Abstract
Objectives:
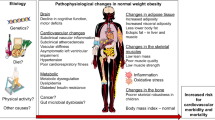
It is generally agreed that excess abdominal fat, in particular visceral abdominal fat (VAF), is related to an increased risk for obesity-related complications. We examined the association between metabolic risk factors and maintaining VAF after weight loss intervention.
Methods:
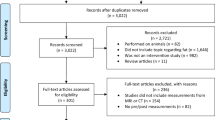
A total of 54 postmenopausal, obese women who achieved a VAF loss of at least 10% from their baseline values during a 14-week intervention were enrolled as subjects. Body weight, VAF assessed by CT scans, and metabolic risk factors (that is, blood pressure, lipids and glucose) were measured at baseline (week 0), post-intervention (week 15), and at a 2-year follow-up (week 105). The subjects were divided into two groups according to their changes in VAF between weeks 15 and 105 (follow-up period): (1) VAF gainers (VAF changes >0 cm2, n=28) or (2) VAF maintainers (VAF changes ⩽0 cm2, n=26).
Results:
The mean change in VAF of all subjects during the 14-week intervention was −34±16 cm2 (−29.7±12.3%) (P<0.01). Along with this change, improvements (P<0.05) were observed in all metabolic risk factors except for high-density lipoprotein cholesterol (HDLC). During the follow-up period, there were interactions between the two VAF groups in HDLC, triglycerides (TG) and total cholesterol (TC)/HDLC ratio (all P<0.01). In particular, the HDLC of VAF maintainers improved, and the value at week 105 exceeded baseline level (P<0.01). However, systolic and diastolic blood pressure, TC and low-density lipoprotein cholesterol in the VAF maintainers increased (all P<0.05) back to their mean baseline level despite a further decrease in their VAF during the follow-up period (P<0.01).
Conclusions:
This study shows that long-term maintenance of VAF after weight loss intervention is associated with improvements in HDLC and TG among obese, postmenopausal women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Rexrode KM, Hennekens CH, Willett WC, Colditz GA, Stampfer MJ, Rich-Edwards JW et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA 1997; 277: 1539–1545.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG et al. Obesity and the risk of heart failure. N Engl J Med 2002; 347: 305–313.
World Health Organization. Obesity: Preventing and Managing the Global Epidemic. WHO: Geneva, Switzerland, 1997.
Okura T, Tanaka K, Nakanishi T, Lee DJ, Nakata Y, Wee SW et al. Effects of obesity phenotype on coronary heart disease risk factors in response to weight loss. Obes Res 2002; 10: 757–766.
Tanaka K, Okura T, Shigematsu R, Nakata Y, Lee DJ, Wee SW et al. Target value of intraabdominal fat area for improving coronary heart disease risk factors. Obes Res 2004; 12: 695–703.
Nakata Y, Okura T, Matsuo T, Tanaka K . Factors alleviating metabolic syndrome via diet-induced weight loss with or without exercise in overweight Japanese women. Prev Med 2009; 48: 351–356.
Matsuo T, Kim MK, Murotake Y, Numao S, Kim MJ, Ohkubo H et al. Indirect lifestyle intervention through wives improves metabolic syndrome components in men. Int J Obes (London) 2010; 34: 136–145.
Weinsier RL, James LD, Darnell BE, Wooldridge NH, Birch R, Hunter GR et al. Lipid and insulin concentrations in obese postmenopausal women: separate effects of energy restriction and weight loss. Am J Clin Nutr 1992; 56: 44–49.
Kelley DE, Wing R, Buonocore C, Sturis J, Polonsky K, Fitzsimmons M . Relative effects of calorie restriction and weight loss in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1993; 77: 1287–1293.
Wing RR, Blair EH, Bononi P, Marcus MD, Watanabe R, Bergman RN . Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care 1994; 17: 30–36.
Wing RR, Hill JO . Successful weight loss maintenance. Annu Rev Nutr 2001; 21: 323–341.
Elfhag K, Rössner S . Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005; 6: 67–85.
Waki M, Heshka S, Heymsfield SB . Long-term serum lipid lowering, behavior modification, and weight loss in obese women. Nutrition 1993; 9: 23–28.
Poobalan A, Aucott L, Smith WC, Avenell A, Jung R, Broom J et al. Effects of weight loss in overweight/obese individuals and long-term lipid outcomes—a systematic review. Obes Rev 2004; 5: 43–50.
Wing RR, Blair E, Marcus M, Epstein LH, Harvey J . Year-long weight loss treatment for obese patients with type II diabetes: does including an intermittent very-low-calorie diet improve outcome? Am J Med 1994; 97: 354–362.
Wadden TA, Anderson DA, Foster GD . Two-year changes in lipids and lipoproteins associated with the maintenance of a 5–10% reduction in initial weight: some findings and some questions. Obes Res 1999; 7: 170–178.
