Abstract
Objective:
We aimed at evaluating whether the addition of low-dose metformin to dietary treatment could be an effective approach in nondiabetic patients with nonalcoholic fatty liver disease (NAFLD).
Methods:
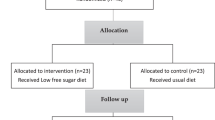
We carried out a 6-month prospective study in a series of overweight or obese patients with ultrasonographic diagnosis of hepatic steatosis. In total, 50 patients were enrolled and randomized into two groups: the first group (n=25) was given metformin (1 g per day) plus dietary treatment and the second group (n=25) was given dietary treatment alone.
Results:
At the end of the study, the proportion of patients with echographic evidence of fatty liver was reduced in both the metformin (P<0.0001) and the diet group (P=0.029). Moreover, patient body mass index and waist circumference significantly decreased in both groups (P<0.001). Fasting glucose, insulin resistance (evaluated as homeostasis model assessment of insulin resistance (HOMA-IR)) and serum adiponectin decreased in both groups, although these changes reached statistical significance only in the metformin group. In this group, HOMA-IR decreased from 3.3±1.6 to 2.4±1.2 (P=0.003), whereas it decreased from 3.2±1.6 to 2.8±1.1 (not significant, NS) in the diet group. Similarly, the proportion of patients with impaired fasting glucose declined from 35 to 5% (P=0.04) in the metformin and from 32 to 12% (NS) in the diet group. At baseline, ∼40% of patients in both groups met the diagnostic criteria of metabolic syndrome. This proportion decreased to 20% in the metformin group (P=0.008) and to 32% in the diet group (NS).
Conclusions:
In our 6-month prospective study, both low-dose metformin and dietary treatment alone ameliorated liver steatosis and metabolic derangements in patients with NAFLD. However, metformin was more effective than dietary treatment alone in normalizing several metabolic parameters in these patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bellentani S, Marino M . Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD). Ann Hepatol 2009; 8 (Suppl 1): S4–S8.
Festi D, Colecchia A, Sacco T, Bondi M, Roda E, Marchesini G . Hepatic steatosis in obese patients: clinical aspects and prognostic significance. Obes Rev 2004; 5: 27–42.
Bugianesi E, Zannoni C, Vanni E, Marzocchi R, Marchesini G . Non-alcoholic fatty liver and insulin resistance: a cause-effect relationship? Dig Liver Dis 2004; 36: 165–173.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 2001; 50: 1844–1850.
Vuppalanchi R, Chalasani N . Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: selected practical issues in their evaluation and management. Hepatology 2009; 49: 306–317.
Tsochatzis EA, Papatheodoridis GV, Archimandritis AJ . Adipokines in nonalcoholic steatohepatitis: from pathogenesis to implications in diagnosis and therapy. Mediators Inflamm 2009; 2009: 831670.
Socha P, Horvath A, Vajro P, Dziechciarz P, Dhawan A, Szajewska H . Pharmacological interventions for nonalcoholic fatty liver disease in adults and in children: a systematic review. J Pediatr Gastroenterol Nutr 2009; 48: 587–596.
Sanyal AJ, Mofrad PS, Contos MJ, Sargeant C, Luketic VA, Sterling RK et al. A pilot study of vitamin E versus vitamin E and pioglitazone for the treatment of nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2004; 2: 1107–1115.
Aithal GP, Thomas JA, Kaye PV, Lawson A, Ryder SD, Spendlove I et al. Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalcoholic steatohepatitis. Gastroenterology 2008; 135: 1176–1184.
Promrat K, Lutchman G, Uwaifo GI, Freedman RJ, Soza A, Heller T et al. A pilot study of pioglitazone treatment for nonalcoholic steatohepatitis. Hepatology 2004; 39: 188–196.
Belfort R, Harrison SA, Brown K, Darland C, Finch J, Hardies J et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med 2006; 355: 2297–2307.
