Abstract
Objectives:
Whether age or menopause per se influences fat distribution remains controversial. This study aimed to investigate the change of body composition, particularly body fat distribution, in relation to menopausal transition in a 30-month prospective study of perimenopausal women.
Methods:
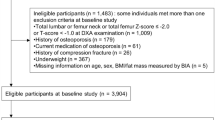
A total of 438 community-based healthy women aged 44–55 years participated in the Hong Kong Perimenopausal Women Osteoporosis Study. Data were obtained at baseline, and at 9-, 18- and 30-month during the follow-up. Soft tissue measurements consisting of fat mass and lean muscle mass of the trunk and whole body were obtained by the dual energy X-ray absorptiometry. Percentage change of body measurements over the follow-up period was compared between women who remained premenopausal, those who went through menopausal transition, and those who were menopausal since baseline.
Results:
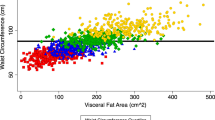
A slight decrease in the lean mass but an increase in the total fat mass and trunk fat mass (TFM) over the follow-up period were noted. Multivariate linear regression analysis showed that age was negatively associated with an increase in central obesity. Adjusted for the important predictors—age, age of menarche and education level, menopausal status was a significant and independent predictor of the decrease in lean mass and the increase in percent of body fat, TFM and trunk–leg fat mass ratio.
Conclusion:
Our 30-month longitudinal study showed that menopause has an independent effect on an increase in fat mass, and an increase in central obesity in perimenopausal Chinese women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wing RR, Matthews KA, Kuller LH, Meilahn EN, Plantinga PL . Weight gain at the time of menopause. Arch Intern Med 1991; 151: 97–102.
Tchernof A, Calles-Escandon J, Sites CK, Poehlman ET . Menopause, central body fatness, and insulin resistance: effects of hormone-replacement therapy. Coron Artery Dis 1998; 9: 503–511.
Carr MC . The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab 2003; 88: 2404–2411.
Rosano GM, Vitale C, Marazzi G, Volterrani M . Menopause and cardiovascular disease: the evidence. Climacteric 2007; 10: 19–24.
Sumino H, Ichikawa S, Yoshida A, Murakami M, Kanda T, Mizunuma H et al. Effects of hormone replacement therapy on weight, abdominal fat distribution, and lipid levels in Japanese postmenopausal women. Int J Obes Relat Metab Disord 2003; 27: 1044–1051.
Sternfeld B, Bhat AK, Wang H, Sharp T, Quesenberry Jr CP . Menopause, physical activity, and body composition/fat distribution in midlife women. Med Sci Sports Exerc 2005; 37: 1195–1202.
Ley CJ, Lees B, Stevenson JC . Sex- and menopause-associated changes in body-fat distribution. Am J Clin Nutr 1992; 55: 950–954.
Svendsen OL, Hassager C, Christiansen C . Relationships and independence of body composition, sex hormones, fat distribution and other cardiovascular risk factors in overweight postmenopausal women. Int J Obes Relat Metab Disord 1993; 17: 459–463.
Toth MJ, Tchernof A, Sites CK, Poehlman ET . Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes Relat Metab Disord 2000; 24: 226–231.
Donato GB, Fuchs SC, Oppermann K, Bastos C, Spritzer PM . Association between menopause status and central adiposity measured at different cutoffs of waist circumference and waist-to-hip ratio. Menopause 2006; 13: 280–285.
Burger HG . The menopause: when it is all over or is it? Aust N Z J Obstet Gynaecol 1994; 34: 293–295.
Wich BK, Carnes M . Menopause and the aging female reproductive system. Endocrinol Metab Clin North Am 1995; 24: 273–295.
Pansini F, Cervellati C, Guariento A, Stacchini MA, Castaldini C, Bernardi A et al. Oxidative stress, body fat composition, and endocrine status in pre- and postmenopausal women. Menopause 2008; 15: 112–118.
Koskova I, Petrasek R, Vondra K, Bláha P, Skibová J, Glagolicová A et al. Weight, body composition and fat distribution of Czech women in relation with reproductive phase: a cross-sectional study. Prague Med Rep 2007; 108: 13–26.
Teh BH, Pan WH, Chen CJ . The reallocation of body fat toward the abdomen persists to very old age, while body mass index declines after middle age in Chinese. Int J Obes Relat Metab Disord 1996; 20: 683–687.