Krebs JD, Evans S, Cooney L, Mishra GD, Fruhbeck G, Finer N et al. Changes in risk factors for cardiovascular disease with body fat loss in obese women. Diabetes Obes Metab 2002; 4: 379–387.
Leenen R, van der Kooy K, Droop A, Seidell JC, Deurenberg P, Weststrate JA et al. Visceral fat loss measured by magnetic resonance imaging in relation to changes in serum lipid levels of obese men and women. Arterioscler Thromb 1993; 13: 487–494.
Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R . Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006; 14: 336–341.
Japan Society for the Study of Obesity (JASSO). Guidelines for diagnosis and treatment in obesity and its comorbidities. The 20th Meeting, Tokyo, Japan, 1999.
Kagawa A . The four-food-group point method. J Kagawa Nutrition University 1983; 14: 5–12 (in Japanese).
Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K et al. Abdominal fat: standardized technique for measurement at CT. Radiology 1999; 211: 283–286.
Okura T, Nakata Y, Lee DJ, Ohkawara K, Tanaka K . Effects of aerobic exercise and obesity phenotype on abdominal fat reduction in response to weight loss. Int J Obes 2005; 29: 1259–1266.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Japan Science and Technology Agency. Standard Tables of Food Composition in Japan The 4th revised edn. Printing Bureau, Ministry of Finance: Tokyo, 1982 (in Japanese).
Rafamantanantsoa HH, Ebine N, Yoshioka M, Higuchi H, Yoshitake Y, Tanaka H et al. Validation of three alternative methods to measure total energy expenditure against the doubly labeled water method for older Japanese men. J Nutr Sci Vitaminol 2002; 48: 517–523.
Kumahara H, Schutz Y, Ayabe M, Yoshioka M, Yoshitake Y, Shindo M et al. The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: a validation study against whole-body indirect calorimetry. Br J Nutr 2004; 91: 235–243.
Health Promotion and Nutrition Division. Health Service Bureau, Ministry of Health and Welfare, Recommended Dietary Allowances for the Japanese, fifth revision, Dai-ichi shuppan Co Ltd.: Tokyo, 1996, pp 20–24.
Matsuo T, Okura T, Nakata Y, Yabushita N, Numao S, Sasai H et al. The influence of physical activity-induced energy expenditure on the variance in body weight change among individuals during a diet intervention. Obesity Res Clin Prac 2007; 1: 109–117.
Borg GA . Perceived exertion: a note on ‘history’ and methods. Med Sci Sports 1973; 5: 90–93.
Follick MJ, Abrams DB, Smith TW, Henderson LO, Herbert PN . Contrasting short- and long-term effects of weight loss on lipoprotein levels. Arch Intern Med 1984; 144: 1571–1574.
Wing RR, Jeffery RW . Effect of modest weight loss on changes in cardiovascular risk factors: are there differences between men and women or between weight loss and maintenance? Int J Obes Relat Metab Disord 1995; 19: 67–73.
Andersen RE, Wadden TA, Bartlett SJ, Vogt RA, Weinstock RS . Relation of weight loss to changes in serum lipids and lipoproteins in obese women. Am J Clin Nutr 1995; 62: 350–357.
Taskinen MR, Nikkilä EA . Effects of caloric restriction on lipid metabolism in man: changes of tissue lipoprotein lipase activities and of serum lipoproteins. Atherosclerosis 1979; 32: 289–299.
Stefanick ML, Terry RB, Haskell WL, Wood PD . Relationships of changes in post heparin hepatic and lipoprotein lipase activity to HDL-cholesterol changes following weight loss achieved by dieting versus exercise. In: Gallo L (ed). Cardiovascular Disease: Molecular and Cellular Mechanisms, Prevention and Treatment. Plenum Press: Washington, DC, 1987, pp 61–68.
van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJ . Waist-hip ratio is a poor predictor of changes in visceral fat. Am J Clin Nutr 1993; 57: 327–333.
Eckel RH . The importance of timing and accurate interpretation of the benefits of weight reduction on plasma lipids. Obes Res 1999; 7: 227–228.
Toth MJ, Tchernof A, Sites CK, Poehlman ET . Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes Relat Metab Disord 2000; 24: 226–231.
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 1991; 45: 569–581.
Acknowledgements
We are grateful to the participants and staff members in the study. The Sodegaura Health Promotion Project, Sodegaura, Chiba, Japan supported this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Matsuo, T., Kato, Y., Murotake, Y. et al. An increase in high-density lipoprotein cholesterol after weight loss intervention is associated with long-term maintenance of reduced visceral abdominal fat. Int J Obes 34, 1742–1751 (2010). https://doi.org/10.1038/ijo.2010.95
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.95