Abstract
Introduction and Objectives:
The frequency of copper deficiency and clinical manifestations following roux-en-y gastric bypass (RYGB) surgery is not yet clear. Objectives were to determine the prevalence and incidence of copper deficiency in patients who have undergone RYGB.
Design and Methods:
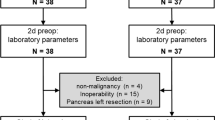
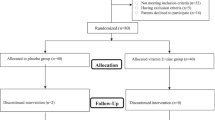
We sought to determine the number of RYGB patients undergoing medical and nutritional follow-up visits at the Emory Bariatric Center who experienced copper deficiency and associated hematological and neurological complaints (n=136). Separately, in patients followed longitudinally before and during 6 and 24 months following RYGB surgery, we obtained measures of copper status (n=16). Systemic blood cell counts and measures of copper, zinc and ceruloplasmin were determined using standardized assays in reference laboratories including atomic absorption spectrometry and immunoassays.
Results:
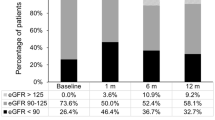
Thirteen patients were identified to have copper deficiency suggesting a prevalence of copper deficiency of 9.6%, and the majority of these had concomitant complications including anemia, leukopenia and various neuro-muscular abnormalities. In the longitudinal study, plasma copper concentrations and ceruloplasmin activity decreased over 6 and 24 months following surgery, respectively (P<0.05), but plasma zinc concentrations did not change. A simultaneous decrease in white blood cells was observed (P<0.05). The incidence of copper deficiency in these subjects was determined to be 18.8%.
Conclusions:
The prevalence and incidence of copper deficiency following RYGB surgery was determined to be 9.6% and 18.8%, respectively, with many patients experiencing mild-to-moderate symptoms. Given that copper deficiency can lead to serious and irreversible complications if untreated, frequent monitoring of the copper status of RYGB patients is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Failla ML, Johnson MA, Prohaska JR . Copper. In: Bowman BA, Russell RM (eds). Present Knowledge in Nutrition 8th ed. ILSI Press: Washington, DC, 2001, pp 373–383.
Andreini C, Banci L, Bertini I, Rosato A . Occurrence of copper proteins through the three domains of life: a bioinformatic approach. J Proteome Res 2008; 7: 209–216.
Haremaki T, Fraser ST, Kuo YM, Baron MH, Weinstein DC . Vertebrate Ctr1 coordinates morphogenesis and progenitor cell fate and regulates embryonic stem cell differentiation. Proc Natl Acad Sci USA 2007; 104: 12029–12034.
Matoba S, Kang JG, Patino WD, Wragg A, Boehm M, Gavrilova O et al. p53 regulates mitochondrial respiration. Science 2006; 312: 1650–1653.
White C, Lee J, Kambe T, Fritsche K, Petris MJ . A role for the ATP7A copper-transporting ATPase in macrophage bactericidal activity. J Biol Chem 2009; 284: 33949–33956.
Food and Nutrition Board Institute of Medicine. Dietary Reference Intakes: Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press: Washington, DC, 2001.
McClain CJ, Shedlofsky SI . Copper toxicity in Wilson's disease: an absorbing problem. J Lab Clin Med 1988; 111: 261–262.
Fields N, Craft N, Lewis C, Holbrook J, Rose A, Reiser S et al. Contrasting effects of stomach and small intestine of rats on copper absorption. J Nutr 1986; 116: 2219–2228.
Mason KE . A conspectus of research on copper metabolism and requirements of man. J Nutr 1979; 109: 1979–2066.
Atkinson RL, Dahms WT, Bray GA, Jacob R, Sandstead HH . Plasma zinc and copper in obesity and after intestinal bypass. Ann Intern Med 1978; 89: 491–493.
Faber J, Randolph JG, Robbins S, Smith JC . Zinc and copper status in young patients following jejunoileal bypass. J Surg Res 1978; 24: 83–86.
Sjostrom L, Lindroos A-K, Peltonen M, Torgerson J, Bouchard C, Carlsson B et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004; 351: 2683–2693.
Dixon JB, O’Brien PE, Playfair J, Chapman L, Schachter LM, Skinner S et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008; 299: 316–323.