Morita Y, Iwamoto I, Mizuma N, Kuwahata T, Matsuo T, Yoshinaga M et al. Precedence of the shift of body-fat distribution over the change in body composition after menopause. J Obstet Gynaecol Res 2006; 32: 513–516.
Troisi RJ, Wolf AM, Mason JE, Klingler KM, Colditz GA . Relation of body fat distribution to reproductive factors in pre- and postmenopausal women. Obes Res 1995; 3: 143–151.
Wang Q, Hassager C, Ravn P, Wang S, Christiansen C . Total and regional body-composition changes in early postmenopausal women: age-related or menopause-related? Am J Clin Nutr 1994; 60: 843–848.
Matthews KA, Abrams B, Crawford S, Miles T, Neer R, Powell LH et al. Body mass index in mid-life women: relative influence of menopause, hormone use, and ethnicity. Int J Obes Relat Metab Disord 2001; 25: 863–873.
Crawford SL, Casey VA, Avis NE, McKinlay SM . A longitudinal study of weight and the menopause transition: results from Massachusetts Women’s Health Study. Menopause 2000; 7: 69–70.
Bjorkelund C, Lissner L, Andersson S, Lapidus L, Bengtsson C . Reproductive history in relation to relative weight and fat distribution. Int J Obes Relat Metab Disord 1996; 20: 213–219.
Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR . Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond) 2008; 32: 949–958.
Sowers MF, Zheng H, Tomey K, Karvonen-Gutierrez C, Jannausch M, Li X et al. Changes in body composition in women over six years at midlife: ovarian and chronological aging. J Clin Endocrinol Metab 2007; 92: 895–901.
Randolph Jr JF, Sowers M, Gold EB, Mohr BA, Luborsky J, Santoro N et al. Reproductive hormones in the early menopausal transition: relationship to ethnicity, body size, and menopausal status. J Clin Endocrinol Metab 2003; 88: 1516–1522.
Ho SC, Chan SG, Yip YB, Cheng A, Yi Q, Chan C . Menopausal symptoms and symptom clustering in Chinese women. Maturitas 1999; 33: 219–227.
Ho SC, Chan SG, Yip YB, Chan CSY, Woo J, Sham A . Change in bone mineral density and its determinants in pre- and perimenopausal Chinese women: the Hong Kong perimenopausal women osteoporosis study. Osteoporos Int 2008; 19: 1785–1796.
Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN et al. Physical activity assessment methodology in the five-city project. Am J Epidemiol 1986; 121: 91–106.
Whittemore AS, Wu-Williams AH, Lee M, Zheng S, Gallagher RP, Jiao DA et al. Diet, physical activity and colorectal cancer among Chinese in North America and China. J Natl Cancer Inst 1990; 82: 915–926.
[Anonymous]. Report of a WHO scientific group. Research on the Menopause, WHO Technical Report Series 670 1981.
Ho SC, Leung PC, Swaminathan R, Chan C, Chan SG, Lindsay R . Determinants of bone mass in Chinese women aged 21–40. II Pattern of dietary calcium intake and association with bone mineral density. Osteoporosis Int 1994; 4: 167–175.
Ho SC, Chen YM, Woo JLF, Lam SSH . High habitual calcium intake attenuates bone loss in early postmenopausal Chinese women: an 18 month followup study. J Clin Endoc Metab 2004; 89: 2166–2170.
Toth MJ, Tchernof A, Sites CK, Poehlman ET . Menopause-related changes in body fat distribution. Ann N Y Acad Sci 2000; 904: 502–506.
Pietrobelli A, Formica C, Wang Z, Heymsfield SB . Dual-energy X-ray absorptiometry body composition model: review of physical concepts. Am J Physiol 1996; 271 (6 Pt 1): E941–E951.
Kohrt WM . Body composition by DXA: tried and true? Med Sci Sports Exerc 1995; 27: 1349–1353.
Kirchengast S, Gruber D, Sator M, Huber J . Impact of the age at menarche on adult body composition in healthy pre- and postmenopausal women. Am J Phys Anthropol 1998; 105: 9–20.
Feng Y, Hong X, Wilker E, Li Z, Zhang W, Jin D et al. Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis 2008; 196: 590–597.
Baglietto L, English DR, Hopper JL, MacInnis RJ, Morris HA, Tilley WD et al. Circulating steroid hormone concentrations in postmenopausal women in relation to body size and composition. Breast Cancer Res Treat 2009; 115: 171–179.
