with a reduction of liver volume as estimated by HLLV; (iii) among various anthropometric parameters measured, reduction of HLLV that follows LAGB represents the best single predictor of improvement of various cardiometabolic risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wajchenberg BL . Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 2000; 21: 697–738.
Eckel RH, Grundy SM, Zimmet PZ . The metabolic syndrome. Lancet 2005; 365: 1415–1428.
Kahn R, Buse J, Ferrannini E, Stern M . The metabolic syndrome: time for a critical appraisal. Joint statement from the American Diabetes Association and the European Association for the study of diabetes. Diabetologia 2005; 48: 1684–1699.
Flegal KM, Carroll MD, Ogden CL, Curtin LR . Prevalence and trends in obesity among US adults, 1999–2008. JAMA 2010; 303: 235–241.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 2001; 50: 1844–1850.
Angulo P . Nonalcoholic fatty liver disease. N Engl J Med 2002; 346: 1221–1231.
Despres JP, Lemieux I . Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881–887.
Brunt EM, Tiniakos DG . Histopathology of nonalcoholic fatty liver disease. World J Gastroenterol 2010; 16: 5286–5296.
Caldwell S, Argo C . The natural history of non-alcoholic fatty liver disease. Dig Dis 2010; 28: 162–168.
Musso G, Gambino R, Cassader M, Pagano G . Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2010; 43: 617–649.
Neuschwander-Tetri BA, Caldwell SH . Nonalcoholic steatohepatitis: summary of an AASLD single topic conference. Hepatology 2003; 37: 1202–1219.
Hart CL, Batty GD, Morrison DS, Mitchell RJ, Smith GD . Obesity, overweight and liver disease in the Midspan prospective cohort studies. Int J Obes 2010; 34: 1051–1059.
Francque S, Verrijken A, Mertens I, Hubens G, Van Marck E, Pelckmans P et al. Visceral adiposity and insulin resistance are independent predictors of the presence of non-cirrhotic NAFLD-related portal hypertension. Int J Obes 2011; 35: 270–278.
Marceau P, Biron S, Hould FS, Marceau S, Simard S, Thung SN et al. Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab 1999; 84: 1513–1517.
Fritschy P, Robotti G, Schneekloth G, Vock P . Measurement of liver volume by ultrasound and computed tomography. J Clin Ultrasound 1983; 11: 299–303.
Busetto L, Tregnaghi A, De Marchi F, Segato G, Foletto M, Sergi G et al. Liver volume and visceral obesity in women with hepatic steatosis undergoing gastric banding. Obes Res 2002; 10: 408–411.
Santini F, Giannetti M, Mazzeo S, Fierabracci P, Scartabelli G, Marsili A et al. Ultrasonographic evaluation of liver volume and the metabolic syndrome in obese women. J Endocrinol Invest 2007; 30: 104–110.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD et al. Long-term mortality after gastric bypass surgery. New Engl J Med 2007; 357: 753–761.
Busetto L, Mirabelli D, Petroni ML, Mazza M, Favretti F, Segato G et al. Comparative long-term mortality after laparoscopic adjustable gastric banding versus nonsurgical controls. Surg Obes Relat Dis 2007; 3: 496–502; discussion 502.
Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752.
Pories WJ . Bariatric surgery: risks and rewards. J Clin Endocrinol Metab 2008; 93 (Suppl 1): S89–S96.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009; 122: 248–256 e5.
Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 2009; 361: 445–454.
Ponce J, Dixon JB . Laparoscopic adjustable gastric banding. Surg Obes Relat Dis 2005; 1: 310–316.
O’Brien PE . Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol 2010; 25: 1358–1365.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Joliffe IT . Principal Component Analysis 2nd edn, New York: Springer-Verlag, 2002. p 487.
Horn JL . A Rationale and Test for the Number of Factors in Factor Analysis. Psychometrika 1965; 30: 179–185.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364: 937–952.
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med 2008; 359: 2105–2120.
Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB . Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation 2008; 117: 1658–1667.
Salvetti G, Santini F, Versari D, Virdis A, Fierabracci P, Scartabelli G et al. Fat distribution and cardiovascular risk in obese women. Obes Metab 2008; 4: 202–207.
Dixon JB, Bhathal PS, O’Brien PE . Weight loss and non-alcoholic fatty liver disease: falls in gamma-glutamyl transferase concentrations are associated with histologic improvement. Obes Surg 2006; 16: 1278–1286.
Acknowledgements
This work was supported by: ‘Weight loss, improvement of metabolic profile and reduction of liver volume in obese women after gastric banding’ Johnson and Johnson Ethicon Endo-Surgery 2007, ‘Pathogenetic mechanisms determining the obese phenotype and influencing the response to treatment’ Ministero dell’Università e della Ricerca, Programmi di Ricerca Scientifica 2007, ‘Integrate protocols for the prevention and the treatment of obesity’ Ministero della Salute, Programmi di Ricerca Finalizzata 2006, ‘Obesità: identificazione e sperimentazione di nuove strategie per la prevenzione dell’obesità e delle sue complicanze’ Ministero del Lavoro, della Salute e delle Politiche Sociali, CCM 2008.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Giannetti, M., Piaggi, P., Ceccarini, G. et al. Hepatic left lobe volume is a sensitive index of metabolic improvement in obese women after gastric banding. Int J Obes 36, 336–341 (2012). https://doi.org/10.1038/ijo.2011.243
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.243
Keywords
This article is cited by
-
Correlations of neck circumference with body composition and cardiometabolic risk factors in Arab women
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2019)
-
Liver volume and hepatic adiposity in childhood: relations to body growth and visceral fat
International Journal of Obesity (2018)
-
Reduction in hepatic left lobe volume is a good indicator of metabolic improvement after bariatric surgery
Nature Reviews Gastroenterology & Hepatology (2012)
-
Serum Insulin-Like Growth Factor-1 Concentrations Are Reduced in Severely Obese Women and Raise After Weight Loss Induced by Laparoscopic Adjustable Gastric Banding
Obesity Surgery (2012)