Abstract
Background:
Overweight is increasing in transition countries, while iron deficiency remains common. In industrialized countries, greater adiposity increases risk of iron deficiency. Higher hepcidin levels in obesity may reduce dietary iron absorption. Therefore, we investigated the association between body mass index (BMI) and iron absorption, iron status and the response to iron fortification in populations from three transition countries (Thailand, Morocco and India).
Methods:
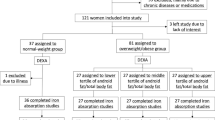
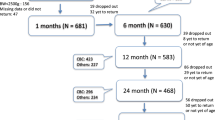
In Thai women (n=92), we examined the relationship between BMI and iron absorption from a reference meal containing ∼4 mg of isotopically labeled fortification iron. We analyzed data from baseline (n=1688) and intervention (n=727) studies in children in Morocco and India to look for associations between BMI Z-scores and baseline hemoglobin, serum ferritin and transferrin receptor, whole blood zinc protoporphyrin and body iron stores, and changes in these measures after provision of iron.
Results:
In the Thai women, 20% were iron deficient and 22% were overweight. Independent of iron status, a higher BMI Z-score was associated with decreased iron absorption (P=0.030). In the Indian and Moroccan children, 42% were iron deficient and 6.3% were overweight. A higher BMI Z-score predicted poorer iron status at baseline (P<0.001) and less improvement in iron status during the interventions (P<0.001).
Conclusions:
Adiposity in young women predicts lower iron absorption, and pediatric adiposity predicts iron deficiency and a reduced response to iron fortification. These data suggest the current surge in overweight in transition countries may impair efforts to control iron deficiency in these target groups. Interactions of the ‘double burden’ of malnutrition during the nutrition transition may have adverse consequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Popkin B . The nutrition transition: an overview of world patterns of change. Nutr Rev 2004; 62: S140–S143.
Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM . The dual burden household and the nutrition transition paradox. Int J Obesity 2005; 29: 129–136.
Kosulwat V . The nutrition and health transition in Thailand. Public Health Nutr 2002; 5: 183–189.
Benjelloun S . Nutrition transition in Morocco. Public Health Nutr 2002; 5: 135–140.
Shetty PS . Nutrition transition in India. Public Health Nutr 2002; 5: 175–182.
Kantachuvessiri A . Obesity in Thailand. J Med Assoc Thai 2005; 88: 554–562.
Zimmermann MB, Winichagoon P, Gowachirapant S, Hess SY, Harrington M, Chavasit V et al. Comparison of the efficacy of wheat-based snacks fortified with ferrous sulfate, electrolytic iron, or hydrogen-reduced elemental iron: randomized, double-blind, controlled trial in Thai women. Am J Clin Nutr 2005; 82: 1276–1282.
Aboussaleh Y, Ahami AO, Alaoui L, Delisle H . Prevalence of anemia among schoolchildren in the province of Kenitra in Morocco (in French). Sante 2004; 14: 37–42.
Moroccan Ministry of Health. Demographic and Health Survey (DHS). Enquête nationale sur la planification familiale, la fécondité et la santé de la population au Maroc. Rapport national (ENPS II). 1992.
Rguibi M, Belahsen R . Prevalence of obesity in Morocco. Obes Rev 2007; 8: 11–13.
Srihari G, Eilander A, Muthayya S, Kurpad AV, Seshadri S . Nutritional status of affluent Indian school children: what and how much do we know? Indian Pediatr 2007; 44: 204–213.
Popkin BM . An overview on the nutrition transition and its health implications: the Bellagio meeting. Public Health Nutr 2002; 5: 93–103.
Wenzel BJ, Stults HB, Mayer J . Hypoferraemia in obese adolescents. Lancet 1962; 2: 327–328.
Seltzer CC, Mayer J . Serum iron and iron-binding capacity in adolescents. Comparison of obese and nonobese subjects. Am J Clin Nutr 1963; 13: 354–361.
Scheer JC, Guthrie HA . Hemoglobin criteria with respect to obesity. Am J Clin Nutr 1981; 34: 2748–2751.
Pinhas-Hamiel O, Newfield RS, Koren I, Agmon A, Lilos P, Phillip M . Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes Relat Metab Disord 2003; 27: 416–418.
Nead KG, Halterman JS, Kaczorowski JM, Auinger P, Weitzman M . Overweight children and adolescents: a risk group for iron deficiency. Pediatrics 2004; 114: 104–108.