Evans DJ, Hoffmann RG, Kalkhoff RK, Kissebah AH . Relationship of androgenic activity to body fat topography, fat cell morphology, and metabolic aberrations in premenopausal women. J Clin Endocrinol Metab 1983; 57: 304–310.
Haffner SM, Katz MS, Dunn JF . Increased upper body and overall adiposity is associated with decreased sex hormone binding globulin in postmenopausal women. Int J Obes 1991; 15: 471–478.
Pasquali R . Obesity and androgens: facts and perspectives. Fertil Steril 2006; 85: 1319–1340.
Arabi A, Garnero P, Porcher R, Pelissier C, Benhamou CL, Roux C . Changes in body composition during post-menopausal hormone therapy: a 2 year prospective study. Hum Reprod 2003; 18: 1747–1752.
Norman RJ, Flight IH, Rees MC . Oestrogen and progestogen hormone replacement therapy for peri-menopausal and post-menopausal women: weight and body fat distribution. Cochrane Database Syst Rev 2000; 2: CD001018.
Boyanov MA, Shinkov AD . Effects of tibolone on body composition in postmenopausal women: a 1-year follow up study. Maturitas 2005; 51: 363–369.
Gambacciani M, Ciaponi M, Cappagli B, De Simone L, Orlandi R, Genazzani AR . Prospective evaluation of body weight and body fat distribution in early postmenopausal women with and without hormonal replacement therapy. Maturitas 2001; 39: 125–132.
Perrone G, Liu Y, Capri O, Critelli C, Barillaro F, Galoppi P et al. Evaluation of the body composition and fat distribution in long-term users of hormone replacement therapy. Gynecol Obstet Invest 1999; 48: 52–55.
Guthrie JR, Dennerstein L, Taffe JR, Ebeling PR, Randolph JF, Burger HG et al. Central abdominal fat and endogenous hormones during the menopausal transition. Fertil Steril 2003; 79: 1335–1340.
Misso ML, Jang C, Adams J, Tran J, Murata Y, Bell R et al. Differential expression of factors involved in fat metabolism with age and the menopause transition. Maturitas 2005; 51: 299–306.
Ferrara CM, Lynch NA, Nicklas BJ, Ryan AS, Berman DM . Differences in adipose tissue metabolism between postmenopausal and perimenopausal women. J Clin Endocrinol Metab 2002; 87: 4166–4170.
Price TM, O′Brien SN, Welter BH, George R, Anandjiwala J, Kilgore M . Estrogen regulation of adipose tissue lipoprotein lipase—possible mechanism of body fat distribution. Am J Obstet Gynecol 1998; 178 (1 Part 1): 101–107.
Lindberg UB, Crona N, Silfverstolpe G, Bjorntorp P, Rebuffe-Scrive M . Regional adipose tissue metabolism in postmenopausal women after treatment with exogenous sex steroids. Horm Metab Res 1990; 22: 345–351.
Kanaley JA, Sames C, Swisher L, Swick AG, Ploutz-Snyder LL, Steppan CM et al. Abdominal fat distribution in pre- and postmenopausal women: The impact of physical activity, age, and menopausal status. Metabolism 2001; 50: 976–982.
Ho SC, Woo J, Chen YM, Sham A, Lau J . Soy protein consumption and bone mass in early postmenopausal Chinese women. Osteoporos Int 2003; 14: 835–842.
Liu Z, Ho SC, Chen YM, Ho YP . A mild favorable effect of soy protein with isoflavones on body composition—a six-month double-blind randomized placebo-controlled trial. Int J Obes 2009. e-pub ahead of print 17 November 2009.
Ijuin H, Douchi T, Oki T, Maruta K, Nagata Y . The contribution of menopause to changes in body-fat distribution. J Obstet Gynaecol Res 1999; 25: 367–372.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ho, S., Wu, S., Chan, S. et al. Menopausal transition and changes of body composition: a prospective study in Chinese perimenopausal women. Int J Obes 34, 1265–1274 (2010). https://doi.org/10.1038/ijo.2010.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.33
Keywords
This article is cited by
-
A review of menopause nomenclature
Reproductive Health (2022)
-
Treating menopause — MHT and beyond
Nature Reviews Endocrinology (2022)
-
Metabolic health, menopause, and physical activity—a 4-year follow-up study
International Journal of Obesity (2022)
-
Examining negative affect, sleep duration, and using food to cope as predictors of weight in midlife women
Journal of Behavioral Medicine (2022)
-
A comparative study of orthorexia between premenopausal, perimenopausal, and postmenopausal women
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)