Abstract
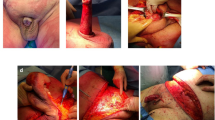
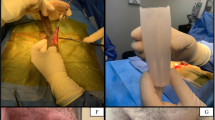
Tunica albuginea plication (TAP) surgery for Peyronie’s disease (PD) is classically described using nonabsorbable suture. Many patients are aware of nodularity at the suture sites (50–88%), and some find them painful (10–33%). We explore whether limiting permanent sutures provides a durable correction of curve and report the incidence of bothersome nodules. Beginning in 2007, we modified our TAP procedure to limit the use of permanent sutures. We reviewed all patients who underwent TAP procedures from 2007 to 2014 at our institution. Patients were contacted to complete a previously published survey regarding postoperative satisfaction. In total, 142 PD patients underwent the TAP procedure and 81/142 (57%) completed the postoperative survey. Mean office follow-up and survey follow-up were 17.3 and 56.3 months, respectively. Of the surveyed patients, 6.2% complained of a bothersome residual curve, 19.8% experienced nodularity and 4.9% reported bothersome nodules. Men with dorsal curves experienced less painful nodularity than those with ventral (P=0.047) or lateral curves (P=0.017). In total, 4/142 (2.8%) of men underwent repeat intervention. At long-term follow-up, limiting permanent sutures during TAP procedures for PD is durable with respect to curvature correction and has encouragingly low levels of nodularity and bother at suture sites.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mulhall JP, Creech SD, Boorjian SA, Ghaly S, Kim ED, Moty A et al. Subjective and objective analysis of the prevalence of peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol 2004; 171: 2350–2353.
Levine LA, Larsen SM . Surgery for Peyronie’s disease. Asian J Androl 2013; 15: 27–34.
Levine LA, Dimitriou RJ . A surgical algorithm for penile prosthesis placement in men with erectile failure and Peyronie's disease. Int J Impot Res 2000; 12: 147–151.
Levine LA, Lenting EL . A surgical algorithm for the treatment of Peyronie's disease. J Urol 1997; 158: 2149–2152.
Mulhall J, Anderson M, Parker M . A surgical algorithm for men with combined Peyronie's disease and erectile dysfunction: functional and satisfaction outcomes. J Sex Med 2005; 2: 132–138.
Papagiannopoulos D, Yura E, Levine L . Examining postoperative outcomes after employing a surgical algorithm for management of Peyronie's disease: a single-institution retrospective review. J Sex Med 2015; 12: 1474–1480.
Shefi S, Pinthus JH, Mor Y, Raviv G, Ramon J, Hanani JI . To bury the knot, then, is better than not. Urology 2008; 71: 1206–1208.
Gholami SS, Lue TF . Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002; 167: 2066–2069.
Chahal R, Gogoi N, Sundaram S, Weston P . Corporal plication for penile curvature caused by peyronie's disease: the patients' perspective. BJU Int 2001; 87: 352–356.
van der Horst C, Portillo FJM, Melchior D, Bross S, Alken P, Juenemann K . Polytetrafluoroethylene versus polypropylene sutures for essed-schroeder tunical plication. J Urol 2003; 170: 472–475.
Schultheiss D, Meschi MR, Hagemann J, Truss MC, Stief CG, Jonas U . Congenital and acquired penile deviation treated with the essed plication method. Eur Urol 2000; 38: 167–171.
Basiri A, Sarhangnejad R, Ghahestani SM, Radfar MH . Comparing absorbable and nonabsorbable sutures in corporeal plication for treatment of congenital penile curvature. Urol J 2011; 8: 302.
Iacono F, Prezioso D, Ruffo A, Illiano E, Romeo G, Amato B . Tunical plication in the management of penile curvature due la Peyronie’s disease. our experience on 47 cases. BMC Surg 2012; 12: 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on International Journal of Impotence Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Papagiannopoulos, D., Phelps, J., Yura, E. et al. Surgical outcomes from limiting the use of nonabsorbable suture in tunica albuginea plication for Peyronie’s disease. Int J Impot Res 29, 258–261 (2017). https://doi.org/10.1038/ijir.2017.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2017.34
This article is cited by
-
Plication techniques in Peyronie’s disease: new developments
International Journal of Impotence Research (2020)
-
Clinical characteristics and surgical outcomes in men undergoing tunica albuginea plication for congenital penile curvature who present with worsening penile deformity
World Journal of Urology (2020)
-
Long-term outcome after grafting with small intestinal submucosa and collagen fleece in patients with Peyronie's disease: a matched pair analysis
International Journal of Impotence Research (2019)
-
Introducing the ventral sealing technique using collagen fleece for surgical therapy of patients with ventral Peyronie’s curvature: initial experience
International Journal of Impotence Research (2018)
-
Contemporary Review of Peyronie’s Disease Treatment
Current Urology Reports (2018)