Ratziu V, Giral P, Jacqueminet S, Charlotte F, Hartemann-Heurtier A, Serfaty L et al. Rosiglitazone for nonalcoholic steatohepatitis: one-year results of the randomized placebo-controlled Fatty Liver Improvement with Rosiglitazone Therapy (FLIRT) Trial. Gastroenterology 2008; 135: 100–110.
Wang CC, Huang HT . Voice aerodynamic analysis of normal Taiwanese adults. J Formos Med Assoc 2005; 104: 868–872.
Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR . Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology 2003; 38: 1008–1017.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Zoli M, Melchionda N . Metformin in non-alcoholic steatohepatitis. Lancet 2001; 358: 893–894.
Nair S, Diehl AM, Wiseman M, Farr Jr GH, Perrillo RP . Metformin in the treatment of non-alcoholic steatohepatitis: a pilot open label trial. Aliment Pharmacol Ther 2004; 20: 23–28.
Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A et al. Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2004; 19: 537–544.
Bugianesi E, Gentilcore E, Manini R, Natale S, Vanni E, Villanova N et al. A randomized controlled trial of metformin versus vitamin E or prescriptive diet in nonalcoholic fatty liver disease. Am J Gastroenterol 2005; 100: 1082–1090.
Nobili V, Manco M, Ciampalini P, Alisi A, Devito R, Bugianesi E et al. Metformin use in children with nonalcoholic fatty liver disease: an open-label, 24-month, observational pilot study. Clin Ther 2008; 30: 1168–1176.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Ascaso JF, Pardo S, Real JT, Lorente RI, Priego A, Carmena R . Diagnosing insulin resistance by simple quantitative methods in subjects with normal glucose metabolism. Diabetes Care 2003; 26: 3320–3325.
Palmentieri B, de Sio I, La Mura V, Masarone M, Vecchione R, Bruno S et al. The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig Liver Dis 2006; 38: 485–489.
Roldan-Valadez E, Favila R, Martinez-Lopez M, Uribe M, Mendez-Sanchez N . Imaging techniques for assessing hepatic fat content in nonalcoholic fatty liver disease. Ann Hepatol 2008; 7: 212–220.
National Institutes Of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report National Institutes Of Health. Obes Res 1998; 6 (Suppl 2): 51S–209S.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735–2752.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth joint task force of the European Society Of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 2007; 14 (Suppl 2): E1–E40.
Expert Panel on Detection, Evaluation, Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003; 37: 917–923.
Kotronen A, Westerbacka J, Bergholm R, Pietilainen KH, Yki-Jarvinen H . Liver fat in the metabolic syndrome. J Clin Endocrinol Metab 2007; 92: 3490–3497.
Huang MA, Greenson JK, Chao C, Anderson L, Peterman D, Jacobson J et al. One-year intense nutritional counseling results in histological improvement in patients with non-alcoholic steatohepatitis: a pilot study. Am J Gastroenterol 2005; 100: 1072–1081.
Park HS, Kim MW, Shin ES . Effect of weight control on hepatic abnormalities in obese patients with fatty liver. J Korean Med Sci 1995; 10: 414–421.
Hickman IJ, Jonsson JR, Prins JB, Ash S, Purdie DM, Clouston AD et al. Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life. Gut 2004; 53: 413–419.
Suzuki A, Lindor K, St Saver J, Lymp J, Mendes F, Muto A et al. Effect of changes on body weight and lifestyle in nonalcoholic fatty liver disease. J Hepatol 2005; 43: 1060–1066.
Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI . Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 2005; 54: 603–608.
Kirpichnikov D, McFarlane SI, Sowers JR . Metformin: an update. Ann Intern Med 2002; 137: 25–33.
Loomba R, Lutchman G, Kleiner DE, Ricks M, Feld JJ, Borg BB et al. Clinical trial: pilot study of metformin for the treatment of nonalcoholic steatohepatitis. Aliment Pharmacol Ther 2008; 29: 172–182.