Brotanek JM, Gosz J, Weitzman M, Flores G . Iron deficiency in early childhood in the United States: risk factors and racial/ethnic disparities. Pediatrics 2007; 120: 568–575.
Micozzi MS, Albanes D, Stevens RG . Relation of body size and composition to clinical biochemical and hematologic indices in US men and women. Am J Clin Nutr 1989; 50: 1276–1281.
Whitfield JB, Treloar S, Zhu G, Powell LW, Martin NG . Relative importance of female-specific and non-female-specific effects on variation in iron stores between women. Br J Haematol 2003; 120: 860–866.
Rossi E, Bulsara MK, Olynyk JK, Cullen DJ, Summerville L, Powell LW . Effect of hemochromatosis genotype and lifestyle factors on iron and red cell indices in a community population. Clin Chem 2001; 47: 202–208.
Lecube A, Carrera A, Losada E, Hernandez C, Simo R, Mesa J . Iron deficiency in obese postmenopausal women. Obesity (Silver Spring) 2006; 14: 1724–1730.
Yanoff LB, Menzie CM, Denkinger B, Sebring NG, McHugh T, Remaley AT et al. Inflammation and iron deficiency in the hypoferremia of obesity. Int J Obes (Lond) 2007; 31: 1412–1419.
Chung B, Matak P, McKie AT, Sharp P . Leptin increases the expression of the iron regulatory hormone hepcidin in HuH7 human hepatoma cells. J Nutr 2007; 137: 2366–2370.
Bekri S, Gual P, Anty R, Luciani N, Dahman M, Ramesh B et al. Increased adipose tissue expression of hepcidin in severe obesity is independent from diabetes and NASH. Gastroenterology 2006; 131: 788–796.
Laftah AH, Ramesh B, Simpson RJ, Solanky N, Bahram S, Schumann K et al. Effect of hepcidin on intestinal iron absorption in mice. Blood 2004; 103: 3940–3944.
Sachdev H, Gera T, Nestel P . Effect of iron supplementation on mental and motor development in children: systematic review of randomised controlled trials. Public Health Nutr 2005; 8: 117–132.
Zimmermann MB, Hurrell RF . Nutritional iron deficiency. Lancet 2007; 370: 511–520.
Walczyk T, Tuntipopipat S, Zeder C, Sirichakwal P, Wasantwisut E, Hurrell RF . Iron absorption by human subjects from different iron fortification compounds added to Thai fish sauce. Eur J Clin Nutr 2005; 59: 668–674.
Tuntipopipat S, Judprasong K, Zeder C, Wasantwisut E, Winichagoon P, Charoenkiatkul S et al. Chili, but not turmeric, inhibits iron absorption in young women from an iron-fortified composite meal. J Nutr 2006; 136: 2970–2974.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
WHO/UNICEF/UNU. Iron Deficiency Anemia Assessment, Prevention, and Control. World Health Organization: Geneva, 2001.
Walczyk T, Davidsson L, Zavaleta N, Hurrell RF . Stable isotope labels as a tool to determine iron absorption by Peruvian school children from a breakfast meal. Fresenius J Anal Chem 1997; 359: 445–449.
Zimmermann MB, Zeder C, Chaouki N, Saad A, Torresani T, Hurrell RF . Dual fortification of salt with iodine and microencapsulated iron: a randomized, double-blind, controlled trial in Moroccan schoolchildren. Am J Clin Nutr 2003; 77: 425–432.
Zimmermann MB, Wegmueller R, Zeder C, Chaouki N, Rohner F, Saïssi M et al. Dual fortification of salt with iodine and micronized ferric pyrophosphate: a randomized, double-blind, controlled trial. Am J Clin Nutr 2004; 80: 952–959.
Moretti D, Zimmermann MB, Muthayya S, Thankachan P, Lee TC, Kurpad AV et al. Extruded rice fortified with micronized ground ferric pyrophosphate reduces iron deficiency in Indian schoolchildren: a double-blind randomized controlled trial. Am J Clin Nutr 2006; 84: 822–829.
Zimmermann MB, Molinari L, Staubli F, Hess S, Chaouki N, Adou P et al. Serum transferrin receptor and zinc protoporphyrin as indicators of iron status in African children. Am J Clin Nutr 2005; 81: 615–623.