Steinbrook R . Surgery for severe obesity. N Engl J Med 2004; 350: 1075–1079.
American-Society-for-Metabolic-and-Bariatric-Surgery. Fact sheet: metabolic and bariatric surgery. cited on 06 September 2010. Available from http://www.asmbs.org/Newsite07/media/asbs_presskit.htm.
DeMaria EJ, Pate V, Warthen M, Winegar DA . Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 2010; 6: 347–355.
Pories WJ . Bariatric surgery: risks and rewards. J Clin Endocrinol Metab 2008; 93: S89–S96.
Griffith DP, Liff DA, Ziegler TR, Esper GJ, Winton EF . Acquired copper deficiency: a potential serious and preventable complication following gastric bypass surgery. Obesity (Silver Spring) 2009; 17: 827–831.
Naismith RT, Shepherd JB, Weihl CC, Tutlam NT, Cross AH . Acute and bilateral blindness due to optic neuropathy associated with copper deficiency. Arch Neurol 2009; 66: 1025–1027.
Pineles SL, Wilson CA, Balcer LJ, Slater R, Galetta SL . Combined optic neuropathy and myelopathy secondary to copper deficiency. Surv Ophthalmol 2010; 55: 386–392.
Rounis E, Laing CM, Davenport A . Acute neurological presentation due to copper deficiency in a hemodialysis patient following gastric bypass surgery. Clin Nephrol 2010; 74: 389–392.
O’Donnell KB, Simmons M . Early-onset copper deficiency following roux-en-y gastric bypass. Nutr Clin Pract 2011; 26: 66–69.
Ernst B, Thurnheer M, Schultes B . Copper deficiency after gastric bypass surgery. Obesity (Silver Spring) 2009; 17: 1980–1981.
Kumar N, McEvoy KM, Ahlskog JE . Myelopathy due to copper deficiency following gastrointestinal surgery. Arch Neurol 2003; 60: 1782–1785.
Goodman BP, Bosch EP, Ross MA, Hoffman-Snyder C, Dodick DD, Smith BE . Clinical and electrodiagnostic findings in copper deficiency myeloneuropathy. J Neurol Neurosurg Psychiatry 2009; 80: 524–527.
Lin E, Gletsu N, Fugate K, McClusky D, Gu LH, Zhu J-L et al. The effects of gastric surgery on systemic ghrelin levels in the morbidly obese. Arch Surg 2004; 139: 780–784.
Lin E, Liang Z, Frediani J, Davis SS, Sweeney JF, Ziegler TR et al. Improvement in beta-cell function in patients with normal- and hyper-glycemia following roux-en-y gastric bypass surgery. Am J Physiol Endocrinol Metab 2010; 299: E706–E712.
Lin E, Armstrong-Moore D, Liang Z, Sweeney JF, Torres WE, Ziegler TR et al. Contribution of adipose tissue to plasma 25-hydroxyvitamin D concentrations during weight loss following gastric bypass surgery. Obesity (Silver Spring) 2011; 19: 588–594.
Healthcare E . Emory Medical Laboratory Services. Cited on March 31. Available from http://www.emoryhealthcare.org/medical-lab-services/index.html.
Broderius M, Mostad E, Wendroth K, Prohaska JR . Levels of plasma ceruloplasmin protein are markedly lower following dietary copper deficiency in rodents. Comp Biochem Physiol C Toxicol Pharmacol 2010; 151: 473–479.
Schosinsky KH, Lehmann HP, Beeler MF . Measurement of ceruloplasmin from its oxidase activity in serum by use of o-dianisidine dihydrochloride. Clin Chem 1974; 20: 1556–1563.
Butrimovitz GP, Purdy WC . The determination of zinc in blood plasma by atomic absorption spectrometry. Anal Chim Acta 1977; 94: 63–73.
Kumar N, Ahlskog JE, Gross Jr B . Acquired hypocupremia after gastric surgery. Clin Gastroenterol Hepatol 2004; 2: 1074–1079.
Tan JC, Burns DL, Jones HR . Severe ataxia, myelopathy, and peripheral neuropathy due to acquired copper deficiency in a patient with history of gastrectomy. J Parenter Enteral Nutr 2006; 30: 446–450.
Halfdanarson TR, Kumar N, Li CY, Phyliky RL, Hogan WJ . Hematological manifestations of copper deficiency: a retrospective review. Eur J Haematol 2008; 80: 523–531.
de Luis DA, Pacheco D, Izaola O, Terroba MC, Cuellar L, Martin T . Clinical results and nutritional consequences of bioliopancreatic diversion: three years of follow-up. Ann Nutr Metab 2008; 53: 234–239.
Twomey PJ, Wierzbicki AS, Reynolds TM, Viljoen A . The copper/caeruloplasmin ratio in routine clinical practice in different laboratories. J Clin Pathol 2009; 62: 60–63.
Xanthakos SA, Inge TH . Nutritional consequences of bariatric surgery. Curr Opin Clin Nutr Metab Care 2006; 9: 489–496.
Aasheim ET, Bjorkman S, Sovik TT, Engstrom M, Hanvold SE, Mala T et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr 2009; 90: 15–22.
Trostler N, Mann A, Zilberbush N, Avinoach E, Charuzi I . Weight loss and food Intake 18 months following vertical banded gastroplasty or gastric bypass for severe obesity. Obes Surg 1995; 5: 39–51.
Chu KU, Tsuchiya T, Ishizuka J, Uchida T, Townsend Jr CM, Thompson JC . Trophic response of gut and pancreas after ileojejunal transposition. Ann Surg 1995; 221: 249–256.
Prohaska JR . Impact of copper limitation on expression and function of multicopper oxidases (ferroxidases). Adv Nutr 2011; 2: 129–137.
Gasteyger C, Suter M, Gaillard RC, Giusti V . Nutritional deficiencies after roux-en-y gastric bypass for morbid obesity often cannot be prevented by standard multivitamin supplementation. Am J Clin Nutr 2008; 87: 1128–1133.
Olivares M, Araya M, Uauy R . Copper homeostasis in infant nutrition: deficit and excess. J Pediatr Gastroenterol Nutr 2000; 31: 102–111.
Danzeisen R, Araya M, Harrison B, Keen C, Solioz M, Thiele D et al. How reliable and robust are current biomarkers for copper status. Br J Nutr 2007; 98: 676–683.
Milne DB . Assessment of copper nutritional status. Clin Chem 1994; 40: 1479–1484.
Brolin RE, Gorman FH, Gorman RC, Petschenic AJ, Bradley LJ, Kenler HA et al. Are vitamin B12 and folate deficiency clinically important after roux-en-y gastric bypass. J Gastrointest Surg 1998; 2: 436–442.
Acknowledgements
This work was supported by National Institute of Health Grants R03 DK067167 and R21 DK 075745 (to NGM), K24 RR023356 (to TRZ), RO1 HD 39078 and a National Research Initiative Grant 2006-35200-17378 from the USDA National Institute for Food and Agriculture (to JRP), the General Clinical Research Center Grant M01 RR00039 and the Atlanta Clinical and Translational Science Institute Grant UL1 RR025008 and the International Copper Association. The authors have nothing to disclose. We graciously thank all the study participants. Adeola T Ayeni, MD assisted with clinical research coordination of the study participants and Amareshwar Chiruvella, MD assisted with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gletsu-Miller, N., Broderius, M., Frediani, J. et al. Incidence and prevalence of copper deficiency following roux-en-y gastric bypass surgery. Int J Obes 36, 328–335 (2012). https://doi.org/10.1038/ijo.2011.159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.159
Keywords
This article is cited by
-
Investigating the Prevalence of Copper and Zinc Abnormalities in Patients Pre and Post bariatric Surgery—an Australian Experience
Obesity Surgery (2023)
-
Vitamin and Mineral Deficiency 12 Years After Roux-en-Y Gastric Bypass a Cross-Sectional Multicenter Study
Obesity Surgery (2023)
-
54-jähriger Patient mit progredienter ataktischer Gangstörung
DGNeurologie (2022)
-
Copper Levels in Patients with Unexplained Dysplastic Cytopenia
Biological Trace Element Research (2021)
-
First Case Report of Acquired Copper Deficiency Following Revisional Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S) Leading to Severe Pancytopenia with Refractory Anemia
Obesity Surgery (2020)