He L, Sabet A, Djedjos S, Miller R, Sun X, Hussain MA et al. Metformin and insulin suppress hepatic gluconeogenesis through phosphorylation of CREB binding protein. Cell 2009; 137: 635–646.
Kohjima M, Higuchi N, Kato M, Kotoh K, Yoshimoto T, Fujino T et al. SREBP-1c, regulated by the insulin and AMPK signaling pathways, plays a role in nonalcoholic fatty liver disease. Int J Mol Med 2008; 21: 507–511.
Musso G, Gambino R, Bo S, Uberti B, Biroli G, Pagano G et al. Should nonalcoholic fatty liver disease be included in the definition of metabolic syndrome? A cross-sectional comparison with Adult Treatment Panel III criteria in nonobese nondiabetic subjects. Diabetes Care 2008; 31: 562–568.
Haukeland JW, Konopski Z, Eggesbo HB, von Volkmann HL, Raschpichler G, Bjoro K et al. Metformin in patients with non-alcoholic fatty liver disease: a randomized, controlled trial. Scand J Gastroenterol 2009; 44: 853–860.
Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology 2003; 37: 1286–1292.
Tobari M, Hashimoto E, Yatsuji S, Torii N, Shiratori K . Imaging of nonalcoholic steatohepatitis: advantages and pitfalls of ultrasonography and computed tomography. Intern Med 2009; 48: 739–746.
Lilly M, Godwin M . Treating prediabetes with metformin: systematic review and meta-analysis. Can Fam Physician 2009; 55: 363–369.
Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 2002; 8: 1288–1295.
Wieckowska A, McCullough AJ, Feldstein AE . Noninvasive diagnosis and monitoring of nonalcoholic steatohepatitis: present and future. Hepatology 2007; 46: 582–589.
Angulo P . Nonalcoholic fatty liver disease. N Engl J Med 2002; 346: 1221–1231.
Gaidos JK, Hillner BE, Sanyal AJ . A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int 2008; 28: 650–658.
Hamaguchi M, Kojima T, Takeda N, Nakagawa T, Taniguchi H, Fujii K et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med 2005; 143: 722–728.
Castera L . Non-invasive diagnosis of steatosis and fibrosis. Diabetes Metab 2008; 34: 674–679.
Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez R, McCullough AJ . Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol 2009; 51: 1061–1067.
Duseja A, Das A, Dhiman RK, Chawla YK, Thumburu KT, Bhadada S et al. Metformin is effective in achieving biochemical response in patients with nonalcoholic fatty liver disease (NAFLD) not responding to lifestyle interventions. Ann Hepatol 2007; 6: 222–226.
de Oliveira CP, Stefano JT, de Siqueira ER, Silva LS, de Campos Mazo DF, Lima VM et al. Combination of N-acetylcysteine and metformin improves histological steatosis and fibrosis in patients with non-alcoholic steatohepatitis. Hepatol Res 2008; 38: 159–165.
Idilman R, Mizrak D, Corapcioglu D, Bektas M, Doganay B, Sayki M et al. Clinical trial: insulin-sensitizing agents may reduce consequences of insulin resistance in individuals with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2008; 28: 200–208.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Garinis, G., Fruci, B., Mazza, A. et al. Metformin versus dietary treatment in nonalcoholic hepatic steatosis: a randomized study. Int J Obes 34, 1255–1264 (2010). https://doi.org/10.1038/ijo.2010.40
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.40
Keywords
This article is cited by
-
The role of anti-diabetic drugs in NAFLD. Have we found the Holy Grail? A narrative review
European Journal of Clinical Pharmacology (2024)
-
The effects of metformin on simple obesity: a meta-analysis
Endocrine (2018)
-
Liraglutide and Metformin alone or combined therapy for type 2 diabetes patients complicated with coronary artery disease
Lipids in Health and Disease (2017)
-
Metformin and metabolic diseases: a focus on hepatic aspects
Frontiers of Medicine (2015)
-
The therapy of insulin resistance in other diseases besides type 2 diabetes
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2014)