Skikne BS, Flowers CH, Cook JD . Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 1990; 75: 1870–1876.
Cook JD, Flowers CH, Skikne BS . The quantitative assessment of body iron. Blood 2003; 101: 3359–3363.
Cook JD, Dassenko SA, Lynch SR . Assessment of the role of nonheme-iron availability in iron balance. Am J Clin Nutr 1991; 54: 717–722.
Thaikruea L, Seetamanotch W, Seetamanotch S . Appropriate cut-off level of BMI for screening in Thai adults. J Med Assoc Thai 2006; 89: 2123–2128.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660–667.
Aeberli I, Kaspar M, Zimmermann MB . Dietary intake and physical activity of normal weight and overweight 6–14 year old Swiss children. Swiss Med Wkly 2007; 137: 424–430.
Anonymous. Iron. In: Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press: Washington, DC, 2001, pp 290–393.
Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME . Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics 2001; 108: 347–353.
Nemeth E, Valore EV, Territo M, Schiller G, Lichtenstein A, Ganz T . Hepcidin, a putative mediator of anemia of inflammation, is a type II acute-phase protein. Blood 2003; 101: 2461–2463.
Knutson MD, Oukka M, Koss LM, Aydemir F, Wessling-Resnick M . Iron release from macrophages after erythrophagocytosis is up-regulated by ferroportin 1 overexpression and downregulated by hepcidin. Proc Natl Acad Sci USA 2005; 102: 1324–1328.
Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 1996; 334: 292–295.
Smith KD . Iron metabolism at the host pathogen interface: lipocalin 2 and the pathogen-associated iroA gene cluster. Int J Biochem Cell Biol 2007; 39: 1776–1780.
Wang Y, Lam KS, Kraegen EW, Sweeney G, Zhang J, Tso AW et al. Lipocalin-2 is an inflammatory marker closely associated with obesity, insulin resistance, and hyperglycemia in humans. Clin Chem 2007; 53: 34–41.
Kennedy ML, Failla ML, Smith JC . Influence of genetic obesity on tissue concentrations of zinc, copper, manganese and iron in mice. J Nutr 1986; 116: 1432–1441.
Failla ML, Kennedy ML, Chen ML . Iron metabolism in genetically obese (ob/ob) mice. J Nutr 1988; 118: 46–51.
Gillum RF . Association of serum ferritin and indices of body fat distribution and obesity in Mexican American men—the Third National Health and Nutrition Examination Survey. Int J Obes Relat Metab Disord 2001; 25: 639–645.
Acknowledgements
We thank the participating women and children, as well as the local health care staff in Thailand, Morocco and India for their assistance on the project. We thank M Andersson (Zürich, Switzerland), D Moretti (Vlaardingen, The Netherlands), T Walcyzk (Singapore), P Thankachan and A Kurpad (Bangalore, India), S Tuntipopipat (Bangkok, Thailand), and A Saad (Rabat, Morocco). MZ, CZ, SM, PW, NC did the field work, MZ wrote the first draft of the manuscript, all authors contributed to the writing and editing of the manuscript. None of the authors has a conflict of interest relating to this paper. This study was supported by the Thrasher Foundation (Salt Lake City, USA) the Micronutrient Initiative (Ottawa, Canada); the Nestlé Foundation (Lausanne, Switzerland); the Foundation for Micronutrients in Medicine (Rapperswil, Switzerland) and the Swiss Federal Institute of Technology (Zürich, Switzerland).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zimmermann, M., Zeder, C., Muthayya, S. et al. Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification. Int J Obes 32, 1098–1104 (2008). https://doi.org/10.1038/ijo.2008.43
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2008.43
Keywords
This article is cited by
-
Dysfunction of DMT1 and miR-135b in the gut-testis axis in high-fat diet male mice
Genes & Nutrition (2024)
-
The role of iron metabolism in chronic diseases related to obesity
Molecular Medicine (2022)
-
Efficacy and safety of ferric derisomaltose (FDI) compared with iron sucrose (IS) in patients with iron deficiency anemia after bariatric surgery
Obesity Surgery (2022)
-
How the cookie crumbled, and the need to strike while the iron is hot
European Journal of Clinical Nutrition (2021)
-
Socio-demographic patterning of the individual-level double burden of malnutrition in a rural population in South India: a cross-sectional study
BMC Public Health (